Abstract
Purpose
To clarify whether the gas exchange response to prone position is associated with lung recruitability in mechanically ventilated patients with acute respiratory failure.
Methods
In 32 patients, gas exchange response to prone position was investigated as a function of lung recruitability, measured by computed tomography in supine position.
Results
No relationship was found between increased oxygenation in prone position and lung recruitability. In contrast, the decrease of PaCO2 was related with lung recruitability (R 2 0.19; P = 0.01). Patients who decreased their PaCO2 more than the median value (−0.9 mmHg) had a greater lung recruitability (19 ± 16 vs. 8 ± 6%; P = 0.02), higher baseline PaCO2 (48 ± 8 vs. 41 ± 11 mmHg; P = 0.07), heavier lungs (1,968 ± 829 vs. 1,521 ± 342 g; P = 0.06) and more non-aerated tissue (1,009 ± 704 vs. 536 ± 188 g; P = 0.02) than those who did not.
Conclusions
During prone position, changes in PaCO2, but not in oxygenation, are associated with lung recruitability which, in turn, is associated with the severity of lung injury.
Similar content being viewed by others
Introduction
Prone position is currently used in the treatment of acute lung injury (ALI) and acute respiratory distress syndrome (ARDS) primarily as a rescue maneuver for severe hypoxemia, as it has been consistently shown to improve oxygenation compared to supine position [1, 2].
Apart from ameliorating gas exchange, prone position may decrease the danger associated with mechanical ventilation [3–6]. Indeed, reversing the vertical lung weight gradient is associated with an increase in normally inflated tissue in the dorsal regions (recruitment) and a variable decrease in aeration in the ventral ones (de-recruitment) [7]. If the net result is recruitment, then ventilation will become more uniform and inflation more homogeneously distributed, with a decrease in stress and strain, the first triggers of ventilator-induced lung (and distant organs) injury [4, 6, 8, 9]. Moreover, any gas exchange improvement occurring in prone position may reduce the need of using (potentially injurious) high fraction of inspired oxygen and ventilator support [10].
Although, so far, prone position has not been associated with any survival benefit [11, 12], despite positive trends [13, 14], we found that patients who significantly decrease their PaCO2 while prone have a higher survival rate compared to those who do not [15]. It is tempting to speculate that this outcome benefit depends on effective lung recruitment in prone position and that the decrease in PaCO2 suggests a decrease in physiological dead space possibly due to the ventilation of newly recruited and perfused pulmonary units.
Patients with ALI or ARDS have, however, highly variable lung recruitability, ranging from negligible values up to more than 50% of total lung parenchyma, which, in turn, is associated with the overall severity of lung injury [16]. We may then expect that patients with different lung recruitability display different gas exchange responses to prone position.
Therefore, we decided to investigate the relationship between gas exchange response to prone position and lung recruitability, hypothesizing that most of the changes occurring in prone position depend on the amount of tissue effectively recruited.
Materials and methods
At two University Hospitals, we retrospectively analyzed the data-sheets of adult, mechanically ventilated patients admitted to Intensive Care Unit with ALI or ARDS since January 2003, who underwent prone ventilation within 72 h from the assessment of lung recruitability by CT scan. Twenty-five of these patients were originally enrolled in another study, specifically aimed at investigating lung recruitability during acute respiratory failure [16].
ALI and ARDS were defined according to standard criteria: a ratio of arterial oxygen tension to fraction of inspired oxygen (PaO2:FiO2) of less than 300 (ALI) or 200 (ARDS) mmHg, the presence of bilateral infiltrates on the chest radiograph, and no clinical evidence of left atrial hypertension [17].
Demographic data, primary diagnosis, and severity of illness at admission (expressed as simplified acute physiology score, SAPS, II) were recorded. We reviewed gas exchange variables (PaO2:FiO2 and arterial carbon dioxide tension, PaCO2), minute ventilation, positive end-expiratory pressure (PEEP), respiratory system compliance (the ratio of tidal volume to the difference between inspiratory plateau pressure and PEEP) in supine position and after an average period of 4 h of prone position, while the ventilator setting was kept constant. Patients were classified as “PaO2 responders” if PaO2:FiO2 increased more than the median value observed in the entire group and as “PaCO2 responders” if PaCO2 decreased more than the corresponding median value.
