Abstract
Psychiatry research lacks an in-depth understanding of mood disorders phenotypes, leading to limited success of genetics studies of major depressive disorder (MDD). The dramatic progress in safe and affordable magnetic resonance-based imaging methods has the potential to identify subtle abnormalities of neural structures, connectivity and function in mood disordered subjects. This review paper presents strategies to improve the phenotypic definition of MDD by proposing imaging endophenotypes derived from magnetic resonance spectroscopy measures, such as cortical gamma-amino butyric acid (GABA) and glutamate/glutamine concentrations, and from measures of resting-state activity and functional connectivity. The proposed endophenotypes are discussed regarding specificity, mood state-independence, heritability, familiarity, clinical relevance and possible associations with candidate genes. By improving phenotypic definitions, the discovery of new imaging endophenotypes will increase the power of candidate gene and genome-wide associations studies. It will also help to develop and evaluate novel therapeutic treatments and enable clinicians to apply individually tailored therapeutic approaches. Finally, improvements of the phenotypic definition of MDD based on neuroimaging measures will contribute to a new classification system of mood disorders based on etiology and pathophysiology.
Similar content being viewed by others
Main
Twin and family studies have demonstrated that 31–42% of the risk factors for major depressive disorder (MDD) are genetic.1 Although there has been progress in the search for risk genes for several complex diseases,2 psychiatric conditions have turned out to be very resistant to robust gene identification. This resistance has been related to the restrictive nature of the definitions of psychiatric disorders according to ICD-10 and DSM-IV, which are not based on etiology or pathophysiolgy.3, 4
The endophenotype concept
The term ‘endophenotype’ describes an internal, intermediate phenotype that fills the gap in the causal pathway from genetic variation to the distal diseases,5 and therefore may help to resolve questions about etiology. The endophenotype concept assumes that the genetic determinants of endophenotypes, representing more elementary phenomena than psychopathological syndromes, is simpler than those involved in producing the full disease.6 The following criteria have been proposed to evaluate endophenotypes:3
-
1)
An endophenotype is associated with illness in the population.
-
2)
An endophenotype is heritable.
-
3)
An endophenotype is state-independent (manifests in an individual whether or not illness is active), but age-normed, and may need to be elicited by a challenge, for example, glucose tolerance test in relatives of diabetics.
-
4)
Within families, endophenotype and illness co-segregate.
-
5)
An endophenotype identified in probands is found in their unaffected relatives at a higher rate than in the general population.
The most important feature of a good endophenotype is its simple genetics, that is, having a less complex relationship to risk genes than the disease phenotype.7 The proof of this quality is that the association with risk genes is stronger for the endophenotype than for the disease phenotype. It is assumed that biological/molecular endophenotypes have simpler genetic determinants than higher level cognitive and psychopathological endophenotypes.3
Selection of endophenotypes
A meta-analysis has revealed that the most frequently proposed endophenotypes for schizophrenia do not meet the most important endophenotype criterion: simple genetics.8 The effect sizes of genetic loci frequently examined in psychiatric research were not larger for endophenotypes, such as N-Back performance and Wisconsin Card Sorting Task preservative errors than for traditional disease phenotypes. These findings may suggest that frequently used neuropsychological measures and behavioral experiments may not provide useful phenotypes for psychiatric genetics because there is still a long road from gene actions to neuropsychological functions. As a result, we propose that neurophysiological and molecular measures are superior over psychological measures regarding ‘simple genetics’.
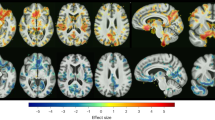
In this paper, we will focus on non-invasive measures derived from magnetic resonance imaging (MRI) because this method is safe, available and relatively inexpensive, and can therefore be applied to large samples. The selected putative endophenotypes are based on two MRI methods: (1) magnetic resonance spectroscopy (MRS) and (2) functional MRI (Figures 1 and 2). MRS provides direct measures at the molecular level that is thought to be close to gene products, while functional MRI provides individual, rather than group-averaged neuroimaging data. In addition, functional MRI is appropriate because the neural substrate of the susceptibility to MDD, in contrast to neurodevelopmental disorders, such as schizophrenia and autism, is expected to be more functional than structural in nature (with structural changes as the consequence of depression).
Heuristic model of the liability to depression. The figure displays a heuristic model of the liability to major depressive disorder (MDD). Candidate genes, modulated by epigenetic and stochastic events, predispose in an age-related manner to the development of depressive symptoms and major depressive disorder (MDD) as a response to stressful life events. Along the continuum between genes and distal phenotype lie candidate depression endophenotypes. The identification of MDD endophenotypes will be useful for studies elucidating the neurobiology and genetics of MDD, and in preclinical research, including the development of animal models of depression. This figure is not meant to be a definitive portrait of depression genes and phenotypes. It is rather an example of how functional imaging abnormalities may relate to neurochemical abnormalities and candidate genes, and to psychopathological key components of MDD. Not all functional directions are indicated for the purpose of clarity of the figure.
Resting state and stimulus-induced activity. The figure shows the different levels of resting state activity, molecular-genetic/biochemical and regional with regard to the left dorsolateral prefrontal cortex (DLPFC) and the perigenual anterior cingulate cortex (PACC). Moreover, it is displayed how that translates into abnormal stimulus-induced activity and connectivity during emotional and cognitive stimulation, as observed in many imaging studies.
Cortical GABA concentration
Neuroimaging of GABA in depression
There is increasing evidence that MDD is associated with perturbations of the metabolism of the major inhibitory neurotransmitters, gamma-amino butyric acid (GABA). Early studies reported abnormally decreased GABA concentrations in the plasma of patients with unipolar depression.9 Recent advances in proton MRS has allowed for direct, non-invasive, in vivo measurement of cerebral GABA concentrations in patients with depression. An early study on cortical GABA in depression10 applied an editing MRS protocol to assess brain GABA concentrations in the occipital lobe (this region was selected because of technical limitations), and found that GABA levels were lower in unmedicated patients with severe MDD than in healthy controls. This finding was replicated in a sample of moderately depressed patients. The reduction in the replication study was less pronounced than in the severely depressed patients of their first study, and differences found with respect to controls were largely accounted for by depressed individuals meeting criteria for the melancholic subtype.11 The first study on prefrontal GABA in depression,12 included 20 moderately depressed subjects and 20 healthy controls. Subjects were scanned on a 3 Tesla GE whole body scanner (Waukesha, WI, USA) with a transmit-receive head coil providing a homogenous radiofrequency field, and the capability to obtain spectroscopic measurements in a dorsomedial/dorsal anterolateral prefrontal region-of-interest and a ventromedial prefrontal region-of-interest. Results demonstrated that cortical GABA concentration was reduced in the dorsomedial voxel, whereas GABA levels were normal in the ventromedial voxel.
Abnormalities of the GABAergic system have been found in a wide range of psychiatric conditions. However, while the association between MDD and low cortical GABA concentration is quite consistent, the associations between cortical GABA levels and bipolar disorder13 or schizophrenia14, 15 are less apparent. Low GABA levels might also be reduced in panic disorder16, 17 and in alcohol dependence,18 possibly contributing to the considerable comorbidity among these conditions.
The literature is in disagreement regarding the mood-state independence of low cortical GABA in depression. Previous reports on an increase in occipital GABA concentrations following successful electroconvulsive therapy,19 a decreased prefrontal GABA concentrations under acute psychological stress in healthy volunteers,20 and in preclinical stress models21 suggest mood-state dependence of cortical GABA levels. Normal prefrontal GABA concentration have been found in unmedicated fully-remitted subjects with mild MDD22 and adds to the literature suggesting that low GABA concentrations is a state marker of acute depressive episodes. However, this finding may be because of the inclusion of subjects with relatively mild depressive disorders reflected by a low number of relatively short depressive episodes, low levels of functional impairments and the capacity to remain in full-remission off medication. In contrast, reduced occipital GABA concentrations have been reported in unmedicated, fully-remitted subjects with MDD,23 suggesting that low cortical GABA is associated with the underlying depressive vulnerability and not just with acute depressive symptoms. This is also suggested by the absence of correlation between depression severity and GABA measures in all previous studies. Longitudinal MRS studies are needed to address the specificity of GABA abnormalities for mood-state versus illness subtype in MDD. Lowered plasma GABA levels, as mentioned above, were specifically associated with unipolar depression.9 The abnormality in plasma GABA was not altered by antidepressant treatment24 and persisted at 4-year follow-up,25 adding to the evidence of low GABA as a trait marker in depression.
Further support for a role of GABA in MDD can be found when examining animal models of MDD. A recent translational meta-analysis26 demonstrated that in the perigenual anterior cingulate cortex (PACC), an area considered to be homologous among rats and humans, reduced concentration of GABA as well as decreased density and affinity of GABA-A receptors has been observed in various animals models of MDD. As the very same region showed hyperactivity in the resting state in both animals and humans, the animal findings can be taken to further extend the rather sparse findings in human studies. As we describe in the follow section, a further way of collecting more evidence is to investigate the concentration of GABA under functional conditions, such as stress.
Psychopathology of GABA deficit–increased stress sensitivity and negative affect
An important symptom of depression is an increased sensitivity to stress. Subjects at risk of depression are more stress sensitive than subjects without such a risk, most likely because of genetic factors.27 The depressogenic effect of stressful life events declines substantially in the course of depressive disorders,28 which is consistent with the kindling hypothesis of depression. Neurotrophic and neurotoxic processes have been proposed to account for these kindling effects. There is consistent evidence that the volume loss of the hippocampus and other brain regions is related to the duration of depression,29 suggesting that untreated depression may result in increased stress sensitivity30 and increased risk of recurrence31 because of hippocampal volume loss. Although men and women are equally sensitive to the depressogenic effects of stressful life events, their responses vary depending upon the nature of the event itself. Men are more likely to have depressive episodes following divorce, separation and work difficulties, whereas women are more sensitive to events in their proximal social network, such as difficulty getting along with an individual, serious illness, or death.32
There are various types of evidence pointing to the important role of GABA in the stress response. A recent MRS study demonstrated down-modulation of the prefrontal cortical GABA concentration under acute psychological stress induced by the threat of electric shocks. Self-reported anxiety levels significantly correlated with GABA concentrations in the medial prefrontal cortex,20 a finding consistent with experimental studies in animals. In rats, forced swimming in 25 °C water resulted in a 70% decrease of extracellular GABA concentration.33 Acute and chronic cold stress led to reductions in cortical GABA concentrations, reduced activity of the GABA-synthesizing enzyme glutamate decarboxlyse, and decreased neuronal GABA uptake in various cortical and subcortical brain regions in rats.34 Exposure of rats to chornic mild stress led to reduced hippocampal GABA concentrations determined by microdialysis.35 In addition, there is abundant evidence that stress has an impact on brain GABA receptors,36, 37, 38, 39, 40 partly mediated by stress-related alterations of neurosteroids that are active on the GABA-A receptors.41 A recent positron emission tomography study found an inverse relationship between decreased GABA-A receptor binding and hypothalamic-pituitary-adrenal (HPA) axis activity in MDD, suggesting that depression-related HPA axis hyperactivity is partly because of reduced GABAergic inhibition.42 The inverse correlation between plasma GABA levels and aggressiveness in healthy relatives of MDD patients43 suggests that GABA-related stress sensitivity is associated with the genetic risk of MDD.
