Abstract
Purpose
Few data are available about optimal nutrition modalities in mechanically ventilated patients with shock. Our objective was to assess associations linking early nutrition (<48 h after intubation), feeding route and calorie intake to mortality and risk of ventilator-associated pneumonia (VAP) in patients with invasive mechanical ventilation (IMV) and shock.
Methods
In the prospective OutcomeRea database, we identified adults with IMV >72 h and shock (arterial systolic pressure <90 mmHg) within 48 h after intubation. A marginal structural Cox model was used to create a pseudo-population in which treatment was unconfounded by subject-specific characteristics.
Results
We included 3,032 patients. Early nutrition was associated with lower day-28 mortality [HR 0.89, 95 % confidence interval (CI) 0.81–0.98, P = 0.01] and day-7 mortality (HR 0.76, CI 0.66–0.87, P < 0.001) but not with lower day-7 to day-28 mortality (HR 1.00, CI 0.89–1.12, P = 0.98). Early nutrition increased VAP risk over the 28 days (HR 1.08, CI 1.00–1.17, P = 0.046) and until day 7 (HR 7.17, CI 6.27–8.19, P < 0.001) but decreased VAP risk from days 7 to 28 (HR 0.85, CI 0.78–0.92, P < 0.001). Compared to parenteral feeding, enteral feeding was associated with a slightly increased VAP risk (HR 1.11, CI 1.00–1.22, P = 0.04) but not with mortality. Neither mortality nor VAP risk differed between early calorie intakes of ≥20 and <20 kcal/kg/day.
Conclusion
In mechanically ventilated patients with shock, early nutrition was associated with reduced mortality. Neither feeding route nor early calorie intake was associated with mortality. Early nutrition and enteral feeding were associated with increased VAP risk.
Similar content being viewed by others
Introduction
Critical illnesses produce calorie and protein deficiencies due to increased catabolism and decreased oral nutrient intake. International guidelines recommend starting artificial nutrition within 24–48 h after intensive care unit (ICU) admission, preferably by the enteral route, with target intakes of 20–25 kcal/kg/day and 1.2–2 g protein/kg/day during the first week [1–4]. Adherence to these guidelines is poor [5, 6]. Early enteral nutrition (EN) raises major challenges, with 30–70 % of patients experiencing vomiting, which may increase their risk of ventilator-associated pneumonia (VAP) [7]. EN is often stopped during periods with vomiting and for planned diagnostic or therapeutic procedures, leading to lower calorie intakes [8, 9].
The increased morbidity and mortality of mechanically ventilated patients with shock is associated with major nutritional deficiencies [6, 10–15]. A severe inflammatory response, metabolic stress and no spontaneous food intake combine to cause nutritional deficiencies. Additional factors include gut dysfunction, EN intolerance, delayed absorption of nutrients, and gut ischemia with subsequent bacterial translocation and multi-organ failure [7, 13, 16]. Studies have investigated EN in patients treated for shock [6, 10, 12]. Whether EN exacerbates or alleviates gut ischemia in these patients is unknown [17–20]. Guidelines indicate that EN should be withheld or delayed in patients with haemodynamic instability or catecholamine therapy [2, 3]. A recent randomised controlled trial showed that early EN and early parenteral nutrition (PN) were associated with similar outcomes and infection rates [21]. However, the benefits from early EN may be greatest in those patients with the most severe critical illnesses [11]. No high-level evidence is available on whether early versus delayed feeding is associated with outcomes of patients with shock receiving invasive mechanical ventilation (IMV). Also controversial are the relative merits of EN versus PN and the optimal macronutrient intake [5, 6, 22, 23].
Here, our main purpose was to compare effects of both early versus late nutrition and EN versus PN on outcomes of patients with shock and IMV. We also assessed potential effects of the early calorie intake on patient outcomes. We used a large prospective database (OutcomeRea) and we built a marginal structural model to create a pseudo-randomised population, thereby reducing any influence of confounding factors.
Methods
Study design and setting
We performed a multicentre cohort study using the OutcomeRea prospective database [24]. Detailed demographic, clinical and outcome data of patients were entered prospectively into the OutcomeRea database by trained senior physicians or clinical research monitors in each participating ICU (details in the online supplement).
In accordance with French law, this observational study involving no changes in patient management and using an approved database did not require informed consent of the patients for study participation.
Participants
Eligible patients were consecutive adults (≥18 years) who were included in the OutcomeRea database between December 1996 and February 2013, received IMV for longer than 72 h and developed shock (arterial systolic pressure <90 mmHg) within 48 h after IMV initiation. Exclusion criteria were abdominal surgery within the past month and treatment-limitation decisions on admission.
