Key summary points
To synthesize the details of the exercises prescribed for the improvement of muscle mass/muscle strength/physical performance among sarcopenic older adults.
AbstractSection FindingsFrequency, intensity, duration, type, mode, and progression while prescribing resistance, aerobic, balance, and flexibility exercises for sarcopenic older adults were identified and reported.
AbstractSection MessageA multicomponent exercise program targeting muscle strength, aerobic, balance, and flexibility are recommended and tailored as per the existing fitness level and targeted outcomes for sarcopenic older adults.
Abstract
Purpose
To synthesize the details of the exercises/exercise program prescribed for the improvement of muscle mass/muscle strength/physical performance among sarcopenic older adults.
Methods
A systematic literature search was conducted in five electronic databases and the details of exercises such as single component or multicomponent exercise program, frequency/week, intensity, duration of the exercise program, type of exercises, progression, adverse events reported, outcome measures used, and whether technology or other educational aids were used to deliver the program were extracted.
Results
A total of 10,045 records were identified and 27 records were included. Resistance exercises were included in all the studies, with the frequency ranging from 1 to 5/week, intensity ranging from 20 to 80% of 1 repetition maximum (RM), or 6–14 points on ratings of perceived exertion (RPE), and duration per session ranging from 20 to 75 min. The intensity of aerobic exercises ranged from 50 to 70% of heart rate max or a level of 7–17 in RPE with a duration ranging from 6 to 30 min per session for 2–5 days/week. For balance exercises, the intensity was mentioned as the level of effort 3 on a scale of 10, and the time duration per session ranged from 5 to 30 min for a frequency of 2/3 per week.
Conclusion
This review synthesized the components of exercise prescription for sarcopenic older adults which would help practitioners and researchers in selecting the frequency, intensity, duration, type, mode, and progression while prescribing exercises.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sarcopenia among older adults is a disorder that causes a gradual loss of skeletal muscle mass, strength, and deterioration in physical performance [1,2,3]. The prevalence of sarcopenia ranges from 9 to 10% among community-dwelling older adults, 23–24% among hospitalized people, and 30–50% among residents of long-term care settings, and its incidence increases with age [4, 5]. A plethora of factors contribute to the development of sarcopenia among older adults, including sedentary lifestyle, changes in endocrine function (insulin, testosterone, growth hormone, insulin-like growth factor-1, cortisol), loss of neuromuscular function, an imbalance between muscle protein synthesis and breakdown, insufficient dietary protein intake, and genetic factors [6, 7].
Sarcopenia is concerning as it leads to negative health outcomes in older people, such as falls, frailty, physical restrictions, activity limitations, lower quality of life, and an increased risk of premature death [8,9,10,11]. The European Working Group for Sarcopenia in Older People (EWGSOP) and Asian Working Group for Sarcopenia (AWGS) have come up with the diagnostic criteria for sarcopenia among older adults, which considers muscle mass, muscle strength, and physical performance parameters with slight variations in the cutoff values [2, 3]. Among the pharmacological and non-pharmacological management options, the highest evidence exists for a multicomponent program involving exercises as the mainstay [12, 13]. However, there is a conflict among practitioners/clinicians and in literature with regard to the details of the exercise programs, and a review targeting the components of exercises for sarcopenia among older adults is lacking. This literature review aims to synthesize the details of the exercises/exercise program prescribed for the improvement of muscle mass/muscle strength/physical performance among sarcopenic older adults.
Methods
Eligibility criteria
The studies were included if they met the criteria: (a) original study, (b) on older adults, (c) including those diagnosed with sarcopenia, (d) with study design such as pilot study, randomized controlled trial, pre–post intervention trial, or longitudinal studies, (e) single-component or multicomponent exercise-based intervention. The studies were excluded if they failed to meet the inclusion criteria and/or: (a) full text was not available, (b) language was other than English, (c) was a single/multiple component intervention in which exercise was not a component, (d) studies providing no extractable data, and (e) patients had secondary sarcopenia due to conditions like COPD, cancer, kidney disease, stroke, Parkinson’s disease, and Alzheimer's disease.
