Abstract
Background
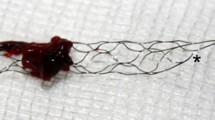
Endovascular treatment (EVT) is an established procedure in patients with acute ischemic stroke due to occlusion of the proximal M1-segment of middle cerebral artery. The assessment of distal thrombectomy in daily clinical routine has not yet been sufficiently evaluated.
Methods
Patients with M2-segment-occlusions treated by EVT in the local department (January 2012–December 2017) were included (n = 57, mean National-Institutes-of-Health-Stroke-Scale of 11, range 0–20). Patients were grouped according to localization of M2-occlusion (Cohort A (n = 14): central region only, B (n = 24): central region and involvement of frontal vessels, C (n = 19): parietal, occipital, and/or temporal vessels). Differences in proximal (M2-trunk, n = 34) and distal (M2-branches, n = 23) occlusions were also examined. Reperfusion (Thrombolysis-In-Cerebral-Infarction (TICI)), early clinical outcome at discharge (modified Rankin Scale (mRS)), and complications (hemorrhage, new emboli) were noted.
Result
Successful reperfusion (TICI2b–3) was found in 49 patients (86.0%). Favorable early clinical outcome (mRS0–2) was achieved in n = 19 (37.7%). Compared to admission, mRS at discharge improved significantly (median (admission) 5 vs. median (discharge) 4, p < 0.001). Early clinical outcome was more favorable in patients with better reperfusion (TICI2b-3: mean mRS 3 ± 1.7 vs. TICI0–2a: mean mRS 4.4 ± 1.4, p = 0.037). Six (10.5%) patients suffered from symptomatic intracranial hemorrhage during treatment or hospitalization. Four patients died (7.0%). No significant differences in favorable clinical outcome (mRS ≤ 2: Cohort A 42.9%, B 50.0%, C 16.7%, p = 0.4; χ2-test) or periinterventional complications were found with regard to vessel involvement.
Conclusion
EVT in patients with acute M2-occlusion is safe and leads to a significant clinical improvement at discharge. No significant differences in clinical outcome or complications were found with regard to the localization of the M2-occlusion.
Similar content being viewed by others
References
Berkhemer OA, Fransen PSS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ et al (2015) A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med 372:11–20 [cited 2018 Sep 25]. Available from: https://www.nejm.org/doi/pdf/10.1056/NEJMoa1411587
Campbell BCV, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N et al (2015) Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med 372:1009–1018 [cited 2018 Sep 29]. Available from: https://www.nejm.org/doi/pdf/10.1056/NEJMoa1414792
Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J et al (2015) Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med 372:1019–1030 [cited 2018 Sep 23]. Available from: www.aspectsinstroke.com
Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A et al (2015) Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med 372:2296–2306 [cited 2018 Sep 29]. Available from: https://www.nejm.org/doi/pdf/10.1056/NEJMoa1503780
Saver JL, Goyal M, Bonafe A, Diener H-C, Levy EI, Pereira VM et al (2015) Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med 372:2285–2295 [cited 2018 Sep 29]. Available from: https://www.nejm.org/doi/pdf/10.1056/NEJMoa1415061
Rahme R, Yeatts SD, Abruzzo TA, Jimenez L, Fan L, Tomsick TA et al (2014) Early reperfusion and clinical outcomes in patients with M 2 occlusion: pooled analysis of the PROACT II, IMS, and IMS II studies. J Neurosurg 121:1354–1358. https://doi.org/10.3171/2014.7.JNS131430
Flores A, Tomasello A, Cardona P, De Miquel MA, Gomis M, Bermejo PG et al (2015) Endovascular treatment for M2 occlusions in the era of stentrievers: a descriptive multicenter experience. J Neurointerv Surg 7:234–237 [cited 2018 Sep 25]. Available from: http://jnis.bmj.com/
Dorn F, Lockau H, Stetefeld H, Kabbasch C, Kraus B, Dohmen C et al (2015) Mechanical thrombectomy of M2-occlusion. J Stroke Cerebrovasc Dis 24:1465–1470 [cited 2018 Aug 12]. Available from: https://www.sciencedirect.com/science/article/pii/S1052305715002062
Sheth SA, Yoo B, Saver JL, Starkman S, Ali LK, Kim D et al (2015) M2 occlusions as targets for endovascular therapy: comprehensive analysis of diffusion/perfusion MRI, angiography, and clinical outcomes. J Neurointerv Surg 7:478–483 [cited 2018 Sep 27]. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24821842
Tomsick TA, Carrozzella J, Foster L, Hill MD, Von Kummer R, Goyal M et al (2017) Endovascular therapy of M2 occlusion in IMS III: role of M2 segment definition and location on clinical and revascularization outcomes. Am J Neuroradiol 38:84–89 [cited 2018 Aug 12]. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27765740
Bhogal P, Bücke P, AlMatter M, Ganslandt O, Bäzner H, Henkes H et al (2017) A comparison of mechanical thrombectomy in the M1 and M2 segments of the middle cerebral artery: a review of 585 consecutive patients. Interv Neurol 6:191–198 [cited 2018 Aug 12]. Available from: http://www.ncbi.nlm.nih.gov/pubmed/29118796