Definitions
Patient groups
To study the effect of nutrition timing, we distinguished patients given nutrition within 48 h after intubation (early-nutrition group) vs. later (delayed-nutrition group). To assess the impact of the early feeding route, patients given early nutrition were separated into a PN group, given only PN, and an EN group, given EN with or without PN, during the first 3 days of nutritional support (Fig. 1).
Diagnosis of ventilator-associated pneumonia (VAP)
VAP episodes were recorded until day 2 after extubation. VAP was suspected in patients who had new and persistent or progressive infiltrates on the chest radiograph with at least two of the following criteria: peripheral leucocytosis (>10,000/mm3), leucopenia (<4,000/mm3), body temperature ≥38.5 or ≤35.5 °C, and purulent tracheal aspirates. In all study ICUs, the criterion for confirming VAP was a positive quantitative bacteriologic culture of respiratory tract material obtained by broncho-alveolar lavage [cut-off ≥104 colony-forming units (cfu)/mL], protected specimen brush (cut-off ≥103 cfu/mL) or tracheobronchial aspirate (cut-off ≥105 cfu/mL) [25].
Data collection
The following data were collected at ICU admission: age, sex, comorbidities, Simplified Acute Physiology Score II (SAPS II), height, weight, diagnostic category (medical, emergent surgery, scheduled surgery) and acute illness. Treatments (fluid load, vasoactive drugs, hypnotic drugs, opiates, neuromuscular blocking agents, antibiotics, proton pump inhibitor and insulin) and the Sequential Organ Failure Assessment (SOFA) score were collected at intubation. Feeding route was recorded daily. Daily calorie intake was recorded starting in 2005, in three categories: <20, 20–35 and >35 kcal/kg/day. Data were collected until death or day 28.
Statistical analysis
Patient characteristics were described as n (%) or median [interquartile range, IQR] for qualitative and quantitative variables, respectively. Chi square or Mann–Whitney tests were used to compare groups, as appropriate. The primary endpoint was day-28 mortality and the secondary endpoint was VAP risk as assessed by day-28 VAP-free survival. Risk factors for day-28 events were identified using univariate Cox models stratified by centre; we successively tested early nutrition, feeding route and calorie intake as risk factors for day-28 mortality and day-28 VAP-free survival. We developed a propensity score to predict the probability of risk-factor exposure (early nutrition, feeding route and calorie intake) in each patient. Because early nutrition was not randomised, we developed a propensity score that used the admission variables to predict the probability of early nutrition in a given patient. All variables associated with early nutrition were entered into the model (Table E1 in the online supplement). According to the marginal structural model approach, this propensity score was used to compute the inverse probability treatment weighted estimator (IPTW) for early nutrition. We thus obtained a pseudo-population in which all patients had the same probability of receiving early nutrition, as if they had been allocated to early nutrition at random [26]. Then, the effect of early nutrition on day-28 mortality and day-28 VAP-free survival was estimated using a Cox model, weighted by the IPTW for early nutrition, stratified by centre and adjusted for risk factors for the study events. The additional survival duration in the early-nutrition group was calculated using an accelerated failure time model.
In subgroup analyses, we compared early EN versus early PN and calorie intake <20 vs. ≥20 kcal/kg/day. The proportional risk assumption was tested using the Kolmogorov-type supremum test [27]. When it was not satisfied, we separately analysed the risk of death using the best cut-off, as determined graphically. Truncation of extreme weights was used to validate the final models (Table E2) [26].
Last, subgroup analyses were performed for patients suffering from renal or liver failure. Patients with liver or renal values of the SOFA score >0 were considered as having a liver or a renal failure, respectively.
Results
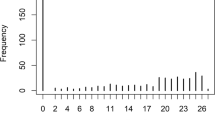
Of the 16,789 patients recorded in the database, 3,032 met our eligibility criteria and were included in the analysis (Fig. 1). Table 1 reports their main characteristics and outcomes.
Early nutrition
Of the 3,032 study patients, 1,861 received early nutrition and 1,171 delayed nutrition. Table 2 lists the main characteristics of both groups. Median ICU stay length was 14 days [IQR 8–24 days] in the early-nutrition group and 9 days [6–17 days] in the delayed-nutrition group (P < 0.001). Crude day-28 mortality rates were 32.4 % with early nutrition and 29.2 % with delayed nutrition (P = 0.06). Table E1 lists the variables tested as factors potentially associated with early nutrition.
