Abstract
Background
Laparoscopic Heller myotomy is the standard operation for achalasia. The incidence of esophageal perforation is approximately 5% to 10%. Data about the safety and utility of robotically assisted Heller myotomy (RAHM) are scarce. The aim of this study was to assess the efficacy and safety of RAHM for the treatment of esophageal achalasia.
Methods
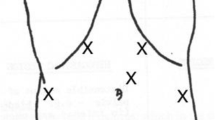
From a prospectively maintained database, demographic data, symptoms, esophagograms, manometries, and perioperative data from all the RAHMs performed between September 2002 and February 2004 were analyzed.
Results
A total of 54 patients underwent RAHM, including 26 men. The mean age of these patients was 43 years (range, 14–75 years). Dysphagia was present in 100% of the patients. Of the 54 patients, 26 (48%) had undergone previous treatment including pneumatic dilation (17 patients), Botox injections (4 patients), or both of these treatments (5 patients). The dissection was performed laparoscopically, and the myotomy was performed with robotic assistance. The operative time, including the robot setup time, averaged 162 min (range, 62–210 min). Blood loss averaged 24 ml. No mucosal perforations were observed. The hospital length of stay was 1.5 days. There were no deaths. At 17 months, 93% of the patients had relief of their dysphagia.
Conclusions
The findings showed RAHM to be safe and effective, with a 0% incidence of perforation and relief of symptoms for 91% of the patients.





Similar content being viewed by others
References
Bloomston M, Serafini F, Boyce HW, Rosemurgy AS (2002) The “learning curve” in videoscopic Heller myotomy. J Laparoendosc Surg 6: 41–47
Bloomston M, Serafini F, Rosemurgy AS (2001) Videoscopic Heller myotomy as first-line therapy for severe achalasia. Am Surg 67: 1105–1109
Bonavina L, Rosati R, Segalin A, Peracchia A (1995) Laparoscopic Heller–Dor operation for the treatment of oesophageal achalasia: technique and early results. Ann Chir Gynaecol 84: 165–168
Chaer RA, Jacobsen G, Elli F, Harris J, Goldstein A, Horgan S (2004) Robotic-assisted laparoscopic pediatric Heller’s cardiomyotomy. J Laparoendosc Adv Surg Tech A 14: 270–273
Csendes A, Braghetto I, Henriquez A, Cortes C (1989) Late results of a prospective randomised study comparing forceful dilatation and oesophagomyotomy in patients with achalasia. Gut 30: 299–304
Donahue PE, Horgan S, Liu KJ, Madura JA (2002) Floppy Dor fundoplication after esophagocardiomyotomy for achalasia. Surgery 132: 716–722, discussion 722–723
Donahue PE, Teresi M, Patel S, Schlesinger PK (1999) Laparoscopic myotomy in achalasia: intraoperative evidence for myotomy of the gastric cardia. Dis Esophagus 12: 30–36
Finley RJ, Clifton JC, Stewart KC, Graham AJ, Worsley DF (2001) Laparoscopic Heller myotomy improves esophageal emptying and the symptoms of achalasia. Arch Surg 136: 892–896
Goldblum JR, Whyte RI, Orringer MB, Appelman HD (1994) Achalasia: a morphologic study of 42 resected specimens. Am J Surg Pathol 18: 327–337
Heller E (1913) Extramucöse Cardioplastie beim chronischen Cardiospasmus mit Dilatation des Oesophagus. Mitt Grengeb Med Chir 2: 141–149
Horgan S, Hudda K, Eubanks T, McAllister J, Pellegrini CA (1999) Does botulinum toxin injection make esophagomyotomy a more difficult operation? Surg Endosc 13: 576–579
Oelschlager BK, Chang L, Pellegrini CA (2003) Improved outcome after extended gastric myotomy for achalasia. Arch Surg 138: 490–495, discussion 495–497
Patti MG, Feo CV, Arcerito M, De Pinto M, Tamburini A, Diener U, Gantert W, Way LW (1999) Effects of previous treatment on results of laparoscopic Heller myotomy for achalasia. Dig Dis Sci 44: 2270–2276
Patti MG, Fisichella PM, Perretta S, Galvani C, Gorodner MV, Robinson T, Way LW (2003) Impact of minimally invasive surgery on the treatment of esophageal achalasia: a decade of change. J Am Coll Surg 196: 698–703, discussion 703–705
Patti MG, Pellegrini CA, Horgan S, Arcerito M, Omelanczuk P, Tamburini A, Diener U, Eubanks TR, Way LW (1999) Minimally invasive surgery for achalasia: an 8-year experience with 168 patients. Ann Surg 230: 587–593, discussion 593–594
Pellegrini CA, Wetter LA, Patti M, Leichter R, Mussan G, Mori T, Bernstein G, Way L (1992) Initial experience with a new approach for the treatment of achalasia. Ann. Surg 216: 291–296
Rakita S, Bloomston M, Villadolid D, Thometz D, Zervos E, Rosemurgy A (2005) Esophagotomy during laparoscopic Heller myotomy cannot be predicted by preoperative therapies and does not influence long-term outcome. J Gastrointest Surg 9: 159–164
Richards WO, Torquati A, Holzman MD, Khaitan L, Byrne D, Lutfi R, Sharp KW (2004) Heller myotomy versus Heller myotomy with Dor fundoplication for achalasia: a prospective randomized double-blind clinical trial. Ann Surg 240: 405–412, discussion 412–415
Sharp KW, Khaitan L, Scholz S, Holzman MD, Richards WO (2002) 100 consecutive minimally invasive Heller myotomies: lessons learned. Ann Surg 235: 631–638, discussion 638–639
Shimi S, Nathanson LK, Cuschieri A (1991) Laparoscopic cardiomyotomy for achalasia. J R Coll Surg Edinb 36: 152–154
Spiess AE, Kahrilas PJ (1998) Treating achalasia: from whalebone to laparoscope. JAMA 280: 638–642
Vaezi MF, Richter JE (1998) Current therapies for achalasia: comparison and efficacy. J Clin Gastroenterol 21–35
West RL, Hirsch DP, Bartelsman JF, de Borst J, Ferwerda G, Tytgat GN, Boeckxstaens GE (2002) Long-term results of pneumatic dilation in achalasia followed for more than 5 years. Am J Gastroenterol 97: 1346–1351
Willis T (1672) Pharmaceutice Rationalis: Sive Diatriba de Medicamentorum: Operationibus in Humano Corpore. Hagae-Comitis, London
Zaninotto G, Costantini M, Molena D, Buin F, Carta A, Nicoletti L, Ancona E (2000) Treatment of esophageal achalasia with laparoscopic Heller myotomy and Dor partial anterior fundoplication: prospective evaluation of 100 consecutive patients. J Gastrointest Surg 4: 282–289
Zaninotto G, Costantini M, Molena D, Portale G, Costantino M, Nicoletti L, Ancona E (2001) Minimally invasive surgery for esophageal achalasia. J Laparoendosc Adv Surg Tech 11: 351–359
Acknowledgment
This study was supported in part by a grant provided by Intuitive Surgical Company.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Galvani, C., Gorodner, M.V., Moser, F. et al. Laparoscopic Heller myotomy for achalasia facilitated by robotic assistance. Surg Endosc 20, 1105–1112 (2006). https://doi.org/10.1007/s00464-005-0272-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-005-0272-9