Abstract
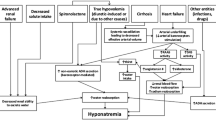
Electrolyte and acid–base disturbances are frequent in patients with end-stage liver disease; the underlying physiopathological mechanisms are often complex and represent a diagnostic and therapeutic challenge to the physician. Usually, these disorders do not develop in compensated cirrhotic patients, but with the onset of the classic complications of cirrhosis such as ascites, renal failure, spontaneous bacterial peritonitis and variceal bleeding, multiple electrolyte, and acid–base disturbances emerge. Hyponatremia parallels ascites formation and is a well-known trigger of hepatic encephalopathy; its management in this particular population poses a risky challenge due to the high susceptibility of cirrhotic patients to osmotic demyelination. Hypokalemia is common in the setting of cirrhosis: multiple potassium wasting mechanisms both inherent to the disease and resulting from its management make these patients particularly susceptible to potassium depletion even in the setting of normokalemia. Acid–base disturbances range from classical respiratory alkalosis to high anion gap metabolic acidosis, almost comprising the full acid–base spectrum. Because most electrolyte and acid–base disturbances are managed in terms of their underlying trigger factors, a systematic physiopathological approach to their diagnosis and treatment is required.


Similar content being viewed by others
Abbreviations
- AG:
-
Anion gap
- AKI:
-
Acute kidney injury
- AQ2:
-
Aquaporin 2
- AVP:
-
Arginine vasopressin
- BP:
-
Blood pressure
- CNI:
-
Calcineurin inhibitors
- CNS:
-
Central nervous system
- DRTA:
-
Distal renal tubular acidosis
- EG:
-
Ethylene glycol
- ENAC:
-
Epithelial sodium channels
- ESLD:
-
End-stage liver disease
- FFP:
-
Fresh frozen plasma
- GFR:
-
Glomerular filtration rate
- HE:
-
Hepatic encephalopathy
- HRS:
-
Hepatorenal syndrome
- NG:
-
Nasogastric
- NH4+ :
-
Ammonium
- NH3:
-
Ammonia
- MELD:
-
Model for End-Stage Liver Disease
- OLT:
-
Orthotopic liver transplantation
- OSD:
-
Osmotic demyelination syndrome
- PBC:
-
Primary biliary cirrhosis
- RAAS:
-
Renin–angiotensin–aldosterone system
- ROMK:
-
Renal outer medullary potassium channels
- RTA:
-
Renal tubular acidosis
- SBP:
-
Spontaneous bacterial peritonitis
- SIAD:
-
Syndrome of inappropriate antidiuresis
- TAL:
-
Thick ascending limb
- TBW:
-
Total body water
- UAG:
-
Urinary anion gap
- VR2:
-
Vasopressin receptor 2
References
Funk GC, Doberer D, Kneidinger N, Lindner G, Holzinger U, Schneeweiss B. Acid-base disturbances in critically ill patients with cirrhosis. Liver Int. 2007;27:901–909.
Ahya SN, José Soler M, Levitsky J, Batlle D. Acid-base and potassium disorders in liver disease. Semin Nephrol. 2006;26:466–470.
Henriksen JH, Bendtsen F, Møller S. Acid-base disturbance in patients with cirrhosis: relation to hemodynamic dysfunction. Eur J Gastroenterol Hepatol. 2015;27:920–927.
Kim WR, Biggins SW, Kremers WK, et al. Hyponatremia and mortality among patients on the liver-transplant waiting list. N Engl J Med. 2008;359:1018–1026.
Gaduputi V, Chandrala C, Abbas N, Tariq H, Chilimuri S, Balar B. Prognostic significance of hypokalemia in hepatic encephalopathy. Hepatogastroenterology. 2014;61:1170–1174.
Funk GC, Doberer D, Osterreicher C, Peck-Radosavljevic M, Schmid M, Schneeweiss B. Equilibrium of acidifying and alkalinizing metabolic acid-base disorders in cirrhosis. Liver Int. 2005;25:505–512.
Guevara M, Baccaro ME, Torre A, et al. Hyponatremia is a risk factor of hepatic encephalopathy in patients with cirrhosis: a prospective study with time-dependent analysis. Am J Gastroenterol. 2009;104:1382–1389.