Effect of early nutrition on mortality
Table E2 reports the results of the univariate analysis. After adjustment for confounders, early nutrition was associated with decreased day-28 mortality [hazards ratio (HR) 0.89, 95 % confidence interval (95 % CI) 0.81–0.98, P = 0.01] (Table 3). The Kolmogorov-type supremum test based on a sample of 1,000 simulated residual patterns showed that the effect on mortality varied over time (P = 0.03). In a multivariate Cox model, the early nutrition group had lower mortality within 7 days after intubation (HR 0.76, 95 % CI 0.66–0.87, P < 0.001) but not from day 7 to day 28 (HR 1.00, 95 % CI 0.89–1.12, P = 0.98) (Table 3). The additional survival duration of the early nutrition group was 3.3 days (95 % CI 0.8–6.2). Subgroup analyses showed that early nutrition was associated with decreased day-28 mortality in patients with renal failure (HR 0.87, 95 % CI 0.77–0.97, P = 0.02), but not in patients with liver failure (HR 0.99, 95 % CI 0.83–1.19, P = 0.93) (Tables E5, E6).
Effect of early nutrition on VAP risk
After adjustment for confounders, early nutrition was associated with an increase in VAP risk (HR 1.08, 95 % CI 1.00–1.17, P = 0.046) (Table 3). This effect varied significantly with time (P < 0.001). By multivariate analysis, the early nutrition group was at higher VAP risk within 7 days after intubation (HR 7.17, 95 % CI 6.27–8.19, P < 0.001) but at lower VAP risk 7–28 days after intubation (HR 0.85, 95 % CI 0.78–0.92, P < 0.001) (Table 3). Early nutrition was not associated with significant change in VAP risk in patients with renal failure (HR 1.04, 95 % CI 0.94–1.15, P = 0.43) or liver failure (HR 1.05, 95 % CI 0.90–1.22, P = 0.58) (Tables E5, E6).
Feeding route
Of the 1,861 patients given early nutrition, 481 received only PN and 1,380 received EN (only EN, n = 1,187; EN + PN, n = 193) (Table 4). Median duration of IMV was 9 days [5–10 days] in the PN group and 10 days [IQR 5–17 days] in the EN group (P = 0.21). Median ICU stay length was 14 days [8–25 days] in the PN group and 14 days [IQR 8–23 days] in the EN group (P = 0.96). Crude day-28 mortality rates were 31.8 % in the PN group and 32.6 % in the EN group (P = 0.75). Table E3 lists the variables tested as potentially associated with receiving EN.
Effect of feeding route on mortality
By multivariate analysis performed after checking that model assumptions were met, EN was not associated with lower mortality compared to PN (HR 1.07, 95 % CI 0.95–1.20, P = 0.27) (Table 3). When we confined the EN group to those patients who received no PN (i.e. to 1,187/1,380 patients given EN), we obtained similar results (HR 1.18, 95 % CI 0.98–1.44, P = 0.08).
EN was associated with increased day-28 mortality in patients with renal failure (HR 1.43, 95 % CI 1.23–1.67, P < 0.001) or with liver failure (HR 1.68, 95 % CI 1.34–2.10, P < 0.001). Feeding route had no impact on mortality in patients without renal failure or without liver failure (Tables E5, E6).
Effect of feeding route on VAP risk
Compared to PN, EN was associated with a higher risk of VAP (HR 1.11, 95 % CI 1.00–1.22, P = 0.04) (Table 3). When we compared the 1,187 patients who received only EN to the 481 patients who received only PN, we found a non-significant association between EN and VAP risk (HR 1.17, 95 % CI 1.00–1.38, P = 0.06).
EN was associated with VAP in patients with renal failure (HR 1.23, 95 % CI 1.08–1.41, P = 0.002) or liver failure (HR 1.25, 95 % CI 1.03–1.53, P = 0.03). Feeding route was not associated with VAP in patients without renal failure or without liver failure (Tables E5, E6).
Calorie intake
Among 2,276 patients fed within 3 days after intubation, 1,398 had their calorie intake recorded in the database. Their main data are shown in Table E4. Calorie intake was not associated with day-28 mortality (HR 0.96, 95 % CI 0.83–1.12, P = 0.63) or VAP risk (HR 0.9, 95 % CI 0.8–1.01, P = 0.08) (Table 3).
In patients with renal failure, calorie intake was not associated with day-28 mortality (HR 0.81, 95 % CI 0.64–1.02, P = 0.07), but calorie intake ≥20 kcal/kg/day was associated with decreased VAP risk (HR 0.68, 95 % CI 0.57–0.83, P < 0.001) compared to calorie intake <20 kcal/kg/day. In patients with liver failure, calorie intake was associated with neither day-28 mortality (HR 1.06, 95 % CI 0.75–1.49, P = 0.75) nor VAP risk (HR 1.20, 95 % CI 0.88–1.63, P = 0.26) (Tables E5, E6).