Sex differences in the GABA system may account for sex differences in the human stress response. In the developing brain, estradiol's effect on the excitatory effects of GABA may significantly contribute to profound sex differences found in the brain volumes of specific nuclei.44 In the rat hypothalamus, striking sexual dimorphisms have been found in the rate of GABA turnover,45 and stress-induced changes in GABAA receptor binding at the orthosteric site were found to be sexually dimorphic.46, 47 Reduced cortical GABA concentration is likely paralleled by reduced GABAergic neuronal inhibition, possibly leading to increased glutamatergic excitotoxicity.48 This mechanism may account for reductions in gray matter volume associated with increased stress sensitivity and increased risk of recurrence of major depressive episodes.
In addition to the role of GABA in the stress response, reduced GABAergic activity has been found to be related to negative emotions and aggression. The rapid and robust anxiolytic effect of benzodiazepines and the anxiogenic effect of the benzodiazepine receptor antagonist flumazenil49 reflect a close and direct relationship between GABA and anxiety. Dysregulation of the central GABAergic system has been implicated in aggressive behavioral phenotypes,50, 51 and GABAergic drugs may be effective in reducing rage and aggression.52 GABAergic neurotransmission in local microcircuits in the nucleus accumbens mediates hedonic reactions and motivated behavior.53 As a result, predispositional and stress-related abnormalities of the GABAergic system may directly contribute to negative affect and anhedonia in MDD. Given the relatively specific familial associations between anxiety, aggression and suicide attempts,54 GABA-related genes may conceivably relate to the risk of suicidal behavior. In support of this, dysregulation of mRNA expression of GABA-A receptor subunits has been found in the frontopolar cortex, hippocampus and amygdala of depressed suicide victims.55, 56 Suicide in MDD has also been associated with altered expression of DNA methyltransferase, resulting in hypermethylation of the GABA-A receptor promoter in frontopolar cortex, amygdala and hypothalamus.57 Taken together, this evidence points to the potentially important contribution of epigenetic mechanisms to the risk of MDD/suicide. Abnormal DNA methyltransferase activity can also reduce the availability of glutamic acid decarboxylase-67 (GAD1) protein expression by methylation of the GAD1 promotor region,58 which may directly relate to reduced total cortical GABA concentration as determined by MRS.
Genetics of GABA in depression
Brain GABA levels result from the dynamic balance between synthesis, re-uptake and degradation. These processes are regulated by the enzymes glutamate decarboxylase and GABA-transaminase. A decrease in GABA synthesis or an increase in GABA degradation by GABA transaminase intracellularly within the mitochondria could result in reduced cortical GABA levels.59
A small study of plasma GABA levels in monozygotic twins60 suggests that GABA concentration is under genetic control. Specifically, a segregation analysis of plasma GABA levels in a sample of 157 individuals from 50 families revealed that familial transmission of GABA levels is compatible with segregation of a recessive major gene.60 Particularly low plasma GABA levels were found in patients with familial unipolar depression.61 Healthy relatives of patients with major depression had significantly lower plasma GABA levels than healthy controls without familial risk of depression,43 suggesting familial co-aggregation of the risk of MDD and low plasma GABA concentration that is thought to reflect GABA levels in the central nervous system. The cortical GABA-increasing effect of antidepressants62 suggests that low cortical GABA functions more as an endophenotype than simply a biomarker because its modification is likely related to altering the risk of the disease.63
GAD1 is an excellent candidate gene for the putative cortical GABA endophenotype because glutamic acid decarboxylase synthesizes GABA and GAD1 knockout mice showed dramatically reduced brain GABA concentrations.64 However, the behavior of the knockout mice was unable to be examined because they died of severe cleft palate shortly after birth. In addition, variation in the GAD1 gene has been associated with neuroticism,65 which is a risk factor of MDD. Associations between polymorphisms within the GAD1 gene and cortical GABA levels in the anterior cingulate cortex66 suggest that cortical GABA determined by MRS is heritable and useful as endophenotype for genetic studies.
Genetic factors associated with the risk of depression, such as risk alleles within the GAD1 gene, may conceivably explain the reduced concentration of GAD1 found in a postmortem study of the prefrontal cortex of MDD subjects.67 Reductions in GAD1 likely lead to reduced cortical GABA concentrations.64 Alternatively, the genetic risk of depression may be associated with the reduced density of calbindin immunoreactive GABAergic neurons that has been found in postmortem prefrontal and occipital brain tissue preparation of depressed individuals.68, 69
GABA-A receptors are sensitive to subtle, sex-specific changes in the environment throughout the lifespan.70 The short- and long-term stress sensitivity of the GABAergic system suggests that GABA-A receptors have a role in the non-genetic etiology of depression, and that this stress-sensitivity may interact with genes. Genetic variants coding for the GABA receptor α-1, α-3, α-5 and α-6 subunits have been associated with the risk of depression.71, 72, 73, 74, 75 Serotonin exerts a complex modulatory control over GABA (and glutamate) neurotransmission. This modulation involves many subtypes of 5-HT receptors and a large variety of effects.76 As a result, variants of these receptors as well as other genes related to the regulation of the serotonergic system may conceivably be associated with the GABA endophenotype in depression. The serotonin-deficiency hypothesis matches well with the GABA-deficiency hypothesis of depression because 5-HT generally reduces neuronal excitability by increasing GABA neurotransmission and decreasing glutamate neurotransmission.77, 78 In addition, there is an important influence of dopamine of the GABA system. D2 and D3 receptors were reported to be mostly associated with non-pyramidal GABAergic interneurons.79 D2 stimulation was found to presynaptically decrease GABA neurotransmission in the striatum,80 and D1 and D2 receptors were reported to modulate GABA activity in the prefrontal cortex.81 Genes associated with the dopaminergic system may therefore be associated with alteration of GABA neurotransmission in depression. In support of such an interaction, there is preliminary evidence that genetic variance in the catechol-o-methyltransferase gene, which regulates synaptic dopamine in the cortex, interacts with GAD1 polymorphisms with regard to GABA concentration in the anterior cingulate cortex.66
Glutamate-related abnormalities
Glutamate is the major excitatory neurotransmitter in the brain, having an important role in neuronal plasticity, learning and memory. Glutamate neurotransmitter release and recycling involves a series of metabolic interactions between glia cells and neurons. Glutamate can be synthesized de novo from the transamination of α-oxogluturate through the Krebs cycle. However, most of the neuronal glutamate is provided by the glutamate/glutamine cycle. Glia cells take up neuronal glutamate through excitatory amino acid transporters (EAATs). In glia cells, glutamate is converted into glutamine by the enzyme glutamine synthetase. The inactive glutamine is then transferred back to the neuron where is converted to glutamate and stored in synaptic vesicles by the activity of vesicular glutamate transporters. MRS studies have shown that the glutamate/glutamine cycle is a major metabolic pathway whose activity is directly correlated with neuronal activity,82 possibly accounting for the majority of brain glucose uptake.83 As a result, glutamate neurotransmission contribute to the blood oxygen level dependent signal as measured in fMRI studies and to glucose uptake as measured by positron emission tomography studies with radiolabeled fluorodesoxyglucose.
Depending on the sequence and editing methods used, MRS studies quantify glutamate and glutamine separately, or as a composite measure of glutamate and glutamine referred to as Glx. A series of MRS studies in depression consistently found low prefrontal and subcortical Glx.12, 84, 85, 86 Glx reductions were found in various brain regions including the anterior cingulate cortex, the dorsolateral, dorsomedial and dorsoventral prefrontal cortex, the amygdala and the hippocampus. Studies that quantified glutamate and glutamine separately suggest that glutamine rather than glutamate is reduced in depression.84, 86, 87 However, not all studies found reduced Glx in depression: some studies reported normal Glx levels in depression,88, 89 and increased glutamate concentration has been reported in the occipital cortex of depressed patients.11
Further evidence for alterations in glutamatergic metabolism comes from animal models of MDD. In the PACC, the region showing the most consistent resting state hyperactivity, glutamine has been found to be reduced in the various animal models of depression. Moreover, NMDA-receptors have been observed to be increased while AMPA-receptors were found to be reduced in this region in the animal models of depression. Hence, taken together, there seems to be some convergence between animal and human findings with the former extending the observed glutamatergic abnormalities to the receptor level, that is, AMPA and NMDA.90, 91
The glutamatergic system can have different roles when distinguishing between unipolar and bipolar depression. Reduced prefrontal and subcortical Glx has appeared as a specific marker of unipolar depression. In bipolar disorder, Glx has found to be increased in all mood states.92 Given the limited reliability and validity of symptom-based diagnostic methods to differentiate between unipolar and bipolar depression, glutamate-related MRS measures have the potential to significantly improve precision and neurobiological validity of mood disorder subtyping. Such an improvement may have a direct impact on clinical practice as therapeutic approaches for unipolar and bipolar depression differ considerably.