Shafiei MS, Lui S, Rockey DC. Integrin-linked kinase regulates endothelial cell nitric oxide synthase expression in hepatic sinusoidal endothelial cells. Liver Int. 2015;35:1213–1221.
Abraldes JG, Iwakiri Y, Loureiro-Silva M, Haq O, Sessa WC, Groszmann RJ. Mild increases in portal pressure upregulate vascular endothelial growth factor and endothelial nitric oxide synthase in the intestinal microcirculatory bed, leading to a hyperdynamic state. Am J Physiol Gastrointest Liver Physiol. 2006;290:G980–G987.
Martin PY, Ginès P, Schrier RW. Nitric oxide as a mediator of hemodynamic abnormalities and sodium and water retention in cirrhosis. N Engl J Med. 1998;339:533–541.
Kayali Z, Herring J, Baron P, et al. Increased plasma nitric oxide, l-arginine, and arginase-1 in cirrhotic patients with progressive renal dysfunction. J Gastroenterol Hepatol. 2009;24:1030–1037.
Schrier RW, Arroyo V, Bernardi M, Epstein M, Henriksen JH, Rodés J. Peripheral arterial vasodilation hypothesis: a proposal for the initiation of renal sodium and water retention in cirrhosis. Hepatology. 1988;8:1151–1157.
Bengus A, Babiuc RD. Hyponatremia–predictor of adverse prognosis in cirrhosis. J Med Life. 2012;5:176–178.
Liamis G, Filippatos TD, Liontos A, Elisaf MS. Hyponatremia in patients with liver diseases: not just a cirrhosis-induced hemodynamic compromise. Hepatol Int. 2016;10:762–772.
Fortgens P, Pillay TS. Pseudohyponatremia revisited: a modern-day pitfall. Arch Pathol Lab Med. 2011;135:516–519.
Vo H, Gosmanov AR, Garcia-Rosell M, Wall BM. Pseudohyponatremia in acute liver disease. Am J Med Sci. 2013;345:62–64.
Massonnet B, Delwail A, Ayrault J-M, Chagneau-Derrode C, Lecron J-C, Silvain C. Increased immunoglobulin A in alcoholic liver cirrhosis: exploring the response of B cells to Toll-like receptor 9 activation. Clin Exp Immunol. 2009;158:115–124.
Hoorn EJ, Zietse R. Diagnosis and treatment of hyponatremia: compilation of the guidelines. J Am Soc Nephrol 2017. doi:10.1681/ASN.2016101139. [Epub ahead of print] PubMed PMID: 28174217.
Spasovski G, Vanholder R, Allolio B, et al. Clinical practice guideline on diagnosis and treatment of hyponatraemia. Nephrol Dial Transplant. 2014;29:i1–i39.
Xiao HY, Wang YX, Xu TD, et al. Evaluation and treatment of altered mental status patients in the emergency department: Life in the fast lane. World J Emerg Med. 2012;3:270–277.
Filippatos TD, Liamis G, Elisaf MS. Ten pitfalls in the proper management of patients with hyponatremia. Postgrad Med. 2016;128:516–522.
Liamis G, Milionis H, Elisaf M. A review of drug-induced hyponatremia. Am J Kidney Dis. 2008;52:144–153.
Liamis G, Milionis HJ, Elisaf M. Hyponatremia in patients with infectious diseases. J Infect. 2011;63:327–335.
Angeli P, Wong F, Watson H, Ginès P. CAPPS investigators: hyponatremia in cirrhosis: results of a patient population survey. Hepatology. 2006;44:1535–1542.
Subramanya AR, Ellison DH. Distal convoluted tubule. Clin J Am Soc Nephrol. 2014;9:2147–2163.
Danziger J, Zeidel ML. Osmotic homeostasis. Clin J Am Soc Nephrol. 2015;10:852–862.
Adrogué HJ, Madias NE. The challenge of hyponatremia. J Am Soc Nephrol. 2012;23:1140–1148.
Häussinger D. Low grade cerebral edema and the pathogenesis of hepatic encephalopathy in cirrhosis. Hepatology. 2006;43:1187–1190.