Data sources and search strategy
A systematic literature search was undertaken in December 2021 using the following electronic databases: PubMed, Scopus, Embase, Cumulated Index to Nursing and Allied Health Literature (CINAHL), and Web of Science. Relevant MeSH terms and Boolean phases were used for the search: “sarcopenia” OR “reduced skeletal muscle mass” OR “muscle mass loss” OR “muscle atrophy” AND “aged” OR “elderly” OR “older adults” OR “older people” AND “physical therapy” OR “rehabilitation programme” OR “therapeutic exercise” AND “residential care facilities” OR “long-term care facilities” OR “old age homes” without time restrictions and no filters were applied. The complete search strategy for each database is shown in the supporting information (search strategy.pdf).
Data extraction
Two reviewers, PK and GN, independently searched the literature. The identified studies were imported to Rayyan (Ref. # 366956) software. After resolving the duplicates, two reviewers (PK and GN) conducted title and abstract screening separately. If the study was deemed suitable, it progressed to the retrieval of the full text. If, after a review of the full text, the article was still considered suitable for the analysis, then it progressed to data extraction. Any conflict regarding the article selection was resolved by discussion with the third reviewer, SU. Full-text reading of the identified articles was done by PK, and relevant studies were included in this review matching our inclusion criteria. The data charting form was drafted by PK as per the American College of Sports Medicines’ (ACSM) [14] frequency, intensity, time and type principle (FITT principle) and finalized after a consensus discussion with all the authors. The details of exercises like a single-component or multicomponent exercise program, frequency/week, intensity, duration/session, total duration of the exercise program, type of exercises, progression, adverse events reported, outcome measures used, and whether technology or other educational aids were used to deliver the program were extracted.
Results
Search results
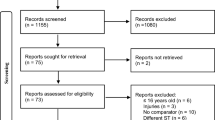
A total of 10,045 studies were identified through database searches. After removing duplicate studies, the titles and abstracts of 5,372 studies were screened. A review of the titles and abstracts yielded 314 relevant studies for full-text screening. Finally, 27 studies met all inclusion criteria and included in this review. A Preferred Reporting Items for Systematic Review and Meta-analysis 2020 (PRISMA 2020) flowchart of the literature search is demonstrated in Fig. 1.
Nine studies used Asian Working Group for Sarcopenia 2014 (AWGS 2014) criteria [15,16,17,18,19,20,21,22,23], one study each used AWGS 2016 [24] and AWGS 2019 criteria [25], six studies used European Working Group for Sarcopenia in Older People (EWGSOP 2010) criteria [26,27,28,29,30,31], one study used EWGSOP 2019 criteria [32], one study used Center for Disease Control and Prevention criteria [33], one used International Working Group on Sarcopenia (IWGS) along with EWGSOP 2010 criteria [34] and seven studies did not report any of the above-mentioned criteria [35,36,37,38,39,40,41].
Twenty-seven studies, which used exercise intervention in single- and multicomponent modes, were included in this review. Out of 27, in 16 studies (n = 16), the exercise intervention was given as a single component with all studies using resistance exercise [15, 19,20,21,22,23, 25,26,27, 29, 31, 32, 34, 37, 38, 40], while the remaining 11 studies (n = 11) administered multicomponent exercise intervention [16,17,18, 24, 28, 30, 33, 35, 36, 39, 41]. Among the multicomponent exercise interventions, resistance exercise plus balance exercise were administered in four studies (n = 4) [16, 18, 28, 41]; resistance exercise plus aerobic exercise in three studies (n = 3) [24, 30, 36], resistance exercise plus aerobic exercise plus balance exercise in one study (n = 1) [39]; resistance exercise plus aerobic exercise plus balance exercise plus flexibility exercise in two studies (n = 2) [17, 33]; resistance exercise plus balance exercise plus aerobic exercise plus endurance exercise in one study (n = 1) [35]. In 25 studies (n = 25), a supervised exercise program [15, 17, 18, 20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41], in one study (n = 1) an unsupervised exercise program [16], and in one study, (n = 1) an initial training was administered and then participants performed exercise unsupervised [19].
The details of the exercise program are summarized in Tables 1, 2, 3, and 4 for resistance exercises, aerobic and endurance exercises, balance exercises, and stretching exercises, respectively.