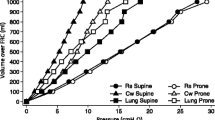
Whole lung CT scans obtained at 5 and 45 cm of water of airway pressure with the patient lying supine were analyzed as previously described [18]. Potential lung recruitability was defined as the difference in the amount of non-aerated lung tissue (density equal to or above −100 HU) at these two levels of airway pressure, expressed as the percentage of total lung weight. We also studied the regional recruitability of the ventral and dorsal halves of the lung, ideally separated by a transverse line crossing the vertical mid-point in each sectional image.
The local Ethics Committee was informed of the ongoing retrospective analysis and did not require any specific informed consent. Indeed, patients included in the present work were either part of other prospective studies in which informed consent had been already obtained or underwent prone position and assessment of lung recruitability by CT scan as part of routine clinical practice and not for research purposes.
Statistical analysis
Data are presented as mean ± standard deviation (range was also reported when appropriate). The association between continuous variables was analyzed using linear regression and expressed as R 2. When patients were categorized according to gas exchange response, differences between groups were investigated using Student t-test (in case of variables normally distributed), Mann–Whitney rank sum test (in case of variables that did not appear normally distributed on graphic inspection), or one way analysis of variance (ANOVA) with post hoc Bonferroni test, as appropriate. A P < 0.05 was considered as significant.
Results
Thirty-two patients were identified (Table 1). On average, lung recruitability was assessed by CT scan within 30 ± 20 h from the evaluation of the response to prone position (range 4–72 h) (Fig. 1). The lung CT scan preceded prone ventilation in 24 patients and followed it in 8 cases. Gas exchange was evaluated in supine position, 1 ± 1 (1–5) h before turning the patient prone, and in prone position, after 4 ± 3 (1–13) h of prone ventilation. Patients were identically ventilated in supine and prone position, in a volume-controlled (n = 15) or pressure-controlled (n = 17) modality. Tidal volume (528 ± 96 vs. 529 ± 116 mL, P = 0.93), respiratory rate (17 ± 6 vs. 17 ± 6, P = 0.33) and minute ventilation (8.7 ± 2.5 vs. 8.6 ± 2.6 L/min, P = 0.80) did not significantly differ between supine and prone position.
Upper panel representative CT images of the lung obtained at 5 (left) and 45 (right) cm of water of airway pressure from a patient with low lung recruitability. Total lung weight at 5 cm of water was 1,508 g and that of non-aerated tissue 372 g. The percentage of recruitable lung was 1% of total lung weight. Lower panel representative CT images of the lung obtained at 5 (left) and 45 (right) cm of water of airway pressure from a patient with high lung recruitability. Total lung weight at 5 cm of water was 2,123 g and that of non-aerated tissue 1,341 g. The percentage of recruitable lung was 59% of total lung weight
Considering the entire study population, prone ventilation was associated with a PaO2:FiO2 increase of 52 ± 59 mmHg (P < 0.001) and a PaCO2 decrease of 2 ± 6 mmHg (P = 0.07) relative to supine position. Nonetheless, the observed changes in PaCO2 and PaO2:FiO2 were clearly not associated (R 2 0.04; P = 0.26).
We could not find any relationship between the percentage of potentially recruitable lung and the changes of PaO2:FiO2 to prone ventilation (R 2 0.01; P = 0.57, Fig. 2, upper panel). This finding was replicated when the analysis was restricted to the patients who had their lung CT scan performed within 24 h from the evaluation of the response to prone position (n = 15, R 2 0.02, P = 0.57) and to those kept prone longer than 4 h (n = 13, R 2 0.0, P = 0.96). In contrast, lung recruitability was inversely associated with the change in PaCO2 that is, the larger the lung recruitability the lower the PaCO2 in prone compared to supine position (R 2 0.19; P = 0.01, Fig. 2, lower panel). This signal was particularly evident in the patients treated in pressure control ventilation (17 patients). In these subjects the possible increase in lung compliance related to the greater recruitment led to an increase of total ventilation, which, in turn, resulted in decreased PaCO2 (R 2 = 0.76, P = 0.0045). In contrast, in patients treated in volume control ventilation the greater recruitment cannot lead to an increase of total ventilation. Indeed the possible PaCO2 decrease in these subjects may be only due to a decrease of alveolar dead space (see Fig. 2 for further details).