Restuccia T, Gómez-Ansón B, Guevara M, et al. Effects of dilutional hyponatremia on brain organic osmolytes and water content in patients with cirrhosis. Hepatology. 2004;39:1613–1622.
Sterns RH. Disorders of plasma sodium–causes, consequences, and correction. N Engl J Med. 2015;372:55–65.
Córdoba J, Garcia-Martinez R, Simón-Talero M. Hyponatremic and hepatic encephalopathies: similarities, differences and coexistence. Metab Brain Dis. 2010;25:73–80.
Solà E, Watson H, Graupera I, et al. Factors related to quality of life in patients with cirrhosis and ascites: relevance of serum sodium concentration and leg edema. J Hepatol. 2012;57:1199–1206.
Sinha VK, Ko B. Hyponatremia in cirrhosis-pathogenesis, treatment, and prognostic significance. Adv Chronic Kidney Dis. 2015;22:361–367.
Schwabl P, Bucsics T, Soucek K, et al. Risk factors for development of spontaneous bacterial peritonitis and subsequent mortality in cirrhotic patients with ascites. Liver Int. 2015;35:2121–2128.
Cárdenas A, Solà E, Rodríguez E, et al. Hyponatremia influences the outcome of patients with acute-on-chronic liver failure: an analysis of the CANONIC study. Crit Care. 2014;18:700.
Møller S, Krag A, Bendtsen F. Kidney injury in cirrhosis: pathophysiological and therapeutic aspects of hepatorenal syndromes. Liver Int. 2014;34:1153–1163.
Cárdenas A, Riggio O. Correction of hyponatraemia in cirrhosis: treating more than a number! J Hepatol. 2015;62:13–14.
Ahluwalia V, Heuman DM, Feldman G, et al. Correction of hyponatraemia improves cognition, quality of life, and brain oedema in cirrhosis. J Hepatol. 2015;62:75–82.
Yun BC, Kim WR. Hyponatremia in hepatic encephalopathy: an accomplice or innocent bystander? Am J Gastroenterol. 2009;104:1390–1391.
Watson H, Jepsen P, Wong F, Ginès P, Córdoba J, Vilstrup H. Satavaptan treatment for ascites in patients with cirrhosis: a meta-analysis of effect on hepatic encephalopathy development. Metab Brain Dis. 2013;28:301–305.
Sterns RH, Nigwekar SU, Hix JK. The treatment of hyponatremia. Semin Nephrol. 2009;29:282–299.
King JD, Rosner MH. Osmotic demyelination syndrome. Am J Med Sci. 2010;339:561–567.
Gerbes AL, Gülberg V, Ginès P, et al. Therapy of hyponatremia in cirrhosis with a vasopressin receptor antagonist: a randomized double-blind multicenter trial. Gastroenterology. 2003;124:933–939.
Ginès P, Wong F, Watson H, et al. Clinical trial: short-term effects of combination of satavaptan, a selective vasopressin V2 receptor antagonist, and diuretics on ascites in patients with cirrhosis without hyponatraemia–a randomized, double-blind, placebo-controlled study. Aliment Pharmacol Ther. 2010;31:834–845.
Ginès P, Wong F, Watson H, Milutinovic S, del Arbol LR, Olteanu D. Effects of satavaptan, a selective vasopressin V(2) receptor antagonist, on ascites and serum sodium in cirrhosis with hyponatremia: a randomized trial. Hepatology. 2008;48:204–213.
McCormick PA, Mistry P, Kaye G, Burroughs AK, McIntyre N. Intravenous albumin infusion is an effective therapy for hyponatraemia in cirrhotic patients with ascites. Gut. 1990;31:204–207.
Garcia-Martinez R, Caraceni P, Bernardi M, Ginès P, Arroyo V, Jalan R. Albumin: pathophysiologic basis of its role in the treatment of cirrhosis and its complications. Hepatology. 2013;58:1836–1846.
Soupart A, Coffernils M, Couturier B, Gankam-Kengne F, Decaux G. Efficacy and tolerance of urea compared with vaptans for long-term treatment of patients with SIADH. Clin J Am Soc Nephrol. 2012;7:742–747.
Miller PD, Linas SL, Schrier RW. Plasma demeclocycline levels and nephrotoxicity. Correlation in hyponatremic cirrhotic patients. JAMA. 1980;243:2513–2515.