Discussion
Our study based on a marginal structural Cox model and a large prospective high-quality database of patients with shock receiving IMV demonstrated that early nutrition, within 48 h after intubation, was associated with decreases in the risks of death and VAP. Neither the route of early nutrition nor delivery of less than 20 kcal/kg/day during the first few days of IMV was associated with mortality or risk of VAP.
A major finding from our study is that early nutrition was associated with decreased mortality in patients with shock and IMV, compared to delayed nutrition. This finding was entirely related to a decrease in mortality during the first 7 days of IMV. We are not aware of other studies investigating associations between early nutrition and outcomes of ICU patients, regardless of route of delivery. As EN is generally considered preferable over PN, previous studies, including meta-analyses, compared early EN to delayed EN. Guidelines recommend EN initiation as early as possible, and never later than 48 h after ICU admission [1–3]. However, data on outcomes associated with early EN are conflicting. In a retrospective multicentre study of over 4,000 patients receiving IMV, EN started within 48 h of MV onset was associated with a significantly decreased mortality, and this association was chiefly ascribable to the sickest patients [11]. Our study shows that the association between early nutrition and survival is robust even after adjusting for possible confounders. One meta-analysis suggested that early EN delivered within 36 h after hospital admission or surgery might decrease infections and hospital stay length but not mortality [28], whereas another showed significant decreases in mortality and pneumonia rates with early EN within 24 h of injury or ICU admission versus delayed EN [29]. However, the overall quality of the studies included in these meta-analyses was poor. More recently, an observational study suggested decreased mortality with EN started within 48 h of intubation versus delayed EN in patients receiving IMV and vasopressors [12]. However, the definition of early EN remains unclear and varies across studies and guidelines, depending on the landmark used (e.g. hospital admission, ICU admission, onset of illness, or intubation). Early EN was usually defined as EN initiation within 24–48 h after the landmark. In our study, we chose intubation as the landmark, as intubated patients are completely unable to eat. Our choice of a 48-h interval since intubation to define early EN is consistent with several recent studies on early EN in patients receiving MV [11, 12, 30, 31]. Two randomised trials focussing on the best time for starting supplemental PN in patients intolerant to EN yielded conflicting results [22, 32]. A recent randomised trial in patients with contraindications to EN demonstrated decreases in costs and IMV duration but no impact on mortality or ICU stay length with PN started within 24 h of ICU admission compared to standard care [33, 34]. However, in the standard-care group, 56.5 % of patients received PN within 3 days after admission and 29.2 % received EN despite contraindications to this route. Finally, a very recent randomised trial compared early EN to early PN (both initiated within 36 h after ICU admission) in unselected ICU patients and found no differences in outcomes [21]. Our study is thus the first to suggest a clear benefit from early nutrition, delivered enterally or parenterally, in patients with severe critical illnesses.
Another striking finding from our study is that the feeding route in patients with early shock and IMV was not associated with survival in the overall study population. This result is consistent with those from a study in unselected critically ill patients [21]. In our EN group, the risk of VAP was increased during the first 7 days but was decreased later on. Although EN is widely viewed as better than PN in ICU patients, this opinion does not rest on sound scientific evidence [35, 36]. According to several studies, EN may improve gut mucosal integrity, decrease nosocomial infections and organ failures, and improve outcomes, compared to PN. However, a meta-analysis comparing early EN to early PN in hospitalised patients showed fewer infections with EN but no effect on mortality [37]. In another meta-analysis, mortality was lower with PN than EN [38, 39]. In our study, results in patients with renal or liver failure suggest that early EN might be deleterious in the most severely ill patients with IMV and shock. Studies focussing specifically on shock showed that many patients received PN despite having no contraindications to EN [5, 6]. Guidelines indicate that EN should be withheld or delayed in patients with haemodynamic instability or catecholamine therapy, who make up over 50 % of all patients receiving IMV [2, 3]. Our results suggest that PN may be the best first-line route for early nutrition in patients with IMV and shock. Further work is needed to assess this possibility.
The mechanisms underlying the survival benefits associated with early nutrition in our study are unclear. Delaying nutrition allows more time for nutritional deficiencies to develop [40–42]. However, no accurate information exists on the calorie requirements of individual ICU patients, which may depend on the disease, pre-existing nutritional status and acute illness severity. In recent studies, lower calorie intakes than recommended in guidelines were associated with similar or improved outcomes [22, 23, 43]. In our work, patients given less than 20 kcal/kg/day during the first few days of IMV had similar outcomes to those with higher calorie intakes. Thus, complete (or nearly complete) absence of nutrient supply during the first few ICU days may have a greater adverse effect on outcomes of patients with shock and IMV than the amount of nutrients supplied. The optimal calorie and protein supply in early stage critical illnesses remains to be determined, and one possibility is that supplies exceeding a certain amount may be deleterious [22, 34]. Thus, during the early management of patients with shock and IMV, low-volume trophic feeding might deserve consideration not only for EN but also for PN. The main goal of nutritional support does not seem to be maintenance of gut mucosal integrity, but, instead, maintenance of immune function, tissue repair mechanisms and muscle mass.