Of the 27 studies on resistance exercises, 9 studies (n = 9) used repetition maximum (RM) criteria [18, 25, 27, 29, 30, 32, 36, 37, 40], whereas 10 studies (n = 10) used rating of perceived exertion (RPE) [15, 19, 21, 23, 26, 28, 31, 38, 39, 41] criteria to quantify the intensity of resistance training. One study each (n = 1) used OMNI-RES scale (OMNI-Rating of perceived Exertion scale) [34], heart rate reserve criteria [20] or coach-adjusted resistance criteria [24], and maximal theoretical force [33] while four studies (n = 4) [16, 17, 22, 35] did not report the method used for intensity measurement. The percentage of 1RM, which ranged from 20 to 80% of 1RM, was used by all the nine studies that used RM criteria, and of the 10 studies (n = 10) that used RPE, it ranged from 6 to 14 points. The frequency/week of resistance training ranged from 1 to 5/week. Eight studies (n = 8) administered resistance training two/week [15, 18, 28,29,30, 32, 33, 41], 14 studies (n = 14) three/week [20,21,22,23,24,25,26,27, 31, 34,35,36,37,38], 1 study (n = 1) each one [40] and five per week [19], respectively. A total of three studies (n = 3) did not report the frequency of resistance training [16, 17, 39]. The duration per session ranged from a minimum of 20 to a maximum of 75 min and the total duration of the intervention program ranged from 6 to 32 weeks. The progression of resistance exercise has been reported in 22 studies (n = 22), among which 9 (n = 9) [18, 25, 27, 28, 30, 32, 33, 36, 40] reported progression in terms of the number of sets, repetition per set, and intensity, either RM or RPE, 2 studies (n = 2) [34, 37] reported progress in resistance exercise using OMNI, 10 studies (n = 10) [15, 17, 19, 21, 22, 26, 29, 31, 38, 41] reported progression with respect to the loading method, and 1 study (n = 1) [20] reported in terms of duration/session. A total of five studies (n = 5) [16, 23, 24, 35, 39] did not report the progression of resistance training.
Seven studies (n = 7) [17, 24, 30, 33, 35, 36, 39] used aerobic and endurance exercises as a multicomponent exercise intervention program. Of the seven studies, two (n = 2) [30, 33] used the percentage of heart rate maximum (HR max), two (n = 2) [36, 39] used RPE criteria for quantifying the intensity of aerobic exercises, and the remaining three studies (n = 3) [17, 24, 35] did not report how the intensity was monitored. The duration of aerobic exercises ranged from 6 to 30 min per session for 2–5 days/week. Among the aerobic and endurance studies included in this review, only one study (n = 1) [36] reported exercise progression in terms of time/session, intensity, and rating of perceived exertion.
Balance exercises were used as a component of the multicomponent program in nine studies (n = 9) [16,17,18, 22, 28, 33, 35, 39, 41] and among those only one (n = 1) reported the intensity of balance exercises [39]. The level of effort was mentioned as 3 on a scale of 10, and the time duration per session ranged from 5 to 30 min for a frequency of 2/3 per week. Only two studies (n = 2) included in this review mentioned the progression of the balance exercise on the bases of weeks and challenging exercise [18, 28]. Two studies (n = 2) [17, 33] mentioned stretching exercises for sarcopenic older adults, and among those one [17] did not report the details, whereas the other [33] mentioned stretching exercises of the lower limb muscles. However, further exercise prescription components such as frequency, intensity, time, and type of stretches were not reported in both studies.
We have proposed the recommendation which the practitioner and researcher could use while prescribing exercise program for sarcopenic older adults in Table 5.
Discussion
This rapid review intended to synthesize the details of the exercises/exercise program prescribed for the improvement of either muscle mass or muscle strength or physical performance among sarcopenic older adults residing in either long-term care setting or in the community. A total of 27 records were summarized with regard to the details of exercises such as a single-component or multicomponent exercise program, frequency/week, intensity, duration/session, total duration of the exercise program, type of exercises, progression, adverse events reported, outcome measures used, and whether technology or other educational aids were used to deliver the program. Also, the Consensus on Exercise Reporting Template (CERT) [42] was used to evaluate the completeness of exercise reporting of the studies included in this review. Most of the studies reported the details of each exercise included in the intervention to enable replication. The exercise progression details were reported well in many of the studies, with most exercise interventions being supervised. However, the way the exercise interventions were tailored were not reported in many of the studies (Supplementary material).
