Abstract
Background
Emergency medical care for critically ill nontrauma patients (CINT) varies between different emergency departments (ED) and healthcare systems, while resuscitation of trauma patients is always performed within the ED. In many ED CINT are treated and stabilized while in many German smaller hospitals CINT are transferred directly to the intensive care unit (ICU) without performing critical care measures in the ED. Little is known about the resuscitation room management of CINT regarding patient characteristics and outcome although bigger hospitals perform ED resuscitation of CINT in routine care. Against this background we conducted this retrospective analysis of CINT treated by an ED resuscitation room concept in a German 756 bed teaching hospital.
Methods
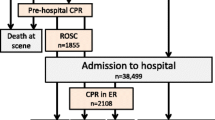
The collective of CINT treated within the ED resuscitation room (1 October 2018 to 31 March 2019) was analyzed after ethical approval. After each resuscitation room operation, the team leader filled out a standardized paper-based questionnaire and qualified the patient as a resuscitation room patient this way. Only patients who underwent invasive procedures and were admitted to ICU or died in the ED were included. Patient characteristics, performed critical care measures, short-term outcomes and the comparison of admission characteristics between survivors and non-survivors were evaluated. Additionally, the accordance of ED admission diagnoses and discharge diