Abstract
Purpose
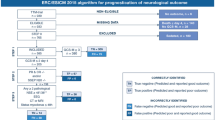
Post-resuscitation guidelines recommend a multimodal algorithm for outcome prediction after cardiac arrest (CA). We aimed at evaluating the prevalence of indeterminate prognosis after application of this algorithm and providing a strategy for improving prognostication in this population.
Methods
We examined a prospective cohort of comatose CA patients (n = 485) in whom the ERC/ESICM algorithm was applied. In patients with an indeterminate outcome, prognostication was investigated using standardized EEG classification (benign, malignant, highly malignant) and serum neuron-specific enolase (NSE). Neurological recovery at 3 months was dichotomized as good (Cerebral Performance Categories [CPC] 1–2) vs. poor (CPC 3–5).
Results
Using the ERC/ESICM algorithm, 155 (32%) patients were prognosticated with poor outcome; all died at 3 months. Among the remaining 330 (68%) patients with an indeterminate outcome, the majority (212/330; 64%) showed good recovery. In this patient subgroup, absence of a highly malignant EEG by day 3 had 99.5 [97.4–99.9] % sensitivity for good recovery, which was superior to NSE < 33 μg/L (84.9 [79.3–89.4] % when used alone; 84.4 [78.8–89] % when combined with EEG, both p < 0.001). Highly malignant EEG had equal specificity (99.5 [97.4–99.9] %) but higher sensitivity than NSE for poor recovery. Further analysis of the discriminative power of outcome predictors revealed limited value of NSE over EEG.
Conclusions
In the majority of comatose CA patients, the outcome remains indeterminate after application of ERC/ESICM prognostication algorithm. Standardized EEG background analysis enables accurate prediction of both good and poor recovery, thereby greatly reducing uncertainty about coma prognostication in this patient population.



Similar content being viewed by others
Abbreviations
- BS:
-
Burst suppression;
- BSR:
-
Brainstem reflexes (including pupillary and corneal)
- CA:
-
Cardiac arrest
- CPC:
-
Cerebral Performance Category
- CT:
-
Brain computerized tomography
- ERC:
-
European Resuscitation Council
- ESICM:
-
European Society of Intensive Care Medicine
- EEG:
-
Electroencephalogram
- FPR:
-
False positive rate
- GCS:
-
Glasgow Coma Scale
- ICU:
-
Intensive care unit
- MRI:
-
Brain magnetic resonance imaging
- NPV:
-
Negative predictive value
- NSE:
-
Serum neuron-specific enolase
- PPV:
-
Positive predictive value
- ROC:
-
Receiving operator characteristic
- SE:
-
Status epilepticus
- SSEP:
-
Somatosensory-evoked potentials
- WLST:
-
Withdrawal of life-sustaining therapies
References
Laver S, Farrow C, Turner D, Nolan J (2004) Mode of death after admission to an intensive care unit following cardiac arrest. Intensiv Care Med 30:2126–2128. https://doi.org/10.1007/s00134-004-2425-z
Nolan JP, Ferrando P, Soar J et al (2016) Increasing survival after admission to UK critical care units following cardiopulmonary resuscitation. Crit Care Lond Engl 20:219. https://doi.org/10.1186/s13054-016-1390-6
Nobile L, Taccone FS, Szakmany T et al (2016) The impact of extracerebral organ failure on outcome of patients after cardiac arrest: an observational study from the ICON database. Crit Care. https://doi.org/10.1186/s13054-016-1528-6
Lemiale V, Dumas F, Mongardon N et al (2013) Intensive care unit mortality after cardiac arrest: the relative contribution of shock and brain injury in a large cohort. Intensiv Care Med 39:1972–1980. https://doi.org/10.1007/s00134-013-3043-4
Dragancea I, Wise MP, Al-Subaie N et al (2017) Protocol-driven neurological prognostication and withdrawal of life-sustaining therapy after cardiac arrest and targeted temperature management. Resuscitation 117:50–57. https://doi.org/10.1016/j.resuscitation.2017.05.014
Dragancea I, Rundgren M, Englund E et al (2013) The influence of induced hypothermia and delayed prognostication on the mode of death after cardiac arrest. Resuscitation 84:337–342. https://doi.org/10.1016/j.resuscitation.2012.09.015
Mulder M, Gibbs HG, Smith SW et al (2014) Awakening and withdrawal of life-sustaining treatment in cardiac arrest survivors treated with therapeutic hypothermia. Crit Care Med 42:2493–2499. https://doi.org/10.1097/CCM.0000000000000540
Nolan JP, Cariou A (2015) Post-resuscitation care: ERC–ESICM guidelines 2015. Intensiv Care Med 41:2204–2206. https://doi.org/10.1007/s00134-015-4094-5
Nolan JP, Soar J, Cariou A et al (2016) Erratum to: European Resuscitation Council and European Society of Intensive Care Medicine 2015 guidelines for post-resuscitation care. Intensiv Care Med 42:488–489. https://doi.org/10.1007/s00134-015-4158-6
Oddo M, Rossetti AO (2014) Early multimodal outcome prediction after cardiac arrest in patients treated with hypothermia. Crit Care Med 42:1340–1347. https://doi.org/10.1097/CCM.0000000000000211
Scarpino M, Lanzo G, Lolli F et al (2018) Neurophysiological and neuroradiological multimodal approach for early poor outcome prediction after cardiac arrest. Resuscitation 129:114–120. https://doi.org/10.1016/j.resuscitation.2018.04.016
Tsetsou S, Novy J, Pfeiffer C et al (2018) Multimodal outcome prognostication after cardiac arrest and targeted temperature management: analysis at 36 °C. Neurocrit Care 28:104–109. https://doi.org/10.1007/s12028-017-0393-8
Cronberg T (2019) Assessing brain injury after cardiac arrest, towards a quantitative approach. Curr Opin Crit Care 25:211–217. https://doi.org/10.1097/MCC.0000000000000611
Rossetti AO, Tovar Quiroga DF, Juan E et al (2017) Electroencephalography predicts poor and good outcomes after cardiac arrest: a two-center study. Crit Care Med 45:e674–e682. https://doi.org/10.1097/CCM.0000000000002337
Ruijter BJ, Tjepkema-Cloostermans MC, Tromp SC et al (2019) Early electroencephalography for outcome prediction of postanoxic coma: a prospective cohort study. Ann Neurol 86:203–214. https://doi.org/10.1002/ana.25518
Paul M, Bougouin W, Geri G et al (2016) Delayed awakening after cardiac arrest: prevalence and risk factors in the Parisian registry. Intensiv Care Med 42:1128–1136. https://doi.org/10.1007/s00134-016-4349-9
Gold B, Puertas L, Davis SP et al (2014) Awakening after cardiac arrest and post resuscitation hypothermia: are we pulling the plug too early? Resuscitation 85:211–214. https://doi.org/10.1016/j.resuscitation.2013.10.030
Rey A, Rossetti AO, Miroz J-P et al (2019) Late awakening in survivors of postanoxic coma: early neurophysiologic predictors and association with ICU and long-term neurologic recovery. Crit Care Med 47:85–92. https://doi.org/10.1097/CCM.0000000000003470
Eid SM, Albaeni A, Vaidya D et al (2016) Awakening following cardiac arrest: determined by the definitions used or the therapies delivered? Resuscitation 100:38–44. https://doi.org/10.1016/j.resuscitation.2015.12.017
Irisawa T, Vadeboncoeur TF, Karamooz M et al (2017) Duration of coma in out-of-hospital cardiac arrest survivors treated with targeted temperature management. Ann Emerg Med 69:36–43. https://doi.org/10.1016/j.annemergmed.2016.04.021
Sandroni C (2016) EEG for prognostication in postanoxic coma: what you predict depends on when you predict. Minerva Anestesiol 82:919–922
Geri G, Guillemet L, Dumas F et al (2015) Acute kidney injury after out-of-hospital cardiac arrest: risk factors and prognosis in a large cohort. Intensiv Care Med 41:1273–1280. https://doi.org/10.1007/s00134-015-3848-4
Bougouin W, Dumas F, Marijon E et al (2017) Gender differences in early invasive strategy after cardiac arrest: Insights from the PROCAT registry. Resuscitation 114:7–13. https://doi.org/10.1016/j.resuscitation.2017.02.005