There is only limited data on mood-state independence of reduced Glx in depression. In the majority of MRS studies in depression, Glx levels did not correlate with symptom severity,92 suggesting that Glx is not directly associated with the experience of acute depressive symptoms. Only two studies have been conducted in asymptomatic subjects with a history of MDD. One study did not find reduced Glx in fully remitted subjects with MDD;22 the relatively mild depressive disorders in the subjects included may have contributed to this negative finding. The second study in remitted MDD cases showed increased Glx in the occipital cortex,23 which is consistent with increased occipital Glx in acute depression. The normalization of Glx after successful electroconvulsive therapy treatment93, 94 may argue against low Glx as a mood-independent marker in depression. Glutamate may be an important mediator of gene-by-environment interactions underlying depression. In animals, various types of stressors lead to rapid increase in glutamate in the extra synaptic space of the medial prefrontal cortex,95 and the glutamate system has an important role in the adaptation to repeated stress.96 The excitatory glutamatergic synaptic inputs identified in hypothalamic corticotropin-releasing hormone (CRH)-expressing neurons suggests that abnormal glutamatergic activity may contribute to the altered HPA axis activity in depression.97 Moreover, one may hypothesize that stress leads to abnormal glutamatergic inputs from stress-sensitive brain regions (medial prefrontal cortex, amgygdala, hippocampus) into the dopamine-rich brain regions of the reward system (nucleus accumbens, brain stem tegmentum).98, 99 Such glutamate–dopamine interactions may represent the neural substrate of stress-induced anhedonia, which has been proposed as the core psychopathology of depression.4
Glutamate-related MRS measures may not be appropriate to study the rapid glutamatergic stress response in living human subjects.20 Aside from direct genetic influences, low Glx in depression may reflect the neurotrophic long-term consequences of chronic stress and depression, such as reduced prefrontal glia cell size and density, which is the most consistent neuropathological finding in depression.100 In addition, metabolic influences on brain glutamate must be taken into account. For example, poor glycemic control in patients with type 1 diabetes has been associated with increased prefrontal Glx.101
We are unaware of any family or twin study examining the familiality and heritability of glutamate/glutamine concentrations in the brain, and there is a lack of data on the role of low Glx, glutamate and glutamine as risk factors of depression. Although there is no solid evidence for associations between specific glutamate-related genes and risk of depression, there are promising leads for the involvement of such genes in depressive vulnerability. A microarray analysis of prefrontal cortex from subjects who suffered from MDD showed reduced expression of the genes SLC1A2, SLC1A3 and GLUL, which encode for EAAT2, EAAT1 and glutamine synthetase, respectively.102 A recent postmortem study in the locus coeruleus, the primary origin of noradrenergic neurons, confirmed that mRNA expression of SLC1A2, SLC1A3 and GLUL is specifically downregulated in MDD.103 A study on striatal expression of EAATs found decreased SLC1A6 (EAAT4) mRNA expression in MDD.104 Vesicular glutamate transporters-1-heterozygote mice that displayed increased anxiety and depressive-like behavior also were found to have a 35–45% reduction in frontal cortical GABA concentration.105 These findings have been confirmed by a recent study using a learned helplessness model of depression that demonstrated reduced EAAT2, EAAT4 and vesicular glutamate transporters-1 expression in helpless animals.106
There is additional evidence for genes encoding glutamate receptor contributing to the risk of depression. AMPA receptor subunit 1 knockout mice showed behavioral and neurochemical features of depression including decreased serotonin and norepinephrine levels.107 Mice deficient in the NR2A subunit of the NMDA receptor exhibited an anxiolytic-like and antidepressant-like phenotype.108 Postmortem studies in the prefrontal cortex found reduced AMPA and NMDA receptor subunits in MDD, including GluR1, GluR3, GluR5, NR2A and NR2B.109, 110 Abnormal expression of the metabotropic glutamate receptors 2, 3 and 5 have been reported from studies using animal models of depression.111, 112
In summary, glutamate-related imaging endophenotypes have the potential to differentiate unipolar from bipolar disorders, which are genetically relevant mood disorder subtypes.3 There is growing evidence from animal studies that altered expression of glutamate-related proteins underlie behavioral and neurochemical characteristics of MDD including monoamine-deficiency, abnormal HPA axis activity, increased stress sensitivity and stress-induced anhedonia. These studies provide a basis for the selection of candidate genes to be tested in glutamate-related endophenotype studies. The many factors that may influence brain’s glutamate and glutamine total concentration, for example, glucose metabolism, limit the use of current glutamate imaging measures as depression endophenotypes. The development of in vivo 13C-MRS, a novel imaging method developed to visualize the flow of 13C-labeled metabolites in living humans, has the potential to provide refined glutamate-related endophenotypes by measuring specific aspects of the glutamate–glutamine cycling flux and its interaction with the GABA system.113
Resting-state activity
Resting-state activity accounts for a large part of brain energy expenditure and activity,114 which is assumed to be under genetic control. Given that resting-state activity has been found to be abnormal in depression, it is plausible that candidate neural endophenotypes for MDD can be derived from non-invasive functional MRI measures of resting-state activity.
Neuroanatomy of resting-state activity in depression
There have been several reviews about the structural and functional brain changes in MDD.26, 115, 116, 117, 118, 119, 120, 121, 122 A meta-analysis of all resting-state activity studies in depression revealed that the PACC, the ventromedial prefrontal cortex (VMPFC), the dorsomedial thalamus, the pulvinar, pallidum/putamen and midbrain regions, such as the ventral tegmental area, substantia nigra, the tectum and the periaqueductal gray, have found to be hyperactive in depression; resting state activity was hypoactive and thus reduced in the dorsolateral prefrontal cortex (DLPFC), the posterior cingulated cortex (PCC) and adjacent precuneus/cuneus.26 These results are in accordance with the findings of other groups.119, 120, 121 Drevets and colleagues emphasized the role of the hippocampus, parahippocampus and the amygdala where they also observed resting state hyperactivity.
Interestingly, the same regions and the PACC also show structural abnormalities with reduced gray matter volume in imaging studies and reduced cell density in postmortem studies.119, 121 Recent reviews show that in addition to the PACC, the medial prefrontal cortex, regions in the medial and caudolateral orbital cortex, the amygdala, the hippocampus and ventromedial parts of the basal ganglia show structural abnormalities in MDD. Hence, the functional resting state abnormalities seem to accompany structural abnormalities in the same regions and networks.121, 122 It remains unclear, however, whether the structural changes drive the functional resting state activity abnormal or, conversely, whether the functional resting state abnormalities lead to structural adaptations. This issue will also come into play when discussing the nature and classification of MDD as a potential neurodevelopmental disorder.123
Involvement of these regions in MDD is further corroborated by the investigation of resting state activity in animal models of MDD. Reviewing the regions showing resting state hyperactivity in the different animal models yielded the anterior cingulated cortex, the central and basolateral nuclei of the amygdala, the bed nucleus of the stria terminalis, the dorsal raphe, the habenula, the hippocampus, the hypothalamus, the nucleus accumbens, the periaqueductal gray, the dorsomedial thalamus, the nucleus of the solitary tract, and the piriform and prelimbic cortex.26 In contrast, evidence of hypoactive resting state activity in animal models remains sparse with inconclusive results.
These findings indicate abnormally high resting state activity in subcortical and cortical medial regions. This has led authors like Phillips, Mayberg and Drevets to assume dysfunction in the limbic system in depression, or more specifically in the ‘limbic-cortico-striato-pallido-thalamic circuit,’ with the most important interactions between the medial prefrontal and limbic regions.115, 116, 117, 121 This though may need to be extended to include subcortical regions on the mesencephalic level as it is suggested by the animal data. There is recent evidence for concurrent involvement of both cortical and subcortical regions in resting state hyperactivity.124 Specifically, relying on evidence from tasks of pure perception rather than cognition, resting state hyperactivity was demonstrated indirectly through the degree of stimulus-induced activity (for example, deactivation in resting state regions) on the cortical level (for example, paralimbic and midline regions) and the subcortical level (for example, periaqueductal gray, thalamus, tectum).
Resting-state hyperactivity may not be mood-state independent. It has been suggested that the brain activity patterns in acute depression reverse after recovery, with increased activity within dorsomedial and dorsolateral prefrontal cortices and decreased activity within the subgenual cingulate gyrus, hippocampus, thalamus, ventral striatum and insula.115 Recent positron emission tomography study on glucose metabolism in fully remitted subjects with MDD demonstrated decreased metabolism in the right DLPFC, right temporal cortex and ventromedial frontal polar cortex, while metabolism was increased significantly in the right parahippocampal cortex, dorsal anterior cingulate cortex and frontal polar cortex,125 which seems to be consistent with increased paralimbic-midline hyperactivity as putative imaging MDD endophenotype.
Psychopathology of resting state activity increased self-focus and hopelessness
Increased self-focus reflects the heightened awareness of the self in depressed patients and their decreased focused on the environment including ongoing events, persons and objects.126 The increased self-focus accompanies the abnormal attribution of predominantly negative emotions to the self and increased cognitive processing of the self with subsequent ruminations. Recent imaging studies reported reduced signal changes during the presentation of either self-related emotional words or emotional pictures.127, 128, 129 All studies demonstrated abnormal activity changes in the anterior paralimbic-midline regions like the PACC, the VMPFC and the DMPFC in depression. These anterior paralimbic-midline regions have been associated with self-related processing that describes the process by means of which personal relevance or meaning and thus self-relatedness is assigned to exteroceptive and interoceptive stimuli.129, 130, 131 As self-relatedness is already highly activated in the resting state, it might be expected to be abnormally low with regard to external stimuli, thus assuming reduced rest-stimulus interaction even in the case of highly self-related external stimuli. In contrast, internally-generated stimuli as related to the abnormally elevated resting state activity may be assigned an abnormally high degree of personal relevance as it is highly visible in the ruminations of MDD patients. Hence, it can be assumed that there exists a disequilibrium between internally and externally generated stimuli, with the former showing increased resting state activity while latter demonstrates a decreased resting state. Symptomatically this disequilibrium in rest-stimulus interaction between internally and externally generated stimuli may correspond to the increased self-focus, and may also be associated with the environmental counterpart sometimes described as ‘decreased environment-focus’.
Another central feature in MDD is hopelessness. Hopelessness is closely related to the ability to extend the self and its expectations into the future. If an individual is no longer able to extend and project the self into the future, he/she can no longer maintain any future-oriented hopefulness. This is exactly what seems to happen in MDD. Almost all items in the Beck Hopelessness scale (BHS) concern the ability to anticipate the self in the future and to project it forward in time. Recent studies demonstrated that MDD patients do indeed show significantly increased scores on the BHS when compared with healthy subjects.129 Moreover, these studies showed that increased resting state activity in the PACC and the VMPFC correlated with the BHS. Specifically, the higher the resting state activity in the PACC and VMPFC, the higher the score in the BHS.
Resting state activity and GABA
A recent study combined MRS and functional MRI to investigate the level of GABA in a typical DMN region, the PACC that, as part of the DMN, shows a predominantly negative blood oxygen level dependent response (NBR).132 As demonstrated in this study, the resting state level of GABA in the PACC correlated with the degree of NBR as induced by an emotional judgment task in the very same region. Thus, an increase in the resting state concentration of GABA in the PACC was positively correlated with an increase in the degree of NBR during stimulus-induced activity. This study showed that the resting state concentration of GABA in the PACC may indeed impact stimulus-induced activity changes in the PACC, suggesting that the resting state activity level (that is, GABA) in a DMN region may impact the degree of stimulus-induced activity in the same region.
Another study in healthy subjects investigated the resting state concentration of GABA in the visual cortex and its effects on subsequent stimulus-induced activity in the both visual cortex and γ frequency bands.133 The investigators measured resting state levels of GABA in the visual cortex with MRS and used fMRI and magnetoencephalography to measure stimulus-induced activity changes in the visual cortex. The resting state concentration of GABA in the visual cortex predicted the degree of stimulus-induced activation (that is, positive blood oxygen level dependent response) and the γ frequency in the very same region.
Despite focusing on different regions, that is, PACC and visual cortex, both studies observed prediction of stimulus-induced activity by resting state level of GABA. In contrast, resting state levels of glutamate, an excitatory transmitter, were not related to rest-stimulus interaction. This suggests that the resting state concentration of GABA as the major inhibitory transmitter may have a crucial role in linking resting state activity to stimulus-induced activity, thereby making possible rest-stimulus interactions.134
Depressed patients show abnormally elevated resting state activity, which could be assumed to also impact stimulus-induced activity amounting to abnormal rest-stimulus interaction. If rest-stimulus interaction is mediated by GABA in healthy subjects, it has the potential to abnormally mediate rest-stimulus interaction in depression. One previous study tested this hypothesis by relating the stimulus-induced signal changes in the PACC as the typical default-mode network region to the concentration of GABA and glutamate in the same region.87 As expected, depressed patients observed decreased signal changes, for example, deactivation in the PACC, as being indicative of increased resting state activity. Most interestingly, the reduced deactivation was no longer related to the concentration of GABA. Instead, deactivation in the PACC was predicted by the glutamate concentration in the same region, which was not observed in the healthy group.