John S, Thuluvath PJ. Hyponatremia in cirrhosis: pathophysiology and management. World J Gastroenterol.. 2015;21:3197–3205.
Schrier RW, Gross P, Gheorghiade M, et al. Tolvaptan, a selective oral vasopressin V2-receptor antagonist, for hyponatremia. N Engl J Med. 2006;355:2099–2112.
Wong F, Blei AT, Blendis LM, Thuluvath PJ. A vasopressin receptor antagonist (VPA-985) improves serum sodium concentration in patients with hyponatremia: a multicenter, randomized, placebo-controlled trial. Hepatology. 2003;37:182–191.
Verbalis JG, Adler S, Schrier RW, Berl T, Zhao Q, Czerwiec FS. Efficacy and safety of oral tolvaptan therapy in patients with the syndrome of inappropriate antidiuretic hormone secretion. Eur J Endocrinol. 2011;164:725–732.
Berl T, Quittnat-Pelletier F, Verbalis JG, et al. Oral tolvaptan is safe and effective in chronic hyponatremia. J Am Soc Nephrol. 2010;21:705–712.
Dahl E, Gluud LL, Kimer N, Krag A. Meta-analysis: the safety and efficacy of vaptans (tolvaptan, satavaptan and lixivaptan) in cirrhosis with ascites or hyponatraemia. Aliment Pharmacol Ther. 2012;36:619–626.
Higashihara E, Torres VE, Chapman AB, et al. Tolvaptan in autosomal dominant polycystic kidney disease: three years’ experience. Clin J Am Soc Nephrol. 2011;6:2499–2507.
FDA: FDA Drug Safety Communication: FDA limits duration and usage of Samsca (tolvaptan) due to possible liver injury leading to organ transplant or death. Available at: http://www.fda.gov/downloads/Drugs/DrugSafety/UCM350084.pdf. Accessed July 20, 2016.
Wong F, Watson H, Gerbes A, et al. Satavaptan for the management of ascites in cirrhosis: efficacy and safety across the spectrum of ascites severity. Gut. 2012;61:108–116.
O’Leary JG, Davis GL. Conivaptan increases serum sodium in hyponatremic patients with end-stage liver disease. Liver Transpl. 2009;15:1325–1329.
Facciorusso A, Amoruso A, Neve V, Antonino M, Prete VD, Barone M. Role of vaptans in the management of hydroelectrolytic imbalance in liver cirrhosis. World J Hepatol. 2014;6:793–799.
Runyon BA. Introduction to the revised American association for the study of liver diseases practice guideline management of adult patients with ascites due to cirrhosis 2012. Hepatology. 2013;57:1651–1653.
European Association for the Study of the Liver. EASL clinical practice guidelines on the management of ascites, spontaneous bacterial peritonitis, and hepatorenal syndrome in cirrhosis. J Hepatol. 2010;53:397–417.
Gianotti RJ, Cárdenas A. Hyponatraemia and cirrhosis. Gastroenterol Rep (Oxf). 2014;2:21–26.
Ginès P, Guevara M. Hyponatremia in cirrhosis: pathogenesis, clinical significance, and management. Hepatology. 2008;48:1002–1010.
Bernardi M, Ricci CS, Santi L. Hyponatremia in patients with cirrhosis of the liver. J Clin Med. 2014;4:85–101.
Moritz ML, Ayus JC. Maintenance intravenous fluids in acutely ill patients. N Engl J Med. 2015;373:1350–1360.
Casey TH, Summerskill WH, Orvis AL. Body and serum potassium in liver disease. I. Relationship to hepatic function and associated factors. Gastroenterology. 1965;48:198–207.
Nagant De Deuxchaines C, Collet RA, Busset R, Mach RS. Exchangeable potassium in wasting, amyotrophy, heart-disease, and cirrhosis of the liver. Lancet. 1961;1:681–687.
Casey TH, Summerskill WH, Bickford RG, Rosevear JW. Body and serum potassium in liver disease. II. Relationships to arterial ammonia, blood pH, and hepatic coma. Gastroenterology. 1965;48:208–215.
Unwin RJ, Luft FC, Shirley DG. Pathophysiology and management of hypokalemia: a clinical perspective. Nat Rev Nephrol. 2011;7:75–84.
Krapf R, Beeler I, Hertner D, Hulter HN. Chronic respiratory alkalosis. The effect of sustained hyperventilation on renal regulation of acid-base equilibrium. N Engl J Med. 1991;324:1394–1401.
Krapf R, Caduff P, Wagdi P, Stäubli M, Hulter HN. Plasma potassium response to acute respiratory alkalosis. Kidney Int. 1995;47:217–224.
Gabduzda GJ, Hall PW. Relation of potassium depletion to renal ammonium metabolism and hepatic coma. Medicine (Baltimore). 1966;45:481–490.
Abu Hossain S, Chaudhry FA, Zahedi K, Siddiqui F, Amlal H. Cellular and molecular basis of increased ammoniagenesis in potassium deprivation. Am J Physiol Renal Physiol. 2011;301:F969–F978.
Palmer BF. Regulation of potassium homeostasis. Clin J Am Soc Nephrol. 2015;10:1050–1060.
Koivisto M, Valta P, Höckerstedt K, Lindgren L. Magnesium depletion in chronic terminal liver cirrhosis. Clin Transplant. 2002;16:325–328.
Elisaf M, Merkouropoulos M, Tsianos EV, Siamopoulos KC. Pathogenetic mechanisms of hypomagnesemia in alcoholic patients. J Trace Elem Med Biol. 1995;9:210–214.
De Marchi S, Cecchin E, Basile A, Bertotti A, Nardini R, Bartoli E. Renal tubular dysfunction in chronic alcohol abuse–effects of abstinence. N Engl J Med. 1993;329:1927–1934.
Martin KJ, González EA, Slatopolsky E. Clinical consequences and management of hypomagnesemia. J Am Soc Nephrol. 2009;20:2291–2295.
Ayuk J, Gittoes NJ. Treatment of hypomagnesemia. Am J Kidney Dis. 2014;63:691–695.
Huang CL, Kuo E. Mechanism of hypokalemia in magnesium deficiency. J Am Soc Nephrol. 2007;18:2649–2652.
Wiese S, Hove JD, Bendtsen F, Møller S. Cirrhotic cardiomyopathy: pathogenesis and clinical relevance. Nat Rev Gastroenterol Hepatol. 2014;11:177–186.
Mozos I. Arrhythmia risk in liver cirrhosis. World J Hepatol. 2015;7:662–672.
Decaux G, Soupart A, Cauchie P, Delwiche F. Potassium homeostasis in liver cirrhosis. Arch Intern Med. 1988;148:547–548.
Maiwall R, Kumar S, Sharma MK, Wani Z, Ozukum M, Sarin SK. Prevalence and prognostic significance of hyperkalemia in hospitalized patients with cirrhosis. J Gastroenterol Hepatol. 2015;31:988–994.
Abbas Z, Mumtaz K, Salam A, Jafri W. Factors predicting hyperkalemia in patients with cirrhosis receiving spironolactone. J Coll Physicians Surg Pak. 2003;13:382–384.
Karagiannis AK, Nakouti T, Pipili C, Cholongitas E. Adrenal insufficiency in patients with decompensated cirrhosis. World J Hepatol. 2015;7:1112–1124.
Bayliss DA, Millhorn DE, Gallman EA, Cidlowski JA. Progesterone stimulates respiration through a central nervous system steroid receptor-mediated mechanism in cat. Proc Natl Acad Sci USA. 1987;84:7788–7792.
Lustik SJ, Chhibber AK, Kolano JW, et al. The hyperventilation of cirrhosis: progesterone and estradiol effects. Hepatology. 1997;25:55–58.
Kaltsakas G, Antoniou E, Palamidas AF, et al. Dyspnea and respiratory muscle strength in end-stage liver disease. World J Hepatol. 2013;5:56–63.
Passino C, Giannoni A, Mannucci F, et al. Abnormal hyperventilation in patients with hepatic cirrhosis: role of enhanced chemosensitivity to carbon dioxide. Int J Cardiol. 2012;154:22–26.
Palmer BF. Evaluation and treatment of respiratory alkalosis. Am J Kidney Dis. 2012;60:834–838.
Soifer JT, Kim HT. Approach to metabolic alkalosis. Emerg Med Clin North Am. 2014;32:453–463.
Luke RG, Galla JH. It is chloride depletion alkalosis, not contraction alkalosis. J Am Soc Nephrol. 2012;23:204–207.
Schrier RW. Use of diuretics in heart failure and cirrhosis. Semin Nephrol. 2011;31:503–512.
Qavi AH, Kamal R, Schrier RW. Clinical Use of Diuretics in Heart Failure, Cirrhosis, and Nephrotic Syndrome. Int J Nephrol. 2015;2015:975934.
Arroyo V, García-Martinez R, Salvatella X. Human serum albumin, systemic inflammation, and cirrhosis. J Hepatol. 2014;61:396–407.
Bruno CM. Acid-base disturbance in liver cirrhosis. Eur J Gastroenterol Hepatol. 2016;28:363.
Berend K, de Vries APJ, Gans ROB. Physiological approach to assessment of acid-base disturbances. N Engl J Med. 2015;372:195.
Bernardi M, Predieri S. Disturbances of acid-base balance in cirrhosis: a neglected issue warranting further insights. Liver Int. 2005;25:463–466.
Kraut JA, Madias NE. Metabolic acidosis: pathophysiology, diagnosis and management. Nat Rev Nephrol. 2010;6:274–285.
Kraut JA, Madias NE. Lactic acidosis. N Engl J Med. 2014;371:2309–2319.
Kraut JA, Madias NE. Lactic acidosis: current treatments and future directions. Am J Kidney Dis. 2016.
Lévy S, Hervé C, Delacoux E, Erlinger S. Thiamine deficiency in hepatitis C virus and alcohol-related liver diseases. Dig Dis Sci. 2002;47:543–548. doi:10.1023/A:1017907817423.
Keating GM. Entecavir: a review of its use in the treatment of chronic hepatitis B in patients with decompensated liver disease. Drugs. 2011;71:2511–2529.
García-Compeán D, González-González JA, Lavalle-González FJ, González-Moreno EI, Maldonado-Garza HJ, Villarreal-Pérez JZ. The treatment of diabetes mellitus of patients with chronic liver disease. Ann Hepatol. 2015;14:780–788.
Paré P, Reynolds TB. Impaired renal acidification in alcoholic liver disease. Arch Intern Med. 1984;144:941–944.
Caregaro L, Lauro S, Ricci G, Gatta A, Zuin R, Ruol A. Pathogenetic relationships between renal tubular acidosis and sodium metabolism alterations in liver cirrhosis. Digestion. 1983;26:179–186.
Subrahmanyam DK, Vadivelan M, Giridharan S, Balamurugan N. Wilson’s disease: a rare cause of renal tubular acidosis with metabolic bone disease. Indian J Nephrol. 2014;24:171–174.
Golding PL, Mason AS. Renal tubular acidosis and autoimmune liver disease. Gut. 1971;12:153–157.
Tsantoulas DC, McFarlane IF, Portmann B, Eddleston AL, Williams R. Proceedings: cell-mediated immunity to human Tamm-Horsfall glycoprotein in autoimmune liver disease associated with renal tubular acidosis. Gut. 1974;15:826.
Komatsuda A, Wakui H, Ohtani H, et al. Tubulointerstitial nephritis and renal tubular acidosis of different types are rare but important complications of primary biliary cirrhosis. Nephrol Dial Transplant. 2010;25:3575–3579.
Unwin RJ, Shirley DG, Capasso G. Urinary acidification and distal renal tubular acidosis. J Nephrol. 2002;15:S142–S150.
Rastogi SP, Crawford C, Wheeler R, Flanigan W, Arruda JA. Effect of furosemide on urinary acidification in distal renal tubular acidosis. J Lab Clin Med. 1984;104:271–282.
Batlle DC, von Riotte A, Schlueter W. Urinary sodium in the evaluation of hyperchloremic metabolic acidosis. N Engl J Med. 1987;316:140–144.
Kamel KS, Ethier JH, Richardson RM, Bear RA, Halperin ML. Urine electrolytes and osmolality: when and how to use them. Am J Nephrol. 1990;10:89–102.
Batlle DC, Hizon M, Cohen E, Gutterman C, Gupta R. The use of the urinary anion gap in the diagnosis of hyperchloremic metabolic acidosis. N Engl J Med. 1988;318:594–599.