Our study has several limitations. First, the database was not specifically designed for the study and contained no details on micronutrient supply, EN intolerance, glycaemia control, calorie and protein targets for individual patients, reasons for delayed nutrition, feeding formulae, exact nutritional and non-nutritional calorie intakes, actual nurse-to-patient ratio, feeding protocol of each ICU or treatment limitation decisions. Thus, we cannot exclude that between-group differences in these variables may have influenced our results. Second, the study was observational and the interventions were not randomised. Nutritional support modalities were not standardised but instead complied with the protocols of each ICU. Furthermore, substantial changes in ICU management have occurred over the 16-year inclusion period. The randomised controlled design remains the reference standard for demonstrating causal relationships between interventions and outcomes. Nevertheless, observational studies are more relevant to everyday practice. Moreover, by using propensity score analysis and minimising potential confounding, we produced comparable groups. However, we cannot rule out the existence of residual confounding factors. The major strengths of our study are the powerful design and large number of patients enrolled in numerous ICUs across France. We are confident that these strengths produced robust, reliable and widely applicable findings. Last, our study does not provide information on the physiological mechanisms underlying the survival benefits associated with early nutrition. This point deserves further investigation.
Conclusion
Our results obtained using a marginal structural model design strongly suggest that ICU patients with shock may benefit from starting nutritional support early after IMV initiation. Neither feeding route nor early calorie intake was associated with mortality. Despite our careful methodology involving a propensity score analysis to eliminate the potential impact of confounders, the results of our observational study require further evaluation using a randomised controlled design.
References
Heyland DK, Dhaliwal R, Drover JW, Gramlich L, Dodek P (2003) Canadian clinical practice guidelines for nutrition support in mechanically ventilated, critically ill adult patients. JPEN J Parenter Enteral Nutr 27:355–373
Kreymann KG, Berger MM, Deutz NE, Hiesmayr M, Jolliet P, Kazandjiev G, Nitenberg G, van den Berghe G, Wernerman J, Ebner C, Hartl W, Heymann C, Spies C (2006) ESPEN guidelines on enteral nutrition: intensive care. Clin Nutr 25:210–223
McClave SA, Martindale RG, Vanek VW, McCarthy M, Roberts P, Taylor B, Ochoa JB, Napolitano L, Cresci G (2009) Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (ASPEN). JPEN J Parenter Enteral Nutr 33:277–316
Hurel D, Lefrant JY, Cano NJ, Ichai C, Preiser JC, Tamion F (2014) Nutrition artificielle en réanimation. Guidelines for nutrition support in critically ill patient. Réanimation 23:332–350
Cahill NE, Dhaliwal R, Day AG, Jiang X, Heyland DK (2010) Nutrition therapy in the critical care setting: what is “best achievable” practice? An international multicenter observational study. Crit Care Med 38:395–401
Elke G, Schadler D, Engel C, Bogatsch H, Frerichs I, Ragaller M, Scholz J, Brunkhorst FM, Loffler M, Reinhart K, Weiler N (2008) Current practice in nutritional support and its association with mortality in septic patients—results from a national, prospective, multicenter study. Crit Care Med 36:1762–1767
Blaser AR, Starkopf J, Kirsimagi U, Deane AM (2014) Definition, prevalence, and outcome of feeding intolerance in intensive care: a systematic review and meta-analysis. Acta Anaesthesiol Scand 58:914–922
Passier RH, Davies AR, Ridley E, McClure J, Murphy D, Scheinkestel CD (2013) Periprocedural cessation of nutrition in the intensive care unit: opportunities for improvement. Intensive Care Med 39:1221–1226
Mentec H, Dupont H, Bocchetti M, Cani P, Ponche F, Bleichner G (2001) Upper digestive intolerance during enteral nutrition in critically ill patients: frequency, risk factors, and complications. Crit Care Med 29:1955–1961
Berger MM, Revelly JP, Cayeux MC, Chiolero RL (2005) Enteral nutrition in critically ill patients with severe hemodynamic failure after cardiopulmonary bypass. Clin Nutr 24:124–132
Artinian V, Krayem H, DiGiovine B (2006) Effects of early enteral feeding on the outcome of critically ill mechanically ventilated medical patients. Chest 129:960–967