Although these findings have yet to be replicated, they nevertheless suggest that the increased resting state activity in the midline regions and its impact on stimulus-induced activity, for example, rest-stimulus interaction, may be mediated by lack of neural inhibition as related to GABA. This, in turn, may then lead to relatively increased neural excitation as mediated by glutamate. The crucial role of GABA and GABAergic-mediated inhibition in depression is further corroborated by results from transcranial magnetic stimulation. Transcranial magnetic stimulation allows the study of resting state activity by measuring neural inhibition using silent period and paired pulse techniques. Severely depressed MDD patients demonstrated deficits in both silent period and paired pulse in the motor cortex, which is indicative of a deficit of cortical inhibition as mediated by GABA-A and GABA-B receptors.135, 136, 137 However, it is important to note that these studies concern the motor cortex as part of the outer ring, the lateral cortical regions. Although there is a need for studies of cortical excitability in paralimbic and midline regions, currently these studies are difficult, if not impossible, to target with transcranial magnetic stimulation.
Finally, it is necessary to discuss the relationship between GABA/glutamate and serotonin as a key player in depression. There is an abundance of evidence for serotoninergic abnormalities in MDD concerning the level of serotonin and specific sertoninergic receptors (5HT-1a, 5HT-1b and so on) in subcortical and cortical paralimbic-midline regions,119, 122, and such abnormalities can be related to GABA and glutamate. GABAergic and glutamatergic systems are ubiquitous throughout the cortex and in most subcortical regions. This distinguishes these receptors from more specific neuromodulatory systems, such as the serotonergic and adrenergic-noradrenergic systems. These systems originate in the subcortical regions (raphe nuclei, locus cerulous) and are connected through forebrain-limbic regions to paralimbic and midline regions in anterior parts of the cortex, such as the VMPFC and the PACC.138 However, serotoninergic neurons are connected to GABAergic interneurons on both subcortical and cortical levels, making it more likely that alterations in the serotoninergic systems necessarily initiate changes in the GABAergic and glutamatergic systems.
What remains unclear, however, is whether the predominantly cortical GABAergic abnormalities in paralimbic brain regions (for example, the PACC) drive the serotoninergic system abnormal in a kind of top-down modulation, or whether the subcortical serotoninergic afferences impact cortical GABA in the PACC through bottom-up modulation. Hence, future studies combining humans and animals may test both options, top-down and bottom-up modulation, by causally interfering with serotoninergic and GABAergic systems in both subcortical and cortical regions (for example, through deep brain stimulation in PACC).
Functional connectivity
Phenotypic definitions can by derived from any type of imaging information, including measures of structural measures of connectivity using diffusion tensor imaging and functional connectivity. Neural connectivity has been successfully used as a neural endophenotype to elucidate the impact of serotonergic and dopaminergic genes on brain structure and function.139 The use of endophenotypes derived from abnormal functional connectivity has been particularly successful in psychosis research.140 For example, extensive imaging work in schizophrenia patients has provided evidence for abnormal functional connectivity of the DLPFC and the hippocampus.141 A genome-wide association study has identified an association between a single nucleotide polymorphism in the ZNF804A gene and psychosis. A recently published imaging-genetics study in healthy volunteers142 showed that this genetic variant relates to alterations in functional coupling of the DLPFC across hemispheres and with the hippocampus, mirroring the findings in psychotic patients.
Functional connectivity during the resting state
Several studies investigated functional connectivity during the resting state. Usually, subjects are required to keep their eyes closed in the fMRI while they are imaged for 5–10 min. Various multivariate techniques such as structural equation modeling, regression of single voxel against all others, or Granger causality estimation technique are used to analyze functional connectivity. Generally, studies are conducted in unmedicated patients so that medication can be excluded as possible confounding factor.
Recently, fMRI has been used to examine resting state connectivity in depression. These studies found reduced resting state connectivity either between the amygdale and the PACC,143 between PACC and bilateral dorsomedial thalamus,144 and between posterior midline regions.145 These regions included the PACC, precuneus and bilateral caudate.145 Unfortunately, subcortical regions are rarely considered in these studies. Because of the difficulty of locating the ventral striatum or raphe in fMRI may account for the sole focus on the thalamus in these imaging studies. A positron emission tomography study on resting state connectivity146 included seven nodes or core regions, the hippocampus, the DLPFC, the PACC, the subgenual anterior cingulate cortex (SACC), the thalamus, the MPFC and the OFC. The resting state connectivity pattern among these regions was found to be predictive of subsequent treatment response in an untreated MDD sample. In a subsequent fMRI resting state study in 46 untreated MDD patients,147 the DLPFC was decoupled from the other midline regions, such as the hippocampus, the PACC and the SACC, thus showing reduced connectivity. Moreover, reciprocal connectivity between PACC and SACC was reduced or resolved in the MDD patients. However, this study did not include a healthy sample for direct comparison, which considerably reduces its scientific significance.
These findings of reduced resting state connectivity contrasts with those studies showing increased connectivity in limbic, paralimbic and frontal brain regions. In a recent fMRI study, the connectivity patterns of three seed regions, the PACC, precuneus and DLPFC, converged in the SACC with some extension into an area of the DMPFC described as the ‘dorsal nexus’.148 The dorsal nexus showed increased connectivity with the PACC, the DLPFC, the VMPFC and the PCC in MDD patients when compared with healthy subjects. Increased resting state connectivity in depression was also found between the DLPFC, the PCC and the MOFC,149 between the PACC and the left anterior insula in severely depressed patients,150 and from the PACC to the thalamus.151 Increased connectivity pattern of both subgenual and pregenual anterior cingulated cortex was related to subsequent response to deep brain stimulation.152 Increased resting state connectivity from the hippocampus to the PACC and leading to the MPFC was interpreted as increased excitation within limbic/paralimbic regions, whereas decreased connectivity to and from the DLPFC was interpreted as increased neural inhibition in lateral prefrontal cortex.153
Taken together, these results demonstrate both increased and decreased functional connectivity in the resting state. In both cases, the core regions include midline regions, such as the PACC, the DLPFC, the MPFC, the PCC and the dorsomedial thalamus, yet the direction of changes remains controversial. Whether the opposite findings are because of the different methods used to analyze connectivity or to differences in patient populations remains unclear.
There has yet to be a consensus regarding the relationship between structural and functional connectivity. Some studies in healthy subjects154 observed the patterns in functional connectivity to be analogous to those in structural connectivity as measured with diffusion tensor imaging. However, functional and structural connectivity patterns did not map onto each other one-to-one and thus were not identical. The mechanism of alteration in the structural-functional relationship in MDD remains unclear. For example, it could be theorized that the functional connectivity in the resting state diverges more strongly from the structural connectivity in MDD, and that this divergence may be crucial in leading to the previously described changes in the level of the resting state activity. However, combined structural and functional resting state connectivity patterns in MDD have yet to be investigated. In addition, relationship between resting state connectivity abnormalities and biochemical changes (such as in GABA and glutamate) remains unclear. One recent study found the abnormally increased resting state activity between the PACC and the left anterior insula to be predicted by the concentration of glutamate in the PACC. Specifically, greater concentrations glutamate lead to increased connectivity from the PACC to the insula in medicated MDD patients.150
There is a lack of data on mood-state independence of resting-state connectivity. Some studies reported correlations between abnormal resting-state connectivity and severity of depression,150 suggesting that these changes are partly mood-state dependent. In a randomly selected community sample, the heritability of default-mode functional connectivity was 42%.155 Although neuroanatomical variation in the default-mode network was also heritable, the genetic factors that influenced functional connectivity and gray-matter density were distinct. Genetic correlations between regions suggest that the same set of genes contribute to variation in functional connectivity throughout the default-mode network. Interestingly, the parahippocampal region, which has appeared to have major roles in depression,4 was genetically correlated with all other network regions. A study on functional connectivity in healthy subjects at risk of MDD found decreased regional homogeneity in the right insula and the left cerebellum.156
Functional connectivity during affective or cognitive stimulation
Analogous to resting state connectivity, functional connectivity has also been investigated during stimulus-induced activity, such as during emotional or cognitive stimulation. Therefore, similar techniques to those as mentioned above are used and similar regions are highlighted. Analogous to the resting state connectivity data, results are still uncertain with regard to increases or decreases in functional connectivity during stimulation.
Severely depressed patients with catatonic syndrome showed significantly decreased connectivity between the MOFC/VMPFC and the premotor cortex in response to emotional stimuli.157 Reduced connectivity in response to emotional pictures of the PACC with the dorsomedial thalamus, the striatum and the amygdala was found in MDD patients.143 MDD patients also showed significantly decreased connectivity from the LOFC to the SACC/DACC and the precuneus in an implicit and explicit facial recognition paradigm,158 while connectivity was increased in MDD patients from the LOFC to the right DLPFC, the right inferior operculum and the motor cortex. Increases in connectivity during an emotion task were also observed in MDD, although in different brain regions: the amygdala, hippocampus and the caudate/putamen.159 Increased functional connectivity related to the MPFC was observed in two studies testing for self-relatedness.128, 160 In addition to emotional and self-related stimuli, functional connectivity has also been investigated during cognitive tasks. One study found increased connectivity from the PACC to the SACC/DACC and the MPFC during a color Stroop Task,161 whereas another study found almost the opposite, finding reduced connectivity and thus uncoupling between PACC and MPFC during a working memory task.162
Taken together, analogous to the resting state connectivity, there are reports of both increases and decreases of stimulation-induced connectivity, concerning almost the same regions as in the resting state. This suggests that resting state and stimulus-induced activity and connectivity may somehow be dependent on each other. There are promising preliminary findings studying the influence of resting state on stimulus-induced activity, for example, rest-stimulus interaction.134 In contrast, we have seen no published results concerning the relationship between functional connectivity during resting state and stimulation in either healthy or depressed subjects.
Methodological issues may have contributed to the disagreements in the functional connectivity literature in depression. The different studies rely on different methods of analyzing functional connectivity. Methods like structural equation modeling, regression analysis, independent component analysis, principal component analysis and dynamic causal modeling are used. They all make different presuppositions and use different statistical methods to analyze the effect of signal changes. Furthermore, the link between functional connectivity during specific tasks and structural connectivity remains unclear. Whether functional connectivity is altered independent of structural connectivity in MDD or whether functional changes reflect structural alterations remains open.