Upper panel association between the response in PaO2:FiO2 to prone ventilation and the percentage of potentially recruitable lung (R 2 0.01; P = 0.57). Triangles indicate patients treated with pressure control ventilation, circles indicate patients treated with volume control ventilation. Lower panel association between the response in PaCO2 to prone ventilation and the percentage of potentially recruitable lung (R 2 0.19; P = 0.01). Triangles indicate patients treated with pressure control ventilation, circles indicate patients treated with volume control ventilation. According to this stratification the relationships obtained are: Patients in volume control: PaCO2 change = −1.14 − 0.16 × potentially recruitable lung (R 2 = 0.05; P = 0.44); Patients in pressure control: PaCO2 change = 2.99 − 0.27 × potentially recruitable lung (R 2 = 0.31; P = 0.02)
According to median values, patients were defined as “PaO2 responders” when PaO2:FiO2 increased at least 40 mmHg and as “PaCO2 responders” if PaCO2 decreased at least 0.9 mmHg in prone compared to supine position. PaO2 responders and non-responders did not differ in any of the physiological baseline values and any of the CT scan-derived variables (Table 2). In contrast, PaCO2 responders appeared more severely ill than PaCO2 non-responders. In fact, the bulk of baseline physiological variables (PaO2:FiO2, PaCO2, compliance of the respiratory system) were worse, although not significantly, in patients who decreased their PaCO2 while prone, compared to those who did not. In line with these findings, the quantitative analysis of CT scans revealed a significantly higher lung weight (that is, much more oedema), greater amount of non-aerated tissue and increased lung recruitability in PaCO2 responders than non-responders (Table 2).
The main results from the regional analysis of CT scans are shown in Table 2. In PaCO2 responders, the lung weight, the non-aerated tissue as well as the lung recruitability were significantly greater in the dorsal and ventral regions compared to PaCO2 non-responders. The ratio between non-aerated tissue in the upper and lower halves of the lung, however, was not different in PaCO2 responders and non-responders (0.89 ± 0.63 vs. 0.68 ± 0.39; P = 0.30), suggesting a similar distribution of lung injury.
Discussion
The primary findings of this study are that oxygen and carbon dioxide responses to prone position are independent and, more important, that the PaCO2 decrease, rather than the PaO2:FiO2 increase, is significantly associated with lung recruitability (R 2 0.19; P = 0.01).
Although the beneficial effect of prone position on oxygenation has been widely reported [1, 2] and has been further confirmed in the present study, with 30 out of 32 patients actually improving their PaO2:FiO2, the underlying mechanism(s) still remains unidentified. Most of the difficulties arise from our inability to simultaneously measure regional blood flow and ventilation in patients with ALI or ARDS. Indeed, while we can quite easily measure the “gas side” of the determinants of PaO2, the blood counterpart usually remains undetermined. Even so, however, there is no doubt that PaO2 can increase independently of lung recruitment [19]. This does not mean that recruitment does not produce any improvement in oxygenation, but rather implies that changes of global cardiac output and/or its distribution between non-aerated and aerated lung regions can lead to a rise in PaO2 even in the absence of lung recruitment. This is likely the reason why inhaled nitric oxide ameliorates oxygenation [20]. Accordingly, in this study, the response in oxygenation to prone position was not associated with lung recruitability, as quantified by CT scan. Others have also suggested that the pattern of lung disease measured by CT scan with the patient lying supine cannot predict the response in oxygenation to prone position [21].