Wagner CA. Effect of mineralocorticoids on acid-base balance. Nephron Physiol. 2014;128:26–34.
Gabow PA, Moore S, Schrier RW. Spironolactone-induced hyperchloremic acidosis in cirrhosis. Ann Intern Med. 1979;90:338–340.
Fabrizi F, Messa P. Challenges in renal failure treatment before liver transplant. Clin Liver Dis. 2017;21:303–319.
Heuman DM, Abou-Assi SG, Habib A, et al. Persistent ascites and low serum sodium identify patients with cirrhosis and low MELD scores who are at high risk for early death. Hepatology. 2004;40:802–810.
Ruf AE, Kremers WK, Chavez LL, Descalzi VI, Podesta LG, Villamil FG. Addition of serum sodium into the MELD score predicts waiting list mortality better than MELD alone. Liver Transpl. 2005;11:336–343.
Londoño MC, Cárdenas A, Guevara M, et al. MELD score and serum sodium in the prediction of survival of patients with cirrhosis awaiting liver transplantation. Gut. 2007;56:1283–1290.
Biggins SW, Rodriguez HJ, Bacchetti P, Bass NM, Roberts JP, Terrault NA. Serum sodium predicts mortality in patients listed for liver transplantation. Hepatology. 2005;41:32–39.
OPTN/UNOS Liver and Intestinal Organ Transplantation Committee. Proposal to Add Serum Sodium to the MELD Score. Available at: https://optn.transplant.hrsa.gov/media/1834/liver_boardreport_20140702.pdf Accessed July 28, 2016.
Fisher RA, Heuman DM, Harper AM, et al. Region 11 MELD Na exception prospective study. Ann Hepatol. 2012;11:62–67.
OPTN/UNOS Policy Notice. Clerical changes for implementation of adding serum sodium to the MELD score. Available at: https://optn.transplant.hrsa.gov/media/1575/policynotice_20151101.pdf Accessed July 28, 2016.
Sersté T, Gustot T, Rautou PE, et al. Severe hyponatremia is a better predictor of mortality than MELDNa in patients with cirrhosis and refractory ascites. J Hepatol. 2012;57:274–280.
Cárdenas A, Ginès P. Predicting mortality in cirrhosis–serum sodium helps. N Engl J Med. 2008;359:1060–1062.
Biggins SW. Use of serum sodium for liver transplant graft allocation: a decade in the making, now is it ready for primetime? Liver Transpl. 2015;21:279–281.
Cimen S, Guler S, Ayloo S, Molinari M. Implications of Hyponatremia in Liver Transplantation. J Clin Med. 2015;4:66–74.
Christensen E, Gunson B, Neuberger J. Optimal timing of liver transplantation for patients with primary biliary cirrhosis: use of prognostic modelling. J Hepatol. 1999;30:285–292.
Londoño MC, Guevara M, Rimola A, et al. Hyponatremia impairs early posttransplantation outcome in patients with cirrhosis undergoing liver transplantation. Gastroenterology. 2006;130:1135–1143.
Boin-I-de FSF, Leonardi MI, Udo EY, Sevá-Pereira T, Stucchi RSB, Leonardi LS. The application of MELD score in patients submitted to liver transplantation: a retrospective analysis of survival and the predictive factors in the short and long term. Arq Gastroenterol. 2008;45:275–283.
Dawwas MF, Lewsey JD, Neuberger JM, Gimson AE. The impact of serum sodium concentration on mortality after liver transplantation: a cohort multicenter study. Liver Transpl. 2007;13:1115–1124.
Hackworth WA, Heuman DM, Sanyal AJ, et al. Effect of hyponatraemia on outcomes following orthotopic liver transplantation. Liver Int. 2009;29:1071–1077.
Yun BC, Kim WR, Benson JT, et al. Impact of pretransplant hyponatremia on outcome following liver transplantation. Hepatology. 2009;49:1610–1615.
Leise MD, Yun BC, Larson JJ, et al. Effect of the pretransplant serum sodium concentration on outcomes following liver transplantation. Liver Transpl. 2014;20:687–697.