There is a paucity of data on the biochemical and genetic modulation of functional connectivity during stimulation. A recent study investigated MDD patients with magnetoencephalography during a working memory task during an NMDA-antagonist ketamine challenge.163 This study found the connectivity between PACC and amygdale to be sensitive to modulation by ketamine and, more importantly, its therapeutic effects. This suggests that functional connectivity between these two regions during stimulation may be mediated by glutamate. As opposed to glutamate, functional connectivity during stimulation has not been related to GABA. The heritability and association of functional stimulation with the risk of MDD has yet to be investigated. One study reported that the functional connectivity between the PACC and the amygdala during negative emotional pictures is abnormally coupled to the expression of 5-HTT low-expression risk alleles in MDD patients.164 Another issue that remains unclear in this context is how the seemingly altered functional connectivity is related to the various neuropsychological abnormalities in such functions as attention, working memory and executive function in MDD (see ref. 165 for a review). The question arising from the neurophysiological point of view is how the resting state hyperactivity impacts stimulus-induced activity and subsequently the neuronal mechanisms underlying these various cognitive functions. Thus, before we will be able to link the neuropsychological deficits in MDD to specific neural networks and their functional connectivity, we may need to better understand what has been recently called ‘rest-stimulus interaction’134 in both healthy subjects and depressed patients.
Discussion
The importance of the phenotypic definition for the success of gene identification was precisely demonstrated by the discovery of the association between the period gene and length of the circadian cycle.166 The choice of the circadian period among the measurable circadian rhythm parameters including phase, period and amplitude was crucial. As period lengths can be easily and accurately measured, this measure is almost two orders of magnitude more precise than commonly used behavioral assays, such as fear conditioning.167 In addition, period length reflects a rate-limiting process, whereas amplitude is significantly influenced by output pathways. In addition, phase is influenced by changes in input pathways, which weakens the associations of these measures with specific genetic factors. In psychiatry, we currently lack a deep understanding of the phenotype and, therefore, we do not know which aspects of psychiatric conditions reflect fundamental, rate-limiting processes. Not surprisingly, the association between candidate genes and endophenotypes frequently used in psychiatric genetics, such as P300 amplitude and latency, performance on working memory tasks and other cognitive measures, have not been found to be stronger than those between specific gene loci and traditional psychiatric disorder phenotypes.8
The aim of this perspective review was to propose putative imaging endophenotypes derived from non-invasive, reasonably available imaging methods that are presumably close to gene and gene products and meet some of the endophenotype criteria. We did not review findings from other, more invasive types of neuroimaging, such as positron emission tomography and single photon emission computed tomography, although these methods have provided important insight into the pathophysiology of depression. As possible associations between imaging endophenotypes and monoaminergic genes and genes related to the HPA axis were included in a previous review,4 they were not discussed here. Many important functional imaging findings in depression are based on behavioral experiments related to higher-order psychological functions, such as the processing of negative feedback or the control of emotions. Assuming that there is a long road between genes and measures from these experiments, which reduces the likelihood of identifying genetic associations, we did not review the imaging literature related to higher-order psychological constructs.
MRS provides candidate endophenotypes that may have relatively close relationships to genes and gene products. Reduced cortical GABA is a consistent and relatively specific neurobiological abnormality in depression, which may be partly mood-state independent. Studies on plasma GABA concentrations provide evidence for genetic control of GABA concentration and for genetic associations between low GABA and the risk of MDD. There is preliminary evidence for variations within the GABAergic GAD1 gene to be associated with cortical GABA and increased stress sensitivity, leading to increased depressive vulnerability. Taken together, low cortical GABA has appeared to be the most promising putative imaging endophenotype in MDD.
Another promising MRS measure as possible mood disorder endophenotype is prefrontal glutamate/glutamine concentration. Given that Glx was found to be reduced in unipolar depression and increased in bipolar depression, this marker has the potential to differentiate between unipolar and bipolar disorder, which has important clinical implications. The heritability of the Glx signal and associations between low prefrontal Glx and the genetic risk of MDD are largely unknown. However, animal and postmortem studies have provided promising leads for glutamate-related MDD risk genes including SLC1A2, SLC1A3, GLUL and various glutamate receptor genes.
There is convergent support from human neuroimaging studies and animal models of depression for the role of increased resting-state activity in the pathophysiology of depression, possibly associated with increased self-focus, decreased environment-focus and hopelessness. Evidence for increased midline glucose metabolism in remitted depression and the association among GABA, serotonin and resign-state activity contribute to the plausibility of increased resting-state activity as putative imaging endophenotype in depression.
Functional connectivity measures were found to be heritable and were successfully used to elucidate the impact of serotonergic and dopaminergic genes on brain function. Abnormal functional resting-state connectivity has consistently been found in midline brain regions, although the direction of change remains controversial. Functional connectivity during emotional or cognitive stimulation has found to be abnormal in almost the same brain regions as in the resting-state. Standardization of functional connectivity measures and studies on connectivity in asymptomatic subjects at risk of MDD are needed to evaluate functional and structural connectivity as depression endophenotypes.
Future directions
The dramatic progress in MR-based imaging methods has the potential to identify subtle abnormalities of neural structures, connectivity and function in depressed patients and healthy subjects at familial risk of MDD. Well-designed twin, family and prospective studies in high-risk populations are needed to discover and evaluate imaging measures as depression endophenotypes. As these measures are relatively low-cost and increasingly available, they will facilitate the identification of MDD risk genes in candidate gene and genome-wide association studies. In addition, by reducing clinical heterogeneity, these measures will help to develop and evaluate novel therapeutic options and enable clinicians to apply individual-tailored therapeutic approaches. Finally, improvements of the phenotypic definition of MDD will contribute to a new classification system for mood disorders based on etiology and pathophysiology. More specifically, one would need to investigate how the suggested endophenotypes of increased self-focus, anhedonia and increased stress-sensitivity relate to the various psychopathological MDD symptoms and syndromes. One might speculate that anhedonia and reduced reward-induced activity and connectivity underlie melancholic depressive symptoms, that increased stress reactivity may be associated with interpersonal rejection sensitivity in atypical depression, and that increased self-focus might show a relationship to what has been referred to as ‘narcissistic depression’. One must remember, however, that currently defined symptom-based MDD subtypes do not breed true and should not be used as reference points in endophenotypic studies. Investigations must be done in a brain-based manner by investigating how the above-describe genetic, biochemical and neural changes supposed to be associated with the different endophenotypes lead to the neuronal changes underlying the different depressive symptoms.
References
Sullivan PF, Neale MC, Kendler KS . Genetic epidemiology of major depression: review and meta-analysis. Am J Psychiatry 2000; 157: 1552–1562.
Wellcome Trust Consortium. Genome-wide association study of 14 000 cases of seven common diseases and 3000 shared controls. Nature 2007; 447: 661–678.
Hasler G, Drevets WC, Gould TD, Gottesman II, Manji HK . Toward constructing an endophenotype strategy for bipolar disorders. Biol Psychiatry 2006; 60: 93–105.
Hasler G, Drevets WC, Manji HK, Charney DS . Discovering endophenotypes for major depression. Neuropsychopharmacology 2004; 29: 1765–1781.
Gottesman II, Shields J . Genetic theorizing and schizophrenia. Br J Psychiatry 1973; 122: 15–30.
Gottesman II, Gould TD . The endophenotype concept in psychiatry: etymology and strategic intentions. Am J Psychiatry 2003; 160: 636–645.
Preston GA, Weinberger DR . Intermediate phenotypes in schizophrenia: a selective review. Dialogues Clin Neurosci 2005; 7: 165–179.
Flint J, Munafo MR . The endophenotype concept in psychiatric genetics. Psychol Med 2007; 37: 163–180.
Petty F, Sherman AD . Plasma GABA levels in psychiatric illness. J Affect Disord 1984; 6: 131–138.
Sanacora G, Mason GF, Rothman DL, Behar KL, Hyder F, Petroff OA et al. Reduced cortical gamma-aminobutyric acid levels in depressed patients determined by proton magnetic resonance spectroscopy. Arch Gen Psychiatry 1999; 56: 1043–1047.
Sanacora G, Gueorguieva R, Epperson CN, Wu YT, Appel M, Rothman DL et al. Subtype-specific alterations of gamma-aminobutyric acid and glutamate in patients with major depression. Arch Gen Psychiatry 2004; 61: 705–713.
Hasler G, van der Veen JW, Tumonis T, Meyers N, Shen J, Drevets WC . Reduced prefrontal glutamate/glutamine and gamma-aminobutyric acid levels in major depression determined using proton magnetic resonance spectroscopy. Arch Gen Psychiatry 2007; 64: 193–200.
Kaufman RE, Ostacher MJ, Marks EH, Simon NM, Sachs GS, Jensen JE et al. Brain GABA levels in patients with bipolar disorder. Prog Neuropsychopharmacol Biol Psychiatry 2009; 33: 427–434.
Tayoshi S, Nakataki M, Sumitani S, Taniguchi K, Shibuya-Tayoshi S, Numata S et al. GABA concentration in schizophrenia patients and the effects of antipsychotic medication: a proton magnetic resonance spectroscopy study. Schizophr Res 2010; 117: 83–91.
Ongur D, Prescot AP, McCarthy J, Cohen BM, Renshaw PF . Elevated gamma-aminobutyric Acid levels in chronic schizophrenia. Biol Psychiatry 2010; 68: 667–670.
Goddard AW, Mason GF, Almai A, Rothman DL, Behar KL, Petroff OA et al. Reductions in occipital cortex GABA levels in panic disorder detected with 1h-magnetic resonance spectroscopy. Arch Gen Psychiatry 2001; 58: 556–561.
Hasler G, van der Veen JW, Geraci M, Shen J, Pine D, Drevets WC . Prefrontal cortical gamma-aminobutyric acid levels in panic disorder determined by proton magnetic resonance spectroscopy. Biol Psychiatry 2009; 65: 273–275.
Behar KL, Rothman DL, Petersen KF, Hooten M, Delaney R, Petroff OA et al. Preliminary evidence of low cortical GABA levels in localized 1H-MR spectra of alcohol-dependent and hepatic encephalopathy patients. Am J Psychiatry 1999; 156: 952–954.
Sanacora G, Mason GF, Rothman DL, Hyder F, Ciarcia JJ, Ostroff RB et al. Increased cortical GABA concentrations in depressed patients receiving ECT. Am J Psychiatry 2003; 160: 577–579.
Hasler G, van der Veen JW, Grillon C, Drevets W, Shen J . Effect of acute psychological stress on prefrontal gamma-aminobutyric acid concentration determined by proton magnetic resonance spectroscopy. Am J Psychiatry 2010; 167: 1226–1231.
Otero Losada ME . Changes in central GABAergic function following acute and repeated stress. Br J Pharmacol 1988; 93: 483–490.
Hasler G, Neumeister A, van der Veen JW, Tumonis T, Bain EE, Shen J et al. Normal prefrontal gamma-aminobutyric acid levels in remitted depressed subjects determined by proton magnetic resonance spectroscopy. Biol Psychiatry 2005; 58: 969–973.
Bhagwagar Z, Wylezinska M, Jezzard P, Evans J, Ashworth F, Sule A et al. Reduction in occipital cortex gamma-aminobutyric acid concentrations in medication-free recovered unipolar depressed and bipolar subjects. Biol Psychiatry 2007; 61: 806–812.
Petty F, Steinberg J, Kramer GL, Fulton M, Moeller FG . Desipramine does not alter plasma GABA in patients with major depression. J Affect Disord 1993; 29: 53–56.