In contrast, the response in PaCO2 to prone position, with an unchanged ventilator setting, did correlate, in a weak but statistically significant way, with lung recruitability, which was in turn associated with signs of more severe lung injury. We hypothesize that a greater lung recruitability in supine position resulted in a greater net recruitment in prone position, with a parallel increase in ventilated and perfused lung units (that is a decrease in alveolar dead space). Although PaO2 may change independently from recruitment, it is interesting to note that the increase in oxygenation was greater, although not significantly, in PaCO2 responders. Furthermore, the seven patients who simultaneously improved their PaO2:FiO2 and PaCO2 while prone had significantly higher lung recruitability (24 ± 18%) than those who only increased their oxygenation or decreased their PaCO2 (12 ± 10%, n = 17; P = 0.05), or did not respond at all to prone position (7 ± 6%, n = 8; P = 0.01).
At a first glance, our results may seem to contradict previous findings from Galiatsou and colleagues, who performed quantitative analysis of lung CT scans taken in supine and prone position in 21 patients with ALI or ARDS [22]. In that study, patients with “lobar” lung injury (so defined according to morphological criteria) almost halved their percentage of non-aerated tissue, significantly decreased their PaCO2 and markedly improved their oxygenation when turned prone. In contrast, in “diffuse” lung injury, also defined according to lung morphology, the decrease in non-aerated tissue (recruitment) was minor; PaCO2 did not decrease whereas oxygenation improved. Nonetheless, if we consider the quantitative CT scan analysis, it becomes evident that patients with “lobar” ALI or ARDS (who had the most striking response to prone position) had a significantly higher amount of non-aerated tissue and lung recruitability than those with “diffuse” lung injury. Accordingly, PaCO2 decreased only in the most severely ill and recruitable patients while oxygenation increased independently of the extent of lung recruitment, a finding that seems to be in line with our current results.
The regional analysis we performed showed that the non-aerated tissue is distributed in equal proportion in ventral and dorsal regions, independently of the change in PaCO2 observed in prone position. The main difference between PaCO2 responders and non-responders is in the absolute amount of non-aerated tissue, i.e., the overall severity of lung injury. This finding is consistent with the following (sponge) model: the oedema is quite homogeneously distributed all over the lung; it increases the lung weight and squeezes the gas out of the dependent lung regions, thus producing alveolar collapse and increasing the CT densities in dependent regions [23, 24]. The greater the oedema (lung weight) the greater the collapse (recruitability) [16]. In prone position, patients with the greatest collapse have the greatest potential for recruiting large portions of previously non-aerated tissue, thus improving alveolar ventilation and decreasing their PaCO2. Our actual results are further corroborated by those from Galiatsou and collegues [22].
Several trials have investigated the impact of prone position on outcome of patients with ALI or ARDS [11–13]. They have consistently shown that prone position does not decrease mortality when randomly applied, but have also suggested that the subgroup of patients with more severe lung injury may still experience a significant benefit. We believe that in these patients prone positioning is associated with net recruitment. This, in turn, may reduce the injurious effects of mechanical ventilation on lungs and distant organs, allowing to modify the ventilator setting towards safer limits or reducing the regional lung stress and strain for a given ventilation [25]. Indeed, the patients with the higher lung injury severity/greater lung recruitability, should be the ones who are benefited more by prone position. Actually in a post hoc analysis of a randomized study on prone position [15] we found that in the prone position group the patients who decreased their PaCO2 (likely the greater lung recruiters) did survive significantly more than the patients who did not modify their PaCO2 (likely the low lung recruiters). However, these findings seem to be in contrast with another study [16] where we found that patients with greater lung recruitability have lower survival rate than patients with lower lung recruitability (all patients were treated in supine position). To reconcile these two findings the only rational explanation is that the prone position may be harmful to patients with moderate lung injury and low lung recruitability, due, as an example, to a redistribution of infection throughout the bronchial tree [26]. If this is the case, prone position should be indicated only in patients with high lung recruitability. Ongoing studies on prone position should help to clarify this issue. Our study has several limitations. It is retrospective and in some cases quite a long time (up to 3 days) passed between the CT scanning and the evaluation of the response to prone position. Moreover, the study was not standardized and lung CT scan was obtained either before or after a period of prone ventilation. In order to reduce any bias, gas exchange response and CT scan analysis were performed by two independent groups of investigators, unaware of each other’s findings. Another limitation of our study is that no CT scan was obtained with the patient lying prone and lung perfusion was not investigated at all.