Given that the studies did not use uniform diagnostic criteria for sarcopenia, the prevalence varied greatly from 10 to 30% [43] depending on the classification and cutoff point chosen. The participants in the studies included in this review may be heterogenous with regard to their fitness profile and exercise capacity. Hence, the compilation of the results of these studies would be difficult and the effectiveness of the program has to be interpreted with caution. However, there are systematic reviews that give evidence about the effect of exercise on sarcopenia management. According to the findings of those systematic reviews, the best evidence exists for multimodal or mixed training programs that include resistance training, aerobic training, and balance training, with a moderate level of evidence for resistance training alone in enhancing muscle mass, muscle strength, and physical performance in sarcopenic older persons. There was a low level of evidence for flexibility or balance alone programs, as the number of studies were limited [44,45,46,47,48].
Eleven studies in this review used multicomponent exercise interventions for the management of sarcopenic older adults. Since there are no exercise recommendations or guidelines for the management of sarcopenia, most of the authors have followed the recommendations for physical frailty that report the beneficial effects of a multicomponent over a single-component intervention [49]. Currently, there is a lack of consensus among practitioners with regard to the dosage of resistance training that is required to get the best results in terms of muscular strength. The frequency per week of resistance training in the studies in this review ranged from a minimum of 2 days to a maximum of 5 days per week, with most of the authors preferring 3 days per week. Two reviews were conducted on the components of exercise prescription for frail older adults and on patients with knee osteoarthritis (OA), which recommended a similar frequency of resistance exercises with significant improvements in muscle strength documented with a training frequency of 2–3 days [49, 50].
Aerobic and endurance studies (n = 7) included in this review are part of a multicomponent exercise intervention. The frequency of aerobic exercises for sarcopenia ranged from two to five times per week. The American College of Sports Medicine physical activity recommendation for older adults states 3–5 days per week of aerobic activity, and for older adults with knee OA, the most common recommendation that exists is to perform 3–5 days per week of cardiorespiratory training [50, 51]. Even though the minimum recommended frequency is 3 days per week, a few studies of this review have used 2 days per week; however, the effect of 2 days over 3 days per week training needs to be studied. Balance exercises have been carried out in nine studies (n = 9) of this review, in which the frequency was found to be two to three times per week, which is the same in the case of older frail adults as well for older adults with knee OA [49, 50]. Also, the US Department of Health and Human Services (2008) Physical Activity Guidelines for Americans recommends three or more times per week of balance training. For stretching exercises, even though frequency was not reported, it was a part of warm-up in most of the studies. However, one of the study recommends two to three times per week of flexibility exercises for frail older adults (41).
The intensity of resistance exercises for sarcopenic older adults ranged from 20 to 79% of 1 RM or 6 to 14 RPE in the studies included in this review. For frail older adults as per the literature, the intensity varies from 40 to 80% 1RM or somewhat hard (12–14) RPE [49]. The literature suggests that 60–80% of 1RM improves the muscle mass, while more than 80% of 1RM will further improve the muscle strength at the cost of musculoskeletal injuries [51]. The intensity of aerobic exercise prescribed for sarcopenic older adults ranged from 50 to 70% of HRmax or 7–17 on RPE, which is in line with the recommendation of ACSM/AHA that recommends moderate- to vigorous-intensity aerobic exercise for older adults. In this review, only one study (n = 1) reported the intensity of balance exercise, which is 3 on a rating of perceived exertion and this corresponds to the recommendations for frail older adults [49].
The duration for resistance exercise ranged from a minimum of 20 min to a maximum of 75 min in the included studies. A study has mentioned that the duration for resistance exercise ranged from 10 min for frail and 20 min for pre-frail older adults [49]. The duration of aerobic exercise per session for sarcopenic older adults reported in the studies in this review ranged from 6 to 30 min per session. As per the ACSM recommendation, moderate-intensity aerobic exercise should be performed for ≥ 30 min per day or vigorous-intensity exercise for ≥ 20 min per day [14]. The duration of balance exercise in the included studies ranged from 6 to 30 min, which covers the time prescribed for frail older adults of 20 min.