Petty F, Kramer GL, Fulton M, Davis L, Rush AJ . Stability of plasma GABA at four-year follow-up in patients with primary unipolar depression. Biol Psychiatry 1995; 37: 806–810.
Alcaro A, Panksepp J, Witczak J, Hayes DJ, Northoff G . Is subcortical-cortical midline activity in depression mediated by glutamate and GABA?A cross-species translational approach. Neurosci Biobehav Rev 2010; 34: 592–605.
Caspi A, Hariri AR, Holmes A, Uher R, Moffitt TE . Genetic sensitivity to the environment: the case of the serotonin transporter gene and its implications for studying complex diseases and traits. Am J Psychiatry 2010; 167: 509–527.
Kendler KS, Thornton LM, Gardner CO . Stressful life events and previous episodes in the etiology of major depression in women: an evaluation of the ‘kindling’ hypothesis. Am J Psychiatry 2000; 157: 1243–1251.
Sheline YI, Gado MH, Kraemer HC . Untreated depression and hippocampal volume loss. Am J Psychiatry 2003; 160: 1516–1518.
Hasler G, Fromm S, Alvarez RP, Luckenbaugh DA, Drevets WC, Grillon C . Cerebral blood flow in immediate and sustained anxiety. J Neurosci 2007; 27: 6313–6319.
Frodl TS, Koutsouleris N, Bottlender R, Born C, Jager M, Scupin I et al. Depression-related variation in brain morphology over 3 years: effects of stress? Arch Gen Psychiatry 2008; 65: 1156–1165.
Kendler KS, Thornton LM, Prescott CA . Gender differences in the rates of exposure to stressful life events and sensitivity to their depressogenic effects. Am J Psychiatry 2001; 158: 587–593.
de Groote L, Linthorst AC . Exposure to novelty and forced swimming evoke stressor-dependent changes in extracellular GABA in the rat hippocampus. Neuroscience 2007; 148: 794–805.
Acosta GB, Otero Losada ME, Rubio MC . Area-dependent changes in GABAergic function after acute and chronic cold stress. Neurosci Lett 1993; 154: 175–178.
Gronli J, Fiske E, Murison R, Bjorvatn B, Sorensen E, Ursin R et al. Extracellular levels of serotonin and GABA in the hippocampus after chronic mild stress in rats. A microdialysis study in an animal model of depression. Behav Brain Res 2007; 181: 42–51.
Hasler G, Nugent AC, Carlson PJ, Carson RE, Geraci M, Drevets WC . Altered cerebral GABAA-benzodiazepine receptor binding in panic disorder determined by [11C]flumazenil PET. Arch Gen Psychiatry 2008; 65: 1166–1175.
Acosta GB, Rubio MC . GABAA receptors mediate the changes produced by stress on GABA function and locomotor activity. Neurosci Lett 1994; 176: 29–31.
Cullinan WE, Wolfe TJ . Chronic stress regulates levels of mRNA transcripts encoding beta subunits of the GABA(A) receptor in the rat stress axis. Brain Res 2000; 887: 118–124.
Dennis T, Beauchemin V, Lavoie N . Differential effects of olfactory bulbectomy on GABAA and GABAB receptors in the rat brain. Pharmacol Biochem Behav 1993; 46: 77–82.
Drugan RC, Morrow AL, Weizman R, Weizman A, Deutsch SI, Crawley JN et al. Stress-induced behavioral depression in the rat is associated with a decrease in GABA receptor-mediated chloride ion flux and brain benzodiazepine receptor occupancy. Brain Res 1989; 487: 45–51.
Longone P, Rupprecht R, Manieri GA, Bernardi G, Romeo E, Pasini A . The complex roles of neurosteroids in depression and anxiety disorders. Neurochem Int 2008; 52: 596–601.
Klumpers UM, Veltman DJ, Boellaard R, Comans EF, Zuketto C, Yaqub M et al. Comparison of plasma input and reference tissue models for analysing [(11)C] flumazenil studies. J Cereb Blood Flow Metab 2007; 28: 579–587.
Bjork JM, Moeller FG, Kramer GL, Kram M, Suris A, Rush AJ et al. Plasma GABA levels correlate with aggressiveness in relatives of patients with unipolar depressive disorder. Psychiatry Res 2001; 101: 131–136.
McCarthy MM, Auger AP, Perrot-Sinal TS . Getting excited about GABA and sex differences in the brain. Trends Neurosci 2002; 25: 307–312.
Searles RV, Yoo MJ, He JR, Shen WB, Selmanoff M . Sex differences in GABA turnover and glutamic acid decarboxylase (GAD(65) and GAD(67)) mRNA in the rat hypothalamus. Brain Res 2000; 878: 11–19.
Wilson MA, Biscardi R . Sex differences in GABA/benzodiazepine receptor changes and corticosterone release after acute stress in rats. Exp Brain Res 1994; 101: 297–306.
Skilbeck KJ, Hinton T, Johnston GA . Sex-differences and stress: effects on regional high and low affinity [3H]GABA binding. Neurochem Int 2008; 52: 1212–1219.
Shen J . (13)C magnetic resonance spectroscopy studies of alterations in glutamate neurotransmission. Biol Psychiatry 2005; 59: 883–887.
Nutt DJ, Glue P, Lawson C, Wilson S . Flumazenil provocation of panic attacks. Evidence for altered benzodiazepine receptor sensitivity in panic disorder. Arch Gen Psychiatry 1990; 47: 917–925.
Fish EW, Faccidomo S, DeBold JF, Miczek KA . Alcohol, allopregnanolone and aggression in mice. Psychopharmacology (Berl) 2001; 153: 473–483.
Sustkova-Fiserova M, Vavrova J, Krsiak M . Brain levels of GABA, glutamate and aspartate in sociable, aggressive and timid mice: an in vivo microdialysis study. Neuro Endocrinol Lett 2009; 30: 79–84.
Hoffman DA . Tiagabine for rage, aggression, and anxiety. J Neuropsychiatry Clin Neurosci 2005 Spring 17: 252.
Reynolds SM, Berridge KC . Positive and negative motivation in nucleus accumbens shell: bivalent rostrocaudal gradients for GABA-elicited eating, taste ‘liking’/‘disliking’ reactions, place preference/avoidance, and fear. J Neurosci 2002; 22: 7308–7320.
Gureje O, Oladeji B, Hwang I, Chiu WT, Kessler RC, Sampson NA et al. Parental psychopathology and the risk of suicidal behavior in their offspring: results from the World Mental Health surveys. Mol Psychiatry 2011 (in press).
Merali Z, Du L, Hrdina P, Palkovits M, Faludi G, Poulter MO et al. Dysregulation in the suicide brain: mRNA expression of corticotropin-releasing hormone receptors and GABA(A) receptor subunits in frontal cortical brain region. J Neurosci 2004; 24: 1478–1485.
Poulter MO, Du L, Zhurov V, Palkovits M, Faludi G, Merali Z et al. Altered organization of GABA(A) receptor mRNA expression in the depressed suicide brain. Front Mol Neurosci 2010; 3: 3.
Poulter MO, Du L, Weaver IC, Palkovits M, Faludi G, Merali Z et al. GABAA receptor promoter hypermethylation in suicide brain: implications for the involvement of epigenetic processes. Biol Psychiatry 2008; 64: 645–652.
Dong E, Agis-Balboa RC, Simonini MV, Grayson DR, Costa E, Guidotti A . Reelin and glutamic acid decarboxylase67 promoter remodeling in an epigenetic methionine-induced mouse model of schizophrenia. Proc Natl Acad Sci USA 2005; 102: 12578–12583.
Tunnicliff G . 4-aminobutyrate transaminase. In: Boulton AA, Baker GB, Yu PH (eds). Neurotransmitter Enzymes. Humana Press: Clifton, NJ, 1986.
Petty F, Fulton M, Kramer GL, Kram M, Davis LL, Rush AJ . Evidence for the segregation of a major gene for human plasma GABA levels. Mol Psychiatry 1999; 4: 587–589.
Petty F, Schlesser MA . Plasma GABA in affective illness. A preliminary investigation. J Affect Disord 1981; 3: 339–343.
Bhagwagar Z, Wylezinska M, Taylor M, Jezzard P, Matthews PM, Cowen PJ . Increased brain GABA concentrations following acute administration of a selective serotonin reuptake inhibitor. Am J Psychiatry 2004; 161: 368–370.
Kendler KS, Neale MC . Endophenotype: a conceptual analysis. Mol Psychiatry 2010; 15: 789–797.
Asada H, Kawamura Y, Maruyama K, Kume H, Ding RG, Kanbara N et al. Cleft palate and decreased brain gamma-aminobutyric acid in mice lacking the 67-kDa isoform of glutamic acid decarboxylase. Proc Natl Acad Sci USA 1997; 94: 6496–6499.
Hettema JM, An SS, Neale MC, Bukszar J, Van den Oord EJ, Kendler KS et al. Association between glutamic acid decarboxylase genes and anxiety disorders, major depression, and neuroticism. Mol Psychiatry 2006; 11: 752–762.
Marenco S, Savostyanova AA, Van der Veen JW, Geramita M, Stern A, Barnett AS et al. Genetic modulation of GABA levels in the anterior cingulate cortex by GAD1 and COMT. Neuropsychopharmacology 2010; 35: 1708–1717.
Karolewicz B, Maciag D, O’Dwyer G, Stockmeier CA, Feyissa AM, Rajkowska G . Reduced level of glutamic acid decarboxylase-67 kDa in the prefrontal cortex in major depression. Int J Neuropsychopharmacol 2010; 13: 411–420.
Maciag D, Hughes J, O’Dwyer G, Pride Y, Stockmeier CA, Sanacora G et al. Reduced density of calbindin immunoreactive GABAergic neurons in the occipital cortex in major depression: relevance to neuroimaging studies. Biol Psychiatry 2010; 67: 465–470.
Rajkowska G, O’Dwyer G, Teleki Z, Stockmeier CA, Miguel-Hidalgo JJ . GABAergic neurons immunoreactive for calcium binding proteins are reduced in the prefrontal cortex in major depression. Neuropsychopharmacology 2007; 32: 471–482.
Skilbeck KJ, Johnston GA, Hinton T . Stress and GABA receptors. J Neurochem 2010; 112: 1115–1130.
Sen S, Villafuerte S, Nesse R, Stoltenberg SF, Hopcian J, Gleiberman L et al. Serotonin transporter and GABAA alpha 6 receptor variants are associated with neuroticism. Biol Psychiatry 2004; 55: 244–249.
Oruc L, Verheyen GR, Furac I, Ivezic S, Jakovljevic M, Raeymaekers P et al. Positive association between the GABRA5 gene and unipolar recurrent major depression. Neuropsychobiology 1997; 36: 62–64.
Yamada K, Watanabe A, Iwayama-Shigeno Y, Yoshikawa T . Evidence of association between gamma-aminobutyric acid type A receptor genes located on 5q34 and female patients with mood disorders. Neurosci Lett 2003; 349: 9–12.