Even so, we believe that our results may help the clinician in appropriately selecting those patients who may get the best out of prone positioning: those more severely ill and with high lung recruitability. Although the quantitative analysis of lung CT scans taken at 5 and 45 cm of water of airway pressure is currently the only way to measure lung recruitability, the subjective evaluation of the lung density redistribution on the two CT scans or the computation of the weight of total and non-aerated lung tissue at 5 cm of water appear as acceptable surrogates, as these variables have been shown to strongly correlate with the potential for lung recruitability [16].
References
Abroug F, Ouanes-Besbes L, Elatrous S, Brochard L (2008) The effect of prone positioning in acute respiratory distress syndrome or acute lung injury: a meta-analysis. Areas of uncertainty and recommendations for research. Intensive Care Med 34:1002–1011
Sud S, Sud M, Friedrich JO, Adhikari NK (2008) Effect of mechanical ventilation in the prone position on clinical outcomes in patients with acute hypoxemic respiratory failure: a systematic review and meta-analysis. CMAJ 178:1153–1161
Broccard A, Shapiro RS, Schmitz LL, Adams AB, Nahum A, Marini JJ (2000) Prone positioning attenuates and redistributes ventilator-induced lung injury in dogs. Crit Care Med 28:295–303
Mentzelopoulos SD, Roussos C, Zakynthinos SG (2005) Prone position reduces lung stress and strain in severe acute respiratory distress syndrome. Eur Respir J 25:534–544
Nakos G, Batistatou A, Galiatsou E, Konstanti E, Koulouras V, Kanavaros P, Doulis A, Kitsakos A, Karachaliou A, Lekka ME, Bai M (2006) Lung and ‘end organ’ injury due to mechanical ventilation in animals: comparison between the prone and supine positions. Crit Care 10:R38
Valenza F, Guglielmi M, Maffioletti M, Tedesco C, Maccagni P, Fossali T, Aletti G, Porro GA, Irace M, Carlesso E, Carboni N, Lazzerini M, Gattinoni L (2005) Prone position delays the progression of ventilator-induced lung injury in rats: does lung strain distribution play a role? Crit Care Med 33:361–367
Gattinoni L, Pelosi P, Vitale G, Pesenti A, D’Andrea L, Mascheroni D (1991) Body position changes redistribute lung computed-tomographic density in patients with acute respiratory failure. Anesthesiology 74:15–23
Gattinoni L, Carlesso E, Cadringher P, Valenza F, Vagginelli F, Chiumello D (2003) Physical and biological triggers of ventilator-induced lung injury and its prevention. Eur Respir J Suppl 47:15s–25s
Haitsma JJ, Lachmann B (2006) Lung protective ventilation in ARDS: the open lung maneuver. Minerva Anestesiol 72:117–132
Tremblay LN, Slutsky AS (2006) Ventilator-induced lung injury: from the bench to the bedside. Intensive Care Med 32:24–33
Gattinoni L, Tognoni G, Pesenti A, Taccone P, Mascheroni D, Labarta V, Malacrida R, Di Giulio P, Fumagalli R, Pelosi P, Brazzi L, Latini R, Prone-Supine Study Group (2001) Effect of prone positioning on the survival of patients with acute respiratory failure. N Engl J Med 345:568–573
Guerin C, Gaillard S, Lemasson S, Ayzac L, Girard R, Beuret P, Palmier B, Le QV, Sirodot M, Rosselli S, Cadiergue V, Sainty JM, Barbe P, Combourieu E, Debatty D, Rouffineau J, Ezingeard E, Millet O, Guelon D, Rodriguez L, Martin O, Renault A, Sibille JP, Kaidomar M (2004) Effects of systematic prone positioning in hypoxemic acute respiratory failure: a randomized controlled trial. JAMA 292:2379–2387