Khalid I, Doshi P, DiGiovine B (2010) Early enteral nutrition and outcomes of critically ill patients treated with vasopressors and mechanical ventilation. Am J Crit Care 19:261–268
Mutlu GM, Mutlu EA, Factor P (2001) GI complications in patients receiving mechanical ventilation. Chest 119:1222–1241
Alberda C, Gramlich L, Jones N, Jeejeebhoy K, Day AG, Dhaliwal R, Heyland DK (2009) The relationship between nutritional intake and clinical outcomes in critically ill patients: results of an international multicenter observational study. Intensive Care Med 35:1728–1737
Ekpe K, Novara A, Mainardi JL, Fagon JY, Faisy C (2014) Methicillin-resistant Staphylococcus aureus bloodstream infections are associated with a higher energy deficit than other ICU-acquired bacteremia. Intensive Care Med 40:1878–1887
Deane AM, Rayner CK, Keeshan A, Cvijanovic N, Marino Z, Nguyen NQ, Chia B, Summers MJ, Sim JA, van Beek T, Chapman MJ, Horowitz M, Young RL (2014) The effects of critical illness on intestinal glucose sensing, transporters, and absorption. Crit Care Med 42:57–65
Mancl EE, Muzevich KM (2013) Tolerability and safety of enteral nutrition in critically ill patients receiving intravenous vasopressor therapy. JPEN J Parenter Enteral Nutr 37:641–651
Thibault R, Pichard C, Wernerman J, Bendjelid K (2011) Cardiogenic shock and nutrition: safe? Intensive Care Med 37:35–45
Gatt M, MacFie J, Anderson AD, Howell G, Reddy BS, Suppiah A, Renwick I, Mitchell CJ (2009) Changes in superior mesenteric artery blood flow after oral, enteral, and parenteral feeding in humans. Crit Care Med 37:171–176
Rokyta R Jr, Matejovic M, Krouzecky A, Novak I (2003) Enteral nutrition and hepatosplanchnic region in critically ill patients—friends or foes? Physiol Res 52:31–37
Harvey SE, Parrott F, Harrison DA, Bear DE, Segaran E, Beale R, Bellingan G, Leonard R, Mythen MG, Rowan KM (2014) Trial of the route of early nutritional support in critically ill adults. N Engl J Med 371:1673–1684
Casaer MP, Mesotten D, Hermans G, Wouters PJ, Schetz M, Meyfroidt G, Van Cromphaut S, Ingels C, Meersseman P, Muller J, Vlasselaers D, Debaveye Y, Desmet L, Dubois J, Van Assche A, Vanderheyden S, Wilmer A, Van den Berghe G (2011) Early versus late parenteral nutrition in critically ill adults. New Engl J Med 365:506–517
Rice TW, Wheeler AP, Thompson BT, Steingrub J, Hite RD, Moss M, Morris A, Dong N, Rock P (2012) Initial trophic vs full enteral feeding in patients with acute lung injury: the EDEN randomized trial. JAMA 307:795–803
OUTCOMEREA Promotion et Developpement de la Recherche et de l’Enseignement en Reanimation (2014) http://www.outcomerea.org. Accessed 21 Feb 2014
Chastre J, Fagon JY (2002) Ventilator-associated pneumonia. Am J Respir Crit Care Med 165:867–903
Cole SR, Hernan MA (2008) Constructing inverse probability weights for marginal structural models. Am J Epidemiol 168:656–664
Lin DY, Wei LJ, Ying Z (1993) Checking the Cox model with cumulative sums of martingale-based residuals. Biometrika 80:557–572
Marik PE, Zaloga GP (2001) Early enteral nutrition in acutely ill patients: a systematic review. Crit Care Med 29:2264–2270
Doig GS, Heighes PT, Simpson F, Sweetman EA, Davies AR (2009) Early enteral nutrition, provided within 24 h of injury or intensive care unit admission, significantly reduces mortality in critically ill patients: a meta-analysis of randomised controlled trials. Intensive Care Med 35:2018–2027
Reignier J, Dimet J, Martin-Lefevre L, Bontemps F, Fiancette M, Clementi E, Lebert C, Renard B (2009) Before-after study of a standardized ICU protocol for early enteral feeding in patients turned in the prone position. Clin Nutr 29(2):210–216
Reignier J, Mercier E, Le Gouge A, Boulain T, Desachy A, Bellec F, Clavel M, Frat JP, Plantefeve G, Quenot JP, Lascarrou JB (2013) Effect of not monitoring residual gastric volume on risk of ventilator-associated pneumonia in adults receiving mechanical ventilation and early enteral feeding: a randomized controlled trial. JAMA 309:249–256
Heidegger CP, Berger MM, Graf S, Zingg W, Darmon P, Costanza MC, Thibault R, Pichard C (2013) Optimisation of energy provision with supplemental parenteral nutrition in critically ill patients: a randomised controlled clinical trial. Lancet 381:385–393
Doig GS, Simpson F (2013) Early parenteral nutrition in critically ill patients with short-term relative contraindications to early enteral nutrition: a full economic analysis of a multicenter randomized controlled trial based on US costs. Clin Econ Outcomes Res 5:369–379