Horiuchi Y, Nakayama J, Ishiguro H, Ohtsuki T, Detera-Wadleigh SD, Toyota T et al. Possible association between a haplotype of the GABA-A receptor alpha 1 subunit gene (GABRA1) and mood disorders. Biol Psychiatry 2004; 55: 40–45.
Henkel V, Baghai TC, Eser D, Zill P, Mergl R, Zwanzger P et al. The gamma amino butyric acid (GABA) receptor alpha-3 subunit gene polymorphism in unipolar depressive disorder: a genetic association study. Am J Med Genet B Neuropsychiatr Genet 2004; 126B: 82–87.
Ciranna L . Serotonin as a modulator of glutamate-and GABA-mediated neurotransmission: implications in physiological functions and in pathology. Curr Neuropharmacol 2006; 4: 101–114.
McMahon LL, Kauer JA . Hippocampal interneurons are excited via serotonin-gated ion channels. J Neurophysiol 1997; 78: 2493–2502.
Shen RY, Andrade R . 5-Hydroxytryptamine2 receptor facilitates GABAergic neurotransmission in rat hippocampus. J Pharmacol Exp Ther 1998; 285: 805–812.
Khan ZU, Gutierrez A, Martin R, Penafiel A, Rivera A, De La Calle A . Differential regional and cellular distribution of dopamine D2-like receptors: an immunocytochemical study of subtype-specific antibodies in rat and human brain. J Comp Neurol 1998; 402: 353–371.
Delgado A, Sierra A, Querejeta E, Valdiosera RF, Aceves J . Inhibitory control of the GABAergic transmission in the rat neostriatum by D2 dopamine receptors. Neuroscience 2000; 95: 1043–1048.
Seamans JK, Gorelova N, Durstewitz D, Yang CR . Bidirectional dopamine modulation of GABAergic inhibition in prefrontal cortical pyramidal neurons. J Neurosci 2001; 21: 3628–3638.
Lebon V, Petersen KF, Cline GW, Shen J, Mason GF, Dufour S et al. Astroglial contribution to brain energy metabolism in humans revealed by 13C nuclear magnetic resonance spectroscopy: elucidation of the dominant pathway for neurotransmitter glutamate repletion and measurement of astrocytic oxidative metabolism. J Neurosci 2002; 22: 1523–1531.
Magistretti PJ, Pellerin L, Rothman DL, Shulman RG . Energy on demand. Science 1999; 283: 496–497.
Auer DP, Putz B, Kraft E, Lipinski B, Schill J, Holsboer F . Reduced glutamate in the anterior cingulate cortex in depression: an in vivo proton magnetic resonance spectroscopy study. Biol Psychiatry 2000; 47: 305–313.
Michael N, Erfurth A, Ohrmann P, Arolt V, Heindel W, Pfleiderer B . Metabolic changes within the left dorsolateral prefrontal cortex occurring with electroconvulsive therapy in patients with treatment resistant unipolar depression. Psychol Med 2003; 33: 1277–1284.
Block W, Traber F, Von Widdern O, Metten M, Schild H, Maier W et al. Proton MR spectroscopy of the hippocampus at 3T in patients with unipolar major depressive disorder: correlates and predictors of treatment response. Int J Neuropsychopharmacol 2009; 12: 415–422.
Walter M, Henning A, Grimm S, Schulte RF, Beck J, Dydak U et al. The relationship between aberrant neuronal activation in the pregenual anterior cingulate, altered glutamatergic metabolism, and anhedonia in major depression. Arch Gen Psychiatry 2009; 66: 478–486.
Milne A, MacQueen GM, Yucel K, Soreni N, Hall GB . Hippocampal metabolic abnormalities at first onset and with recurrent episodes of a major depressive disorder: a proton magnetic resonance spectroscopy study. Neuroimage 2009; 47: 36–41.
Price RB, Shungu DC, Mao X, Nestadt P, Kelly C, Collins KA et al. Amino acid neurotransmitters assessed by proton magnetic resonance spectroscopy: relationship to treatment resistance in major depressive disorder. Biol Psychiatry 2009; 65: 792–800.
Hashimoto K . Emerging role of glutamate in the pathophysiology of major depressive disorder. Brain Res Rev 2009; 61: 105–123.
Machado-Vieira R, Manji HK, Zarate CA . The role of the tripartite glutamatergic synapse in the pathophysiology and therapeutics of mood disorders. Neuroscientist 2009; 15: 525–539.
Yuksel C, Ongur D . Magnetic resonance spectroscopy studies of glutamate-related abnormalities in mood disorders. Biol Psychiatry 2010; 68: 785–794.
Michael N, Erfurth A, Ohrmann P, Arolt V, Heindel W, Pfleiderer B . Neurotrophic effects of electroconvulsive therapy: a proton magnetic resonance study of the left amygdalar region in patients with treatment-resistant depression. Neuropsychopharmacology 2003; 28: 720–725.
Pfleiderer B, Michael N, Erfurth A, Ohrmann P, Hohmann U, Wolgast M et al. Effective electroconvulsive therapy reverses glutamate/glutamine deficit in the left anterior cingulum of unipolar depressed patients. Psychiatry Res 2003; 122: 185–192.
Moghaddam B . Stress activation of glutamate neurotransmission in the prefrontal cortex: implications for dopamine-associated psychiatric disorders. Biol Psychiatry 2002; 51: 775–787.
Bagley J, Moghaddam B . Temporal dynamics of glutamate efflux in the prefrontal cortex and in the hippocampus following repeated stress: effects of pretreatment with saline or diazepam. Neuroscience 1997; 77: 65–73.
Gao SF, Bao AM . Corticotropin-releasing hormone, glutamate, and {gamma}-aminobutyric acid in depression. Neuroscientist 2011; 17: 124–144.
Grace AA . Gating of information flow within the limbic system and the pathophysiology of schizophrenia. Brain Res Brain Res Rev 2000; 31: 330–341.
Sesack SR, Carr DB, Omelchenko N, Pinto A . Anatomical substrates for glutamate-dopamine interactions: evidence for specificity of connections and extrasynaptic actions. Ann N Y Acad Sci 2003; 1003: 36–52.
Rajkowska G, Miguel-Hidalgo JJ . Gliogenesis and glial pathology in depression. CNS Neurol Disord Drug Targets 2007; 6: 219–233.
Lyoo IK, Yoon SJ, Musen G, Simonson DC, Weinger K, Bolo N et al. Altered prefrontal glutamate-glutamine-gamma-aminobutyric acid levels and relation to low cognitive performance and depressive symptoms in type 1 diabetes mellitus. Arch Gen Psychiatry 2009; 66: 878–887.
Choudary PV, Molnar M, Evans SJ, Tomita H, Li JZ, Vawter MP et al. Altered cortical glutamatergic and GABAergic signal transmission with glial involvement in depression. Proc Natl Acad Sci USA 2005; 102: 15653–15658.
Bernard R, Kerman IA, Thompson RC, Jones EG, Bunney WE, Barchas JD et al. Altered expression of glutamate signaling, growth factor, and glia genes in the locus coeruleus of patients with major depression. Mol Psychiatry 2011 (in press).
McCullumsmith RE, Meador-Woodruff JH . Striatal excitatory amino acid transporter transcript expression in schizophrenia, bipolar disorder, and major depressive disorder. Neuropsychopharmacology 2002; 26: 368–375.
Tordera RM, Totterdell S, Wojcik SM, Brose N, Elizalde N, Lasheras B et al. Enhanced anxiety, depressive-like behaviour and impaired recognition memory in mice with reduced expression of the vesicular glutamate transporter 1 (VGLUT1). Eur J Neurosci 2007; 25: 281–290.
Zink M, Vollmayr B, Gebicke-Haerter PJ, Henn FA . Reduced expression of glutamate transporters vGluT1, EAAT2 and EAAT4 in learned helpless rats, an animal model of depression. Neuropharmacology 2010; 58: 465–473.
Chourbaji S, Vogt MA, Fumagalli F, Sohr R, Frasca A, Brandwein C et al. AMPA receptor subunit 1 (GluR-A) knockout mice model the glutamate hypothesis of depression. FASEB J 2008; 22: 3129–3134.
Boyce-Rustay JM, Holmes A . Genetic inactivation of the NMDA receptor NR2A subunit has anxiolytic-and antidepressant-like effects in mice. Neuropsychopharmacology 2006; 31: 2405–2414.
Beneyto M, Kristiansen LV, Oni-Orisan A, McCullumsmith RE, Meador-Woodruff JH . Abnormal glutamate receptor expression in the medial temporal lobe in schizophrenia and mood disorders. Neuropsychopharmacology 2007; 32: 1888–1902.
Feyissa AM, Chandran A, Stockmeier CA, Karolewicz B . Reduced levels of NR2A and NR2B subunits of NMDA receptor and PSD-95 in the prefrontal cortex in major depression. Prog Neuropsychopharmacol Biol Psychiatry 2009; 33: 70–75.
Matrisciano F, Caruso A, Orlando R, Marchiafava M, Bruno V, Battaglia G et al. Defective group-II metaboropic glutamate receptors in the hippocampus of spontaneously depressed rats. Neuropharmacology 2008; 55: 525–531.
Wieronska JM, Branski P, Szewczyk B, Palucha A, Papp M, Gruca P et al. Changes in the expression of metabotropic glutamate receptor 5 (mGluR5) in the rat hippocampus in an animal model of depression. Pol J Pharmacol 2001; 53: 659–662.
Shen J . 13C magnetic resonance spectroscopy studies of alterations in glutamate neurotransmission. Biol Psychiatry 2006; 59: 883–887.
Raichle ME, MacLeod AM, Snyder AZ, Powers WJ, Gusnard DA, Shulman GL . A default mode of brain function. Proc Natl Acad Sci USA 2001; 98: 676–682.
Phillips ML, Drevets WC, Rauch SL, Lane R . Neurobiology of emotion perception II: implications for major psychiatric disorders. Biol Psychiatry 2003; 54: 515–528.
Mayberg HS . Positron emission tomography imaging in depression: a neural systems perspective. Neuroimaging Clin N Am 2003; 13: 805–815.
Mayberg HS . Modulating limbic-cortical circuits in depression: targets of antidepressant treatments. Semin Clin Neuropsychiatry 2002; 7: 255–268.
Mayberg HS . Targeted electrode-based modulation of neural circuits for depression. J Clin Invest 2009; 119: 717–725.
Savitz JB, Drevets WC . Imaging phenotypes of major depressive disorder: genetic correlates. Neuroscience 2009; 164: 300–330.
Fitzgerald PB, Laird AR, Maller J, Daskalakis ZJ . A meta-analytic study of changes in brain activation in depression. Hum Brain Mapp 2008; 29: 683–695.
Price JL, Drevets WC . Neurocircuitry of mood disorders. Neuropsychopharmacology 2009; 35: 192–216.
Drevets WC, Price JL, Furey ML . Brain structural and functional abnormalities in mood disorders: implications for neurocircuitry models of depression. Brain Struct Funct 2008; 213: 93–118.