Chen CJ, Wang C, Buell TJ, Ding D, Raper DM, Ironside N et al (2017) Endovascular mechanical thrombectomy for acute middle cerebral artery M2 segment occlusion: a systematic review. World Neurosurg:684–691 [cited 2018 Aug 12]. Available from: https://www.sciencedirect.com/science/article/pii/S1878875017314092
Deutsche Gesellschaft für Neurologie. Leitlinien für Diagnostik und Therapie in der Neurologie. Leitlinien für Diagnostik und Ther der Neurol [Internet]. 2012 [cited 2018 Dec 26]. p 1–17. Available from: www.dgn.org
Warwick Pexman JH, Barber PA, Hill MD, Sevick RJ, Demchuk AM, Hudon ME et al (2001) Use of the Alberta Stroke Program Early CT score (ASPECTS) for assessing CT scans in patients with acute stroke. AJNR Am J Neuroradiol Available from: http://www.ajnr.org/content/ajnr/22/8/1534.full.pdf
Wiesmann M, Brockmann M-A, Heringer S, Müller M, Reich A, Nikoubashman O (2017) Active push deployment technique improves stent/vessel-wall interaction in endovascular treatment of acute stroke with stent retrievers. J Neurointerv Surg 9:253–256 [cited 2019 Apr 22]. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26975839
Humphries W, Hoit D, Doss VT, Elijovich L, Frei D, Loy D, Dooley G, Turk AS, Chaudry I, Turner R, Mocco J, Morone P, Fiorella D, Siddiqui A, Mokin M, Arthur AS (2015) Distal aspiration with retrievable stent assisted thrombectomy for the treatment of acute ischemic stroke. J Neurointerv Surg 7:90–94
Iodice F, Brunetti V, Nicolini E, Paolucci M, Di Lorenzo F (2019) Endovascular therapy for acute ischemic stroke: which role for neurologists? Neurol Sci: 1737–9
Derex L, Nighoghossian N (2008) Intracerebral haemorrhage after thrombolysis for acute ischaemic stroke: an update. J Neurol Neurosurg Psychiatry:1093–1099 [cited 2018 Sep 29]. Available from: http://jnnp.bmj.com/
Larrue V, Von Kummer R, Müller A, Bluhmki E (2001) Risk factors for severe hemorrhagic transformation in ischemic stroke patients treated with recombinant tissue plasminogen activator: a secondary analysis of the European-Australasian acute stroke study (ECASS II). Stroke 32:438–441
R Core Team (2018) R: a language and environment for statistical computing [Internet]. Vienna, Austria. Available from: https://www.r-project.org/
Turc G, Bhogal P, Fischer U, Khatri P, Lobotesis K, Mazighi M et al (2019) European Stroke Organisation (ESO) - European Society for Minimally Invasive Neurological Therapy (ESMINT) guidelines on mechanical thrombectomy in acute ischemic stroke. J Neurointerv Surg:1–30 [cited 2020 Feb 13]. Available from: http://jnis.bmj.com/
Ornello R, Carolei A (2019) Primary stroke centers: are they worthy of an upgrade? Intern Emerg Med:333–334
Coutinho JM, Liebeskind DS, Slater LA, Nogueira RG, Baxter BW, Levy EI et al (2016) Mechanical thrombectomy for isolated M2 occlusions: a post hoc analysis of the star, swift, and SWIFT PRIME studies. Am J Neuroradiol:667–672 [cited 2018 Aug 12]. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26564442
Sarraj A, Sangha N, Hussain MS, Wisco D, Vora N, Elijovich L et al (2016) Endovascular therapy for acute ischemic stroke with occlusion of the middle cerebral artery M2 segment. JAMA Neurol 73:1291–1296 [cited 2018 Sep 30]. Available from: http://archneur.jamanetwork.com/article.aspx?doi=10.1001/jamaneurol.2016.2773
Bhogal P, Bücke P, AlMatter M, Ganslandt O, Bäzner H, Henkes H et al (2017) A comparison of mechanical thrombectomy in the M1 and M2 segments of the middle cerebral artery: a review of 585 consecutive patients. Interv Neurol 6:191–198 [cited 2018 Aug 12]. Available from: http://www.ncbi.nlm.nih.gov/pubmed/29118796
Heider DM, Simgen A, Wagenpfeil G, Dietrich P, Yilmaz U, Mühl-Benninghaus R et al (2020) Why we fail: mechanisms and co-factors of unsuccessful thrombectomy in acute ischemic stroke. Neurol Sci:1–9
Author information
Authors and Affiliations
Contributions
M.K., B.T., and V.I. conceived of the presented idea. V.I. and M.K developed the theory and V.I. performed the computations and analytic calculations. C.R. and J.C verified the analytical methods. M.K. encouraged V.I. to investigate the outcome and vessel involvement in patients with mechanical thrombectomy in acute middle cerebral artery M2 segment occlusions and supervised the findings of this work. V.I., M.K., C.R., J.C., B.T., J.L., M.G., and S.J. contributed to the interpretation of the results. All authors discussed the results and contributed to the final manuscript. V.I. took the lead in writing the manuscript with input and support from all authors (M.K., C.R., J.C., B.T. J.L., M.G., S.J.). All authors provided critical feedback and helped shape the research, analysis and manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in the studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the local ethics committee.
Informed consent
The requirement for written informed consent was waived by the local ethics committee.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ivan, V.L., Rubbert, C., Caspers, J. et al. Mechanical thrombectomy in acute middle cerebral artery M2 segment occlusion with regard to vessel involvement. Neurol Sci 41, 3165–3173 (2020). https://doi.org/10.1007/s10072-020-04430-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-020-04430-5