Doig GS, Simpson F, Sweetman EA, Finfer SR, Cooper DJ, Heighes PT, Davies AR, O’Leary M, Solano T, Peake S (2013) Early parenteral nutrition in critically ill patients with short-term relative contraindications to early enteral nutrition: a randomized controlled trial. JAMA 309:2130–2138
Ziegler TR (2011) Nutrition support in critical illness–bridging the evidence gap. New Eng J Med 365:562–564
Desai SV, McClave SA, Rice TW (2014) Nutrition in the ICU: an evidence-based approach. Chest 145:1148–1157
Peter JV, Moran JL, Phillips-Hughes J (2005) A metaanalysis of treatment outcomes of early enteral versus early parenteral nutrition in hospitalized patients. Crit Care Med 33:213–220 (Discussion 260–211)
Simpson F, Doig GS (2005) Parenteral vs. enteral nutrition in the critically ill patient: a meta-analysis of trials using the intention to treat principle. Intensive Care Med 31:12–23
Doig GS (2013) Parenteral versus enteral nutrition in the critically ill patient: additional sensitivity analysis supports benefit of early parenteral compared to delayed enteral nutrition. Intensive Care Med 39:981–982
Singer P, Anbar R, Cohen J, Shapiro H, Shalita-Chesner M, Lev S, Grozovski E, Theilla M, Frishman S, Madar Z (2011) The tight calorie control study (TICACOS): a prospective, randomized, controlled pilot study of nutritional support in critically ill patients. Intensive Care Med 37:601–609
Tsai JR, Chang WT, Sheu CC, Wu YJ, Sheu YH, Liu PL, Ker CG, Huang MC (2011) Inadequate energy delivery during early critical illness correlates with increased risk of mortality in patients who survive at least seven days: a retrospective study. Clin Nutr 30:209–214
Villet S, Chiolero RL, Bollmann MD, Revelly JP, Cayeux RNM, Delarue J, Berger MM (2005) Negative impact of hypocaloric feeding and energy balance on clinical outcome in ICU patients. Clin Nutr 24:502–509
Casaer MP, Wilmer A, Hermans G, Wouters PJ, Mesotten D, Van den Berghe G (2013) Role of disease and macronutrient dose in the randomized controlled EPaNIC trial: a post hoc analysis. Am J Respir Crit Care Med 187:247–255
Acknowledgments
We are indebted to A. Wolfe, MD, for assistance in preparing and reviewing the manuscript. We are grateful to all staff physicians, staff nurses and research nurses at the study sites for their crucial contribution to the successful conduct of the study.
Conflicts of interest
All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflict of Interest and none reported any such conflict.
Funding
The study was funded by the non-profit OutcomeRea network. The OutcomeRea network took full administrative responsibility for data management, analysis and interpretation; and for manuscript preparation, review and approval.
Author information
Authors and Affiliations
Corresponding author
Additional information
Take-home message: In spite of experimental evidence, few clinical data exist for determining whether nutritional support should be started early, which feeding route should be used and how many calories should be provided in mechanically ventilated patients with shock. A marginal structural model study of a large, prospective database strongly suggests that mechanically ventilated patients with shock should be started on nutritional support within 48 h after mechanical ventilation initiation and that neither feeding route nor early calorie intake is associated with mortality.
On behalf of the OUTCOMEREA Study Group.
The members of the OUTCOMEREA Study Group are listed in the "Appendix".
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendix: OutcomeRea network
Appendix: OutcomeRea network
Scientific committee
Jean-François Timsit (Hôpital Albert Michallon and INSERM U823, Grenoble, France), Elie Azoulay (Medical ICU, Hôpital Saint Louis, Paris, France), Yves Cohen (ICU, Hôpital Avicenne, Bobigny, France), Maïté Garrouste-Orgeas (ICU, Hôpital Saint-Joseph, Paris, France), Lilia Soufir (ICU, Hôpital Saint-Joseph, Paris, France), Alban Le Monnier (Microbiology Department, Hôpital Saint-Joseph, Paris, France), Jean-Ralph Zahar (Microbiology Department, CHU Angers, France), Christophe Adrie (ICU, Hôpital Delafontaine, Saint Denis, France), Michael Darmon (Medical ICU, Hôpital St Etienne, France), Corinne Alberti (Hôpital Robert Debré, Paris France) and Christophe Clec’h (ICU, Hôpital Avicenne, Bobigny).