Karapanagiotou A, Kydona C, Papadopoulos S, et al. The effect of hyponatremia on the outcome of patients after orthotopic liver transplantation. Transplant Proc. 2012;44:2724–2726.
Sharma P, Schaubel DE, Goodrich NP, Merion RM. Serum sodium and survival benefit of liver transplantation. Liver Transpl. 2015;21:308–313.
Lee EM, Kang JK, Yun S-C, et al. Risk factors for central pontine and extrapontine myelinolysis following orthotopic liver transplantation. Eur Neurol. 2009;62:362–368.
Morard I, Gasche Y, Kneteman M, et al. Identifying risk factors for central pontine and extrapontine myelinolysis after liver transplantation: a case-control study. Neurocrit Care. 2014;20:287–295.
Totsuka E, Dodson F, Urakami A, et al. Influence of high donor serum sodium levels on early postoperative graft function in human liver transplantation: effect of correction of donor hypernatremia. Liver Transpl Surg. 1999;5:421–428.
Cywinski JB, Mascha E, Miller C, et al. Association between donor-recipient serum sodium differences and orthotopic liver transplant graft function. Liver Transpl. 2008;14:59–65.
Mangus RS, Fridell JA, Vianna RM, et al. Severe hypernatremia in deceased liver donors does not impact early transplant outcome. Transplantation. 2010;90:438–443.
Dawwas MF, Lewsey JD, Watson CJ, Gimson AE. The impact of serum potassium concentration on mortality after liver transplantation: a cohort multicenter study. Transplantation. 2009;88:402–410.
Ayres EJ, Lee BR, Weckwerth JA, Myhre LJ, Freese D, Lobritto S. Potassium supplementation requirement post orthotopic liver transplantation in children. J Liver: Dis Transplant. 2013;2:2.
Xia VW, Du B, Tran A, et al. Intraoperative hypokalemia in pediatric liver transplantation: incidence and risk factors. Anesth Analg. 2006;103:587–593.
Nakasuji M, Bookallil MJ. Pathophysiological mechanisms of postrevascularization hyperkalemia in orthotopic liver transplantation. Anesth Analg. 2000;91:1351–1355.
Merritt WT. Metabolism and liver transplantation: review of perioperative issues. Liver Transpl. 2000;6:S76–S84.
Shangraw RE. Metabolic issues in liver transplantation. Int Anesthesiol Clin. 2006;44:1–20.
Shangraw RE, Hexem JG. Glucose and potassium metabolic responses to insulin during liver transplantation. Liver Transpl Surg. 1996;2:443–454.
Li Q, Zhou M-T, Wang Y, et al. Effect of insulin on hyperkalemia during anhepatic stage of liver transplantation. World J Gastroenterol. 2004;10:2427–2429.
Nadim MK, Annanthapanyasut W, Matsuoka L, et al. Intraoperative hemodialysis during liver transplantation: a decade of experience. Liver Transpl. 2014;20:756–764.
Raj D, Abreo K, Zibari G. Metabolic alkalosis after orthotopic liver transplantation. Am J Transpl. 2003;3:1566–1569.
Contreras G, Garces G, Reich J, et al. Predictors of alkalosis after liver transplantation. Am J Kidney Dis. 2002;40:517–524.
Boniatti MM, Filho EMR, Cardoso PRC, Vieira SRR. Physicochemical evaluation of acid-base disorders after liver transplantation and the contribution from administered fluids. Transplant Proc. 2013;45:2283–2287.
Guidet B, Soni N, Rocca Della G, et al. A balanced view of balanced solutions. Crit Care. 2010;14:325.
Bobadilla NA, Gamba G. New insights into the pathophysiology of cyclosporine nephrotoxicity: a role of aldosterone. Am J Physiol Renal Physiol. 2007;293:F2–F9.
Lee CH, Kim GH. Electrolyte and Acid-base disturbances induced by clacineurin inhibitors. Electrolyte Blood Press. 2007;5:126–130.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Jiménez, J.V., Carrillo-Pérez, D.L., Rosado-Canto, R. et al. Electrolyte and Acid–Base Disturbances in End-Stage Liver Disease: A Physiopathological Approach. Dig Dis Sci 62, 1855–1871 (2017). https://doi.org/10.1007/s10620-017-4597-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-017-4597-8