Hirsch LJ, LaRoche SM, Gaspard N et al (2013) American clinical neurophysiology society’s standardized critical care EEG terminology: 2012 version. J Clin Neurophysiol 30:27
Westhall E, Rossetti AO, van Rootselaar A-F et al (2016) Standardized EEG interpretation accurately predicts prognosis after cardiac arrest. Neurology 86:1482–1490. https://doi.org/10.1212/WNL.0000000000002462
Perkins GD, Jacobs IG, Nadkarni VM et al (2015) Cardiac arrest and cardiopulmonary resuscitation outcome reports: update of the utstein resuscitation registry templates for out-of-hospital cardiac arrest. Resuscitation 96:328–340. https://doi.org/10.1016/j.resuscitation.2014.11.002
Hirsch LJ, Claassen J, Mayer SA, Emerson RG (2004) Stimulus-induced rhythmic, periodic, or ictal discharges (SIRPIDs): a common EEG phenomenon in the critically ill. Epilepsia 45:109–123
Rossetti AO, Rabinstein AA, Oddo M (2016) Neurological prognostication of outcome in patients in coma after cardiac arrest. Lancet Neurol 15:597–609. https://doi.org/10.1016/S1474-4422(16)00015-6
Wijman CAC, Mlynash M, Caulfield AF et al (2009) Prognostic value of brain diffusion weighted imaging after cardiac arrest. Ann Neurol 65:394–402. https://doi.org/10.1002/ana.21632
Grossestreuer AV, Abella BS, Leary M et al (2013) Time to awakening and neurologic outcome in therapeutic hypothermia-treated cardiac arrest patients. Resuscitation 84:1741–1746. https://doi.org/10.1016/j.resuscitation.2013.07.009
Howell K, Grill E, Klein A-M et al (2013) Rehabilitation outcome of anoxic-ischaemic encephalopathy survivors with prolonged disorders of consciousness. Resuscitation 84:1409–1415. https://doi.org/10.1016/j.resuscitation.2013.05.015
Lybeck A, Cronberg T, Aneman A et al (2018) Time to awakening after cardiac arrest and the association with target temperature management. Resuscitation 126:166–171. https://doi.org/10.1016/j.resuscitation.2018.01.027
Ponz I, Lopez-de-Sa E, Armada E et al (2016) Influence of the temperature on the moment of awakening in patients treated with therapeutic hypothermia after cardiac arrest. Resuscitation 103:32–36. https://doi.org/10.1016/j.resuscitation.2016.03.017
Acknowledgements
The authors thank John-Paul Miroz, RN, Jan Novy, MD PhD, Christine Stähli, RN and Laura Pezzi, RN, for their help in data collection, and EEG retrieval and analysis.
Funding
Mauro Oddo and Andrea O. Rossetti are supported by the Swiss National Science Foundation.
Author information
Authors and Affiliations
Contributions
FB and FR equally contributed to data acquisition and analysis, and drafted the manuscript; GB performed EEG analysis and classification; ADR provided expert supervision of statistical analysis; AOR supervised EEG analysis and classification, contributed to data acquisition and analysis, and critically revised the manuscript; FST revised the manuscript and provided important intellectual contribution; CS and MO equally contributed to supervise the concept and design of the study, data analysis and interpretation, and critically revised the manuscript. All authors approved and agreed on the final version of the manuscript. This article is reported according to the STARD 2015 guidelines (https://www.equator-network.org/reporting-guidelines/stard/).
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no competing interests.
Ethics approval
Approval was obtained from the Ethical Research Committee of the University of Lausanne, and waiver of consent was allowed since all examinations were part of standard patient care.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Bongiovanni, F., Romagnosi, F., Barbella, G. et al. Standardized EEG analysis to reduce the uncertainty of outcome prognostication after cardiac arrest. Intensive Care Med 46, 963–972 (2020). https://doi.org/10.1007/s00134-019-05921-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-019-05921-6