The type and mode of exercise should be chosen based on the participant's level of fitness, as well as his or her interests and available resources for better compliance and for lowering the risk of injury [51, 52]. The type of resistance training delivered in the included studies is related to training the large muscle groups of the upper limb and lower limb along with the trunk. These are in line with the recommendations by other studies as well, which recommends resistance training to be directed at the large muscle groups that are important in everyday activities incorporating arms/shoulders, chest, back, hips, and legs [14, 50, 51, 53]. Aerobic and endurance exercises have been delivered as walking, stepping, and cycle ergometry. Walking is the most popular activity among senior citizens because it requires no special skills, attire, or equipment [52]. For those with musculoskeletal problem, cycling has been preferred over walking and jogging [51]. A similar type of exercise for improving cardiorespiratory fitness has been recommended for older adults with knee OA [50]. In the included studies in this review, stretching is used as part of a warm-up/cool-down in multicomponent training program, with only one study targeted specifically. Stretching of upper, trunk, and lower limb has been suggested, in line with the recommendation by ACSM as it reduces the chance of injury among older adults [53].
The progression of resistance training reported in the studies included in this review suggests starting with a fewer number of sets, higher repetition with less intensity progression, to more sets with less number of repetitions. An author has recommended that clinicians should start their clients with higher repetitions, that is, 12–15, and at a lower intensity (55% of 1RM) and eventually progress to fewer repetitions of 4–6 at a greater intensity (> 80% of 1RM) [49]. Aerobic and endurance studies included only one study (n = 1) [36] in this review, which reported the endurance exercise progression in terms of increasing time/session and increasing intensity as HRmax with higher rating of perceived exertion. Mazzeo et al. [51] recommended starting exercise with low intensity and gradually progressing to higher levels according to tolerance and preference. Only two studies (n = 2) included in this review have mentioned about the progression of balance exercise on the basis of weeks and challenging exercise. A similar recommendation by the US Department of Health and Human Services (2008) Physical Guidelines for Americans says progressively difficult postures gradually reduce the base of support and dynamic movements perturb the center of gravity and stress the postural muscle groups [54].
Among the included studies, n = 4 were study protocols and n = 23 were completed studies. Of these 23 studies, n = 15 studies did not assess for any adverse events [16, 18, 20, 21, 23, 27, 33,34,35,36,37,38,39,40,41], n = 5 studies reported no adverse events [15, 17, 24, 28, 30], and only n = 3 studies reported adverse events because of exercise intervention [19, 26, 31]. Muscle pain, joint pain, fatigue, vertigo, and fall were the commonly reported events.
None of the studies in this review has reported a novel or a non-traditional exercise, except one study that incorporated a BFR program (blood flow restriction) [25], which we feel is a non-conventional mode of training for improving muscle strength or muscle mass. This review did not identify a study that has adopted a tailor-made exercise program with regard to the stages of sarcopenia; hence, the authors of this review recommend designing an exercise program as per the stage of sarcopenia with appropriate progression guidelines.
In this paper, the researchers have synthesized the components of the exercises/exercise program prescribed for the improvement of muscle mass/muscle strength/physical performance among sarcopenic older adults.
Limitations
There are a few limitations to this review. First and foremost, this review has considered only the published articles available in electronic databases. Second, it considered only full-text articles as abstracts, and proceedings were excluded.
Future recommendations
This review has done a narrative summarization of the details of the exercise for sarcopenia. In the future a systematic review with a meta-analysis could be conducted to quantify the efficacy of the exercise program. Since there are more than two types of exercises to be compared for their effect, the authors would recommend performing a network meta-analysis. Also, studies published in non-electronic databases and on gray literature could be carried out as an update to this review.