Savitz J, Drevets WC . Bipolar and major depressive disorder: neuroimaging the developmental-degenerative divide. Neurosci Biobehav Rev 2009; 33: 699–771.
Grimm S, Boesiger P, Beck J, Schuepbach D, Bermpohl F, Walter M et al. Altered negative BOLD responses in the default-mode network during emotion processing in depressed subjects. Neuropsychopharmacology 2009; 34: 932–843.
Hasler G, Fromm S, Carlson PJ, Luckenbaugh DA, Waldeck T, Geraci M et al. Neural response to catecholamine depletion in unmedicated subjects with major depressive disorder in remission and healthy subjects. Arch Gen Psychiatry 2008; 65: 521–531.
Northoff G . Psychopathology and pathophysiology of the self in depression-neuropsychiatric hypothesis. J Affect Disord 2007; 104: 1–14.
Lemogne C, Gorwood P, Bergouignan L, Pelissolo A, Lehericy S, Fossati P . Negative affectivity, self-referential processing and the cortical midline structures. Soc Cogn Affect Neurosci 2011 (in press).
Lemogne C, le Bastard G, Mayberg H, Volle E, Bergouignan L, Lehericy S et al. In search of the depressive self: extended medial prefrontal network during self-referential processing in major depression. Soc Cogn Affect Neurosci 2009; 4: 305–312.
Grimm S, Ernst J, Boesiger P, Schuepbach D, Hell D, Boeker H et al. Increased self-focus in major depressive disorder is related to neural abnormalities in subcortical-cortical midline structures. Hum Brain Mapp 2009; 30: 2617–2627.
Northoff G, Heinzel A, de Greck M, Bermpohl F, Dobrowolny H, Panksepp J . Self-referential processing in our brain--a meta-analysis of imaging studies on the self. Neuroimage 2006; 31: 440–457.
Enzi B, de Greck M, Prosch U, Tempelmann C, Northoff G . Is our self nothing but reward? Neuronal overlap and distinction between reward and personal relevance and its relation to human personality. PLoS One 2009; 4: e8429.
Northoff G, Walter M, Schulte RF, Beck J, Dydak U, Henning A et al. GABA concentrations in the human anterior cingulate cortex predict negative BOLD responses in fMRI. Nat Neurosci 2007; 10: 1515–1517.
Muthukumaraswamy SD, Edden RA, Jones DK, Swettenham JB, Singh KD . Resting GABA concentration predicts peak gamma frequency and fMRI amplitude in response to visual stimulation in humans. Proc Natl Acad Sci USA 2009; 106: 8356–8361.
Northoff G, Qin P, Nakao T . Rest-stimulus interaction in the brain: a review. Trends Neurosci 2010; 33: 277–284.
Levinson AJ, Fitzgerald PB, Favalli G, Blumberger DM, Daigle M, Daskalakis ZJ . Evidence of cortical inhibitory deficits in major depressive disorder. Biol Psychiatry 2010; 67: 458–464.
Bajbouj M, Lang UE, Neu P, Heuser I . Therapeutic brain stimulation and cortical excitability in depressed patients. Am J Psychiatry 2005; 162: 2192–2193.
Sanacora G . Cortical inhibition, gamma-aminobutyric acid, and major depression: there is plenty of smoke but is there fire? Biol Psychiatry 2010; 67: 397–398.
Morgane PJ, Galler JR, Mokler DJ . A review of systems and networks of the limbic forebrain/limbic midbrain. Prog Neurobiol 2005; 75: 143–160.
Meyer-Lindenberg A . Neural connectivity as an intermediate phenotype: brain networks under genetic control. Hum Brain Mapp 2009; 30: 1938–1946.
Meyer-Lindenberg A, Weinberger DR . Intermediate phenotypes and genetic mechanisms of psychiatric disorders. Nat Rev Neurosci 2006; 7: 818–827.
Meyer-Lindenberg AS, Olsen RK, Kohn PD, Brown T, Egan MF, Weinberger DR et al. Regionally specific disturbance of dorsolateral prefrontal-hippocampal functional connectivity in schizophrenia. Arch Gen Psychiatry 2005; 62: 379–386.
Esslinger C, Walter H, Kirsch P, Erk S, Schnell K, Arnold C et al. Neural mechanisms of a genome-wide supported psychosis variant. Science 2009; 324: 605.
Anand A, Li Y, Wang Y, Wu J, Gao S, Bukhari L et al. Activity and connectivity of brain mood regulating circuit in depression: a functional magnetic resonance study. Biol Psychiatry 2005; 57: 1079–1088.
Anand A, Li Y, Wang Y, Lowe MJ, Dzemidzic M . Resting state corticolimbic connectivity abnormalities in unmedicated bipolar disorder and unipolar depression. Psychiatry Res 2009; 171: 189–198.
Bluhm R, Williamson P, Lanius R, Theberge J, Densmore M, Bartha R et al. Resting state default-mode network connectivity in early depression using a seed region-of-interest analysis: decreased connectivity with caudate nucleus. Psychiatry Clin Neurosci 2009; 63: 754–761.
Seminowicz DA, Mayberg HS, McIntosh AR, Goldapple K, Kennedy S, Segal Z et al. Limbic-frontal circuitry in major depression: a path modeling metanalysis. Neuroimage 2004; 22: 409–418.
James GA, Kelley ME, Craddock RC, Holtzheimer PE, Dunlop BW, Nemeroff CB et al. Exploratory structural equation modeling of resting-state fMRI: applicability of group models to individual subjects. Neuroimage 2009; 45: 778–787.
Sheline YI, Price JL, Yan Z, Mintun MA . Resting-state functional MRI in depression unmasks increased connectivity between networks via the dorsal nexus. Proc Natl Acad Sci USA 2010; 107: 11020–11025.
Zhou Y, Yu C, Zheng H, Liu Y, Song M, Qin W et al. Increased neural resources recruitment in the intrinsic organization in major depression. J Affect Disord 2010; 121: 220–230.
Horn DI, Yu C, Steiner J, Buchmann J, Kaufmann J, Osoba A et al. Glutamatergic and resting-state functional connectivity correlates of severity in major depression-the role of pregenual anterior cingulate cortex and anterior insula. Front Syst Neurosci 2010; 4: 1–10.
Greicius MD, Flores BH, Menon V, Glover GH, Solvason HB, Kenna H et al. Resting-state functional connectivity in major depression: abnormally increased contributions from subgenual cingulate cortex and thalamus. Biol Psychiatry 2007; 62: 429–437.
Johansen-Berg H, Gutman DA, Behrens TE, Matthews PM, Rushworth MF, Katz E et al. Anatomical connectivity of the subgenual cingulate region targeted with deep brain stimulation for treatment-resistant depression. Cereb Cortex 2008; 18: 1374–1383.
Hamilton JP, Chen G, Thomason ME, Schwartz ME, Gotlib IH . Investigating neural primacy in major depressive disorder: multivariate granger causality analysis of resting-state fMRI time-series data. Mol Psychiatry 2011 (in press).
Greicius MD, Supekar K, Menon V, Dougherty RF . Resting-state functional connectivity reflects structural connectivity in the default mode network. Cereb Cortex 2009; 19: 72–78.
Glahn DC, Winkler AM, Kochunov P, Almasy L, Duggirala R, Carless MA et al. Genetic control over the resting brain. Proc Natl Acad Sci USA 2010; 107: 1223–1228.
Liu Z, Xu C, Xu Y, Wang Y, Zhao B, Lv Y et al. Decreased regional homogeneity in insula and cerebellum: a resting-state fMRI study in patients with major depression and subjects at high risk for major depression. Psychiatry Res 2010; 182: 211–215.
Northoff G, Kotter R, Baumgart F, Danos P, Boeker H, Kaulisch T et al. Orbitofrontal cortical dysfunction in akinetic catatonia: a functional magnetic resonance imaging study during negative emotional stimulation. Schizophr Bull 2004; 30: 405–427.
Frodl T, Bokde AL, Scheuerecker J, Lisiecka D, Schoepf V, Hampel H et al. Functional connectivity bias of the orbitofrontal cortex in drug-free patients with major depression. Biol Psychiatry 2010; 67: 161–167.
Hamilton JP, Gotlib IH . Neural substrates of increased memory sensitivity for negative stimuli in major depression. Biol Psychiatry 2008; 63: 1155–1162.
Yoshimura S, Ueda K, Suzuki S, Onoda K, Okamoto Y, Yamawaki S . Self-referential processing of negative stimuli within the ventral anterior cingulate gyrus and right amygdala. Brain Cogn 2009; 69: 218–225.
Schlosser RG, Wagner G, Koch K, Dahnke R, Reichenbach JR, Sauer H . Fronto-cingulate effective connectivity in major depression: a study with fMRI and dynamic causal modeling. Neuroimage 2008; 43: 645–655.
Vasic N, Walter H, Sambataro F, Wolf RC . Aberrant functional connectivity of dorsolateral prefrontal and cingulate networks in patients with major depression during working memory processing. Psychol Med 2009; 39: 977–987.
Salvadore G, Cornwell BR, Sambataro F, Latov D, Colon-Rosario V, Carver F et al. Anterior cingulate desynchronization and functional connectivity with the amygdala during a working memory task predict rapid antidepressant response to ketamine. Neuropsychopharmacology 2010; 35: 1415–1422.
Friedel E, Schlagenhauf F, Sterzer P, Park SQ, Bermpohl F, Strohle A et al. 5-HTT genotype effect on prefrontal-amygdala coupling differs between major depression and controls. Psychopharmacology (Berl) 2009; 205: 261–271.
Chamberlain SR, Sahakian BJ . The neuropsychology of mood disorders. Curr Psychiatry Rep 2006; 8: 458–463.
Konopka RJ, Benzer S . Clock mutants of Drosophila melanogaster. Proc Natl Acad Sci USA 1971; 68: 2112–2116.
Takahashi JS, Shimomura K, Kumar V . Searching for genes underlying behavior: lessons from circadian rhythms. Science 2008; 322: 909–912.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
PowerPoint slides
Rights and permissions
About this article
Cite this article
Hasler, G., Northoff, G. Discovering imaging endophenotypes for major depression. Mol Psychiatry 16, 604–619 (2011). https://doi.org/10.1038/mp.2011.23
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/mp.2011.23
Keywords
This article is cited by
-
Deletion of Crtc1 leads to hippocampal neuroenergetic impairments associated with depressive-like behavior
Molecular Psychiatry (2022)
-
Sequential fear generalization and network connectivity in trauma exposed humans with and without psychopathology
Communications Biology (2022)
-
Activation of SIRT-1 Signalling in the Prevention of Bipolar Disorder and Related Neurocomplications: Target Activators and Influences on Neurological Dysfunctions
Neurotoxicity Research (2022)
-
Associations between childhood family emotional health, fronto-limbic grey matter volume, and saliva 5mC in young adulthood
Clinical Epigenetics (2021)
-
Understanding personalized dynamics to inform precision medicine: a dynamic time warp analysis of 255 depressed inpatients
BMC Medicine (2020)