Biostatistical and informatics expertise
Jean-Francois Timsit (Hôpital Albert Michallon and Integrated Research Centre U823, Grenoble, France), Corinne Alberti (Medical Computer Sciences and Biostatistics Department, Hôpital Robert Debré, Paris, France), Sebastien Bailly (Integrated Research Centre U823, Grenoble, France), Stephane Ruckly (Outcomerea, INSERM UMR 1137, Paris, France), Christophe Clec’h (ICU, Hôpital Avicenne, Bobigny, France) and Aurélien Vannieuwenhuyze (Tourcoing, France).
OutcomeRea database investigators
Christophe Adrie (ICU, Hôpital Delafontaine, Saint Denis, France; and Physiology Department, Hôpital Cochin, Paris, France), Bernard Allaouchiche (surgical ICU, Hôpital Edouard Herriot, Lyon, France), Claire Ara-Somohano (Hôpital Albert Michallon, Grenoble, France), Laurent Argaud (medical ICU, Hôpital Edouard Herriot, Lyon, France), Francois Barbier (ICU, Hôpital d’Orléans, Orléans, France), Jean-Pierre Bédos (ICU, Hôpital André Mignot, Versailles, France), Agnès Bonadona (Hôpital Albert Michallon, Grenoble, France), Anne Laure Borel (Nutrition, Hôpital Albert Michallon, Grenoble), Caroline Bornstain (ICU, Hôpital de Montfermeil, Montfermeil, France), Lila Bouadma (ICU, Hôpital Bichat-Claude Bernard, Paris, France), Alexandre Boyer (ICU, Hôpital Pellegrin, Bordeaux, France), Christophe Clec’h (ICU, Hôpital Avicenne, Bobigny, France), Yves Cohen (ICU, Hôpital Avicenne, Bobigny, France), Jean-Pierre Colin (ICU, Hôpital de Dourdan, Dourdan, France), Michael Darmon (ICU, Hôpital Saint-Etienne, Saint-Etienne, France), Anne-Sylvie Dumenil (Hôpital Antoine Béclère, Clamart, France), Maïté Garrouste-Orgeas (ICU, Hôpital Saint-Joseph, Paris, France), Antoine Gros (ICU, Hôpital André Mignot, Versailles, France), Rebecca Hamidfar-Roy (Hôpital Albert Michallon, Grenoble, France), Hakim Haouache (surgical ICU, Hôpital Henri Mondor, Creteil, France), Samir Jamali (ICU, Hôpital de Dourdan, Dourdan, France), Hatem Kallel (ICU, Hôpital de Cayenne, Cayenne, France), Christian Laplace (ICU, Hôpital Kremlin-Bicêtre, Bicêtre, France), Alexandre Lautrette (ICU, Hôpital Gabriel-Montpied, Clermont-Ferrand, France), Guillaume Marcotte (surgical ICU, Hôpital Edouard Herriot, Lyon, France), Benoit Misset (ICU, Hôpital St Joseph, Paris, France), Laurent Montesino (ICU, Hôpital Bichat, Paris, France), Bruno Mourvillier (ICU, Hôpital Bichat, Paris, France), Guillaume Lacave (ICU, Hôpital André Mignot, Versailles, France), Virgine Lemiale (ICU, Hôpital Saint-Louis, Paris, France), Virginie Laurent (ICU, Hôpital André Mignot, Versailles, France), Eric Marriotte (ICU, Hopital Bichat, Paris, France), Benjamin Planquette (ICU, Hôpital André Mignot, Versailles, France), Jean Reignier (ICU, Centre Hospitalier Départemental, La Roche sur Yon, France), Romain Sonneville (ICU, Hôpital Bichat-Claude Bernard, Paris, France), Bertrand Souweine (ICU, Hôpital Gabriel-Montpied, Clermont-Ferrand, France), Carole Schwebel (Hôpital Albert Michallon, Grenoble, France), Gilles Troché (ICU, Hôpital André Mignot, Versailles, France), Marie Thuong (ICU, Hôpital de Pontoise, Pontoise, France), Dany Goldgran-Toledano (Centre Hospitalier de Gonesse, Gonesse, France) and Eric Vantalon (surgical ICU, Hôpital Saint-Joseph, Paris, France).
Study monitors
Caroline Tournegros, Nadira Kaddour, Boris Berthe, Kaouttar Mellouk, Sophie Letrou, Igor Théodose, Julien Fournier, Véronique Deiler and Mireille Adda.
Rights and permissions
About this article
Cite this article
Reignier, J., Darmon, M., Sonneville, R. et al. Impact of early nutrition and feeding route on outcomes of mechanically ventilated patients with shock: a post hoc marginal structural model study. Intensive Care Med 41, 875–886 (2015). https://doi.org/10.1007/s00134-015-3730-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-015-3730-4