Significance of this review
This review has synthesized the exercise components and has come up with the exercise recommendations that would benefit the interdisciplinary team to assess, design, and appraise safe and effective exercise programs for sarcopenic older adults. The exercises identified in this review are multicomponent and multimodal in nature, giving the practitioners and researchers the freedom to choose, as per the need and available resources. Also, strategies to improve and maintain adherence to exercise-based intervention have been identified, which need to be incorporated. Moreover, this review has summarized the exercises using the CERT checklist, making the recommendations replicable and transferrable across a variety of settings (hospital, gym, home, primary care, etc.); delivery methods (group, individualized, supervised, or home based), and personnels (physiotherapist,, exercise physiologist,, trainers, or others).
Conclusion
This review would help practitioners and researchers in selecting the frequency, intensity, duration, type, mode, and progression while prescribing exercises for sarcopenic older adults. Also, this review may assist in identifying the variations in the components of exercise prescription for sarcopenic older adults as per the targeted outcome.
Change history
04 August 2023
A Correction to this paper has been published: https://doi.org/10.1007/s41999-023-00844-4
References
Rosenberg IH (1997) Sarcopenia: origins and clinical relevance. J Nutr 127:990S-991S
Cruz-Jentoft AJ, Bahat G, Bauer J et al (2019) Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing 48:16–31
Chen L-K, Woo J, Assantachai P et al (2020) Asian Working Group for Sarcopenia: 2019 consensus update on sarcopenia diagnosis and treatment. J Am Med Dir Assoc 21:300–307
Cruz-Jentoft AJ, Landi F, Schneider SM et al (2014) Prevalence of and interventions for sarcopenia in ageing adults: a systematic review. Report of the International Sarcopenia Initiative (EWGSOP and IWGS). Age Ageing 43:748–759
Papadopoulou SK, Tsintavis P, Potsaki G et al (2020) Differences in the prevalence of sarcopenia in community-dwelling, nursing home and hospitalized individuals. A systematic review and meta-analysis. J Nutr Health Aging 24:83–90
Roubenoff R (2000) Sarcopenia and its implications for the elderly. Eur J Clin Nutr 54:S40–S47
Tournadre A, Vial G, Capel F et al (2019) Sarcopenia. Joint Bone Spine 86:309–314
Chang K-V, Hsu T-H, Wu W-T et al (2016) Association between sarcopenia and cognitive impairment: a systematic review and meta-analysis. J Am Med Dir Assoc 17:1164-e7
Bone AE, Hepgul N, Kon S et al (2017) Sarcopenia and frailty in chronic respiratory disease: Lessons from gerontology. Chron Respir Dis 14:85–99
Schaap LA, Van Schoor NM, Lips P et al (2018) Associations of sarcopenia definitions, and their components, with the incidence of recurrent falling and fractures: the longitudinal aging study Amsterdam. J Gerontol Ser A 73:1199–204
Beaudart C, Locquet M, Reginster J-Y et al (2018) Quality of life in sarcopenia measured with the SarQoL®: impact of the use of different diagnosis definitions. Aging Clin Exp Res 30:307–13
Morley JE (2016) Frailty and sarcopenia in elderly. Wien Klin Wochenschr 128:439–45
Pascual-Fernández J, Fernández-Montero A, Córdova-Martínez A et al (2020) Sarcopenia: molecular pathways and potential targets for intervention. Int J Mol Sci 21:8844
Nelson ME, Rejeski WJ, Blair SN et al (2007) Physical activity and public health in older adults: recommendation from the American College of Sports Medicine and the American Heart Association. Circulation 116:1094
Osuka Y, Kojima N, Sasai H et al (2021) Effects of exercise and/or β-hydroxy-β-methylbutyrate supplementation on muscle mass, muscle strength, and physical performance in older women with low muscle mass: a randomized, double-blind, placebo-controlled trial. Am J Clin Nutr 114:1371–85
Maruya K, Asakawa Y, Ishibashi H et al (2016) Effect of a simple and adherent home exercise program on the physical function of community dwelling adults sixty years of age and older with pre-sarcopenia or sarcopenia. J Phys Ther Sci 28:3183–8