Mancebo J, Fernandez R, Blanch L, Rialp G, Gordo F, Ferrer M, Rodríguez F, Garro P, Ricart P, Vallverdú I, Gich I, Castaño J, Saura P, Domínguez G, Bonet A, Albert RK (2006) A multicenter trial of prolonged prone ventilation in severe acute respiratory distress syndrome. Am J Respir Crit Care Med 173:1233–1239
Fernandez R, Trenchs X, Klamburg J, Castedo J, Serrano JM, Besso G, Tirapu JP, Santos A, Mas A, Parraga M, Jubert P, Frutos F, Añon JM, Garcia M, Rodriguez F, Yebenes JC, Lopez MJ (2008) Prone positioning in acute respiratory distress syndrome: a multicenter randomized clinical trial. Intensive Care Med 34:1487–1491
Gattinoni L, Vagginelli F, Carlesso E, Taccone P, Conte V, Chiumello D, Valenza F, Caironi P, Pesenti A, Prone-Supine Study Group (2003) Decrease in PaCO2 with prone position is predictive of improved outcome in acute respiratory distress syndrome. Crit Care Med 31:2727–2733
Gattinoni L, Caironi P, Cressoni M, Chiumello D, Ranieri VM, Quintel M, Russo S, Patroniti N, Cornejo R, Bugedo G (2006) Lung recruitment in patients with the acute respiratory distress syndrome. N Engl J Med 354:1775–1786
Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, Lamy M, LeGall JR, Morris A, Spragg R (1994) Report of the American–European consensus conference on ARDS: definitions, mechanisms, relevant outcomes and clinical trial coordination The Consensus Committee. Intensive Care Med 20:225–232
Gattinoni L, Caironi P, Pelosi P, Goodman LR (2001) What has computed tomography taught us about the acute respiratory distress syndrome? Am J Respir Crit Care Med 164:1701–1711
Dantzker DR, Lynch JP, Weg JG (1980) Depression of cardiac output is a mechanism of shunt reduction in the therapy of acute respiratory failure. Chest 77:636–642
Hopkins SR, Johnson EC, Richardson RS, Wagner H, De Rosa M, Wagner PD (1997) Effects of inhaled nitric oxide on gas exchange in lungs with shunt or poorly ventilated areas. Am J Respir Crit Care Med 156:484–491
Papazian L, Paladini MH, Bregeon F, Thirion X, Durieux O, Gainnier M, Huiart L, Agostini S, Auffray JP (2002) Can the tomographic aspect characteristics of patients presenting with acute respiratory distress syndrome predict improvement in oxygenation-related response to the prone position? Anesthesiology 97:599–607
Galiatsou E, Kostanti E, Svarna E, Kitsakos A, Koulouras V, Efremidis SC, Nakos G (2006) Prone position augments recruitment and prevents alveolar overinflation in acute lung injury. Am J Respir Crit Care Med 174:187–197
Pelosi P, D’Andrea L, Vitale G, Pesenti A, Gattinoni L (1994) Vertical gradient of regional lung inflation in adult respiratory distress syndrome. Am J Respir Crit Care Med 149:8–13
Gattinoni L, D’Andrea L, Pelosi P, Vitale G, Pesenti A, Fumagalli R (1993) Regional effects and mechanism of positive end-expiratory pressure in early adult respiratory distress syndrome. JAMA 269:2122–2127
Gattinoni L, Protti A (2008) Ventilation in the prone position: for some but not for all? CMAJ 178:1174–1176
Marini JJ, Gattinoni L (2008) Propagation prevention: a complementary mechanism for “lung protective” ventilation in acute respiratory distress syndrome. Crit Care Med 36:3252–3258
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Protti, A., Chiumello, D., Cressoni, M. et al. Relationship between gas exchange response to prone position and lung recruitability during acute respiratory failure. Intensive Care Med 35, 1011–1017 (2009). https://doi.org/10.1007/s00134-009-1411-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-009-1411-x