Abstract
Purpose
To evaluate changes in hospital length-of-stay and time-to-operation of older hip fracture patients before and after the foundation of a co-managed Geriatric Fracture Center (GFC).
Methods
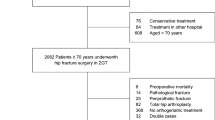
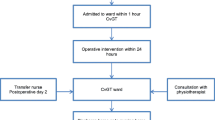
A co-managed GFC was established in a German level-1 trauma center. In a retrospective cohort study, we analyzed femoral neck fracture patients >60 years treated with hemiarthroplasty. Patients treated within the first year after foundation of the GFC were compared to the patients treated during the year before. One-way ANOVA was performed to identify differences regarding time-to-operation and hospital length-of-stay.
Results
One hundred and fourteen patients of the GFC were compared to 169 patients previously treated without co-management. Mean patient age did not significantly differ (81.9 vs. 81.5 years; p = 0.7), nor did gender distribution. Hospital length-of-stay was significantly shorter after foundation of the GFC (13.9 vs. 16.8 days; p = 0.007). The same is true for the interval between hospital admission and operation, which decreased from 3.1 to 2.1 days (p = 0.029). Early surgical complication rate was not significantly affected by GFC foundation (7.7 % pre-GFC vs. 9.6 % GFC; p = 0.6), nor was inpatient mortality (5.9 % pre-GFC vs. 4.4 % GFC; p = 0.6). Subgroup analysis revealed that GFC patients without early surgical complications displayed a reduced length-of-stay (LOS), whereas LOS was even prolonged in GFC patients with surgical complications.
Conclusions
A co-managed GFC offering an organized fracture program for the elderly can reduce hospital length-of-stay and time-to-operation in hip fracture patients. A significant effect can be observed within the first year after establishment of a GFC.

Similar content being viewed by others
References
Bhaskar D, Parker MJ (2011) Haematological indices as surrogate markers of factors affecting mortality after hip fracture. Injury 42:178–182
Buecking B, Timmesfeld N, Riem S, Bliemel C, Hartwig E, Friess T, Liener U, Ruchholtz S, Eschbach D (2013) Early orthogeriatric treatment of trauma in the elderly—a systematic review and metaanalysis. Dtsch Arztebl Int 110:255–262
Dy CJ, Dossous PM, Ton QV, Hollenberg JP, Lorich DG, Lane JM (2011) Does a multidisciplinary team decrease complications in male patients with hip fractures? Clin Orthop Relat Res 469:1919–1924
Dy CJ, Dossous PM, Ton QV, Hollenberg JP, Lorich DG, Lane JM (2012) The medical orthopaedic trauma service: an innovative multidisciplinary team model that decreases in-hospital complications in patients with hip fractures. J Orthop Trauma 26:379–383
Folbert E, Smit R, van der Velde D, Regtuijt M, Klaren H, Hegeman JH (2011) Multidisciplinary integrated care pathway for elderly patients with hip fractures: implementation results from Centre for Geriatric Traumatology, Almelo, The Netherlands. Ned Tijdschr Geneeskd 155:A3197
Fox MT, Persaud M, Maimets I, O‘Brien K, Brooks D, Tregunno D, Schraa E (2012) Effectiveness of acute geriatric unit care using acute care for elders components: a systematic review and meta-analysis. J Am Geriatr Soc 60:2237–2245
Friedman SM, Mendelson DA, Bingham KW, Kates SL (2009) Impact of a comanaged Geriatric Fracture Center on short-term hip fracture outcomes. Arch Intern Med 169:m1712–m1717
González-Montalvo JI, Alarcón T, Mauleón JL, Gil-Garay E, Gotor P, Martín-Vega A (2010) The orthogeriatric unit for acute patients: a new model of care that improves efficiency in the management of patients with hip fracture. Hip Int 20:229–235
Gregersen M, Mørch MM, Hougaard K, Damsgaard EM (2012) Geriatric intervention in elderly patients with hip fracture in an orthopedic ward. J Inj Violence Res 4:45–51
Kammerlander C, Gosch M, Blauth M, Lechleitner M, Luger TJ, Roth T (2011) The tyrolean geriatric fracture center: an orthogeriatric co-management model. Z Gerontol Geriatr 44:363–367
Kammerlander C, Roth T, Friedman SM, Suhm N, Luger TJ, Kammerlander-Knauer U, Krappinger D, Blauth M (2010) Ortho-geriatric service—a literature review comparing different models. Osteoporos Int 21(Suppl 4):S637–S646
Kates SL, Blake D, Bingham KW, Kates OS, Mendelson DA, Friedman SM (2010) Comparison of an organized geriatric fracture program to United States government data. GOS 1(1):15–21
Kates SL, Mendelson DA, Friedman SM (2010) Co-managed care for fragility hip fractures (Rochester model). Osteoporos Int 21(Suppl 4):S621–S625
Kates SL, Mendelson DA, Friedman SM (2011) The value of an organized fracture program for the elderly: early results. J Orthop Trauma 25:233–237
Khan SK, Kalra S, Khanna A, Thiruvengada MM, Parker MJ (2009) Timing of surgery for hip fractures: a systematic review of 52 published studies involving 291.413 patients. Injury 40:692–697
Khasraghi FA, Christmas C, Lee EJ, Mears SC, Wenz JF Sr (2005) Effectiveness of a multidisciplinary team approach to hip fracture management. J Surg Orthop Adv 14:27–31
Liem IS, Kammerlander C, Suhm N, Kates SL, Blauth M (2012) Literature review of outcome parameters used in studies of geriatric fracture centers. Arch Orthop Trauma Surg. doi:10.1007/s00402-012-1594-4
Shiga T, Wajima Z, Ohe Y (2008) Is operative delay associated with increased mortality of hip fracture patients? Systematic review, meta-analysis, and meta-regression. Can J Anaesth 55:146–154
Singler K, Biber R, Wicklein S, Heppner HJ, Sieber CC, Bail HJ (2011) ‘‘N-active’’: a new comanaged, orthogeriatric ward: observations and prospects. Z Gerontol Geriatr 44:368–374
Vochteloo AJ, Borger van der Burg BL, Mertens B, Niggebrugge AH, de Vries MR, Tuinebreijer WE, Bloem RM, Nelissen RG, Pilot P (2011) Outcome in hip fracture patients related to anemia at admission and allogeneic blood transfusion: an analysis of 1262 surgically treated patients. BMC Musculoskelet Disord 12:262
Acknowledgments
We would like to thank our study nurse Mrs. Marion Wendlik for taking care of the databases.
Conflict of interest
RB and HJB received grants from B. Braun Aesculap (Tuttlingen, Germany) within the past 5 years for consulting activities. The other authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Biber, R., Singler, K., Curschmann-Horter, M. et al. Implementation of a co-managed Geriatric Fracture Center reduces hospital stay and time-to-operation in elderly femoral neck fracture patients. Arch Orthop Trauma Surg 133, 1527–1531 (2013). https://doi.org/10.1007/s00402-013-1845-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-013-1845-z