Makizako H, Nakai Y, Tomioka K et al (2020) Effects of a multicomponent exercise program in physical function and muscle mass in sarcopenic/pre-sarcopenic adults. J Clin Med 9:1386
Liang Y, Wang R, Jiang J et al (2020) A randomized controlled trial of resistance and balance exercise for sarcopenic patients aged 80–99 years. Sci Rep 10:1–7
Kuptniratsaikul V, Thanakiatpinyo T, Pongratanakul R et al (2021) Efficacy and safety of a simple home-based resistance exercise program for older adults with low muscle mass: a prospective longitudinal clinical trial. Int J Rehabil Res 44:241–7
Jung WS, Kim YY, Park HY (2019) Circuit training improvements in Korean women with Sarcopenia. Percept Mot Skills 126:828–42
Jeon YK, Shin MJ, Kim CM et al (2018) Effect of Squat Exercises on Lung Function in Elderly Women with Sarcopenia. J Clin Med. https://doi.org/10.3390/jcm7070167
Chow SKH, Chim YN, Cheng KYK et al (2020) Elastic-band resistance exercise or vibration treatment in combination with hydroxymethylbutyrate (HMB) supplement for management of sarcopenia in older people: a study protocol for a single-blinded randomised controlled trial in Hong Kong. BMJ Open. https://doi.org/10.1136/bmjopen-2019-034921
Chiang FY, Chen JR, Lee WJ et al (2021) Effects of milk or soy milk combined with mild resistance exercise on the muscle mass and muscle strength in very old nursing home residents with sarcopenia. Foods. https://doi.org/10.3390/foods10112581
Zhu LY, Chan R, Kwok T et al (2019) Effects of exercise and nutrition supplementation in community-dwelling older Chinese people with sarcopenia: a randomized controlled trial. Age Ageing 48:220–8
Chen N, He XF, Zhao GY et al (2021) Efficacy of low-load resistance training combined with blood flow restriction vs. high-load resistance training on sarcopenia among community-dwelling older Chinese people: study protocol for a 3-arm randomized controlled trial. Trials. https://doi.org/10.1186/s13063-021-05495-z
Vikberg S, Sörlén N, Brandén L et al (2019) Effects of resistance training on functional strength and muscle mass in 70-year-old individuals with pre-sarcopenia: a randomized controlled trial. J Am Med Dir Assoc 20:28–34
Ude Viana J, Domingues Dias JM, Parreira Batista P et al (2018) Effect of a resistance exercise program for sarcopenic elderly women: quasi-experimental study. Fisioter Em Mov 31:1–9
Hassan BH, Hewitt J, Keogh JWL et al (2016) Impact of resistance training on sarcopenia in nursing care facilities: A pilot study. Geriatr Nur (Lond) 37:116–21
Granic A, Hurst C, Dismore L et al (2019) Milk and resistance exercise intervention to improve muscle function in community-dwelling older adults at risk of sarcopenia (MIlkMAN): protocol for a pilot study. BMJ Open 9:e031048
Chang KV, Wu WT, Huang KC et al (2021) Effectiveness of early versus delayed exercise and nutritional intervention on segmental body composition of sarcopenic elders—a randomized controlled trial. Clin Nutr Edinb Scotl 40:1052–9
Martín Del Campo Cervantes J, Habacuc Macías Cervantes M, Monroy Torres R (2019) Effect of a resistance training program on sarcopenia and functionality of the older adults living in a nursing home. J Nutr Health Aging 23:829–36
Laddu D, Kim H, Phillips SA et al (2021) INERTIA: a pilot study of the impact of progressive resistance training on blood pressure control in older adults with sarcopenia. Contemp Clin Trials 108:106516
Bellomo RG, Iodice P, Maffulli N et al (2013) Muscle strength and balance training in sarcopenic elderly: a pilot study with randomized controlled trial. Eur J Inflamm 11:193–201
Seo MW, Jung SW, Kim SW et al (2021) Effects of 16 weeks of resistance training on muscle quality and muscle growth factors in older adult women with sarcopenia: a randomized controlled trial. Int J Environ Res Public Health. https://doi.org/10.3390/ijerph18136762
Najafi Z, Kooshyar H, Mazloom R et al (2018) The effect of fun physical activities on sarcopenia progression among elderly residents in nursing homes: a randomized controlled trial. J Caring Sci 7:137–42
Moghadam BH, Bagheri R, Ashtary-Larky D et al (2020) The effects of concurrent training order on satellite cell-related markers, body composition, muscular and cardiorespiratory fitness in older men with sarcopenia. J Nutr Health Aging 24:796–804
Letieri RV, Furtado GE, Barros PMN et al (2019) Effect of 16-week blood flow restriction exercise on functional fitness in sarcopenic women: a randomized controlled. Int J Morphol 37:59–64
Hong J, Kim J, Kim SW et al (2017) Effects of home-based tele-exercise on sarcopenia among community-dwelling elderly adults: Body composition and functional fitness. Exp Gerontol 87:33–9
Caballero-García A, Pascual-Fernández J, Noriega-González DC et al (2021) L-citrulline supplementation and exercise in the management of sarcopenia. Nutrients. https://doi.org/10.3390/nu13093133
Sousa N, Mendes R, Abrantes C et al (2013) Is once-weekly resistance training enough to prevent sarcopenia? J Am Geriatr Soc 61:1423–4
Kim HK, Suzuki T, Saito K et al (2012) Effects of exercise and amino acid supplementation on body composition and physical function in community-dwelling elderly Japanese sarcopenic women: a randomized controlled trial. J Am Geriatr Soc 60:16–23
Slade SC, Dionne CE, Underwood M et al (2016) Consensus on exercise reporting template (CERT): explanation and elaboration statement. Br J Sports Med 50:1428–37
Petermann-Rocha F, Balntzi V, Gray SR et al (2022) Global prevalence of sarcopenia and severe sarcopenia: a systematic review and meta-analysis. J Cachexia Sarcopenia Muscle 13:86–99
Lu L, Mao L, Feng Y et al (2021) Effects of different exercise training modes on muscle strength and physical performance in older people with sarcopenia: a systematic review and meta-analysis. BMC Geriatr 21:1–30
Wu P-Y, Huang K-S, Chen K-M et al (2021) Exercise, nutrition, and combined exercise and nutrition in older adults with sarcopenia: a systematic review and network meta-analysis. Maturitas 145:38–48
Escriche-Escuder A, Fuentes-Abolafio IJ, Roldan-Jimenez C et al (2021) Effects of exercise on muscle mass, strength, and physical performance in older adults with sarcopenia: a systematic review and meta-analysis according to the EWGSOP criteria. Exp Gerontol 151:111420
Chen N, He X, Feng Y et al (2021) Effects of resistance training in healthy older people with sarcopenia: a systematic review and meta-analysis of randomized controlled trials. Eur Rev Aging Phys Act 18:1–19
Barajas-Galindo DE, Arnáiz EG, Vicente PF et al (2021) Effects of physical exercise in sarcopenia. A systematic review. Endocrinol Diabetes Nutr Engl Ed 68:159–69
Bray NW, Smart RR, Jakobi JM et al (2016) Exercise prescription to reverse frailty. Appl Physiol Nutr Metab 41:1112–6
Hammerich AS, Anemaet WK (2016) Applying the evidence for exercise prescription in older adults with knee osteoarthritis. Curr Geriatr Rep 5:179–90
Mazzeo RS, Tanaka H (2001) Exercise prescription for the elderly. Sports Med 31:809–18
Booth ML, Bauman A, Owen N et al (1997) Physical activity preferences, preferred sources of assistance, and perceived barriers to increased activity among physically inactive Australians. Prev Med 26:131–7
Lee PG, Jackson EA, Richardson CR (2017) Exercise prescriptions in older adults. Am Fam Physician 95:425–32
Mora JC, Valencia WM (2018) Exercise and older adults. Clin Geriatr Med 34:145–62
Funding
Open access funding provided by Manipal Academy of Higher Education, Manipal.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical approval
Not Applicable.
Informed consent
Not Applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: The citations in Tables 1, 2, 3 and 4 were partially incorrect.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kumar, P., Umakanth, S. & Girish, N. A review of the components of exercise prescription for sarcopenic older adults. Eur Geriatr Med 13, 1245–1280 (2022). https://doi.org/10.1007/s41999-022-00693-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41999-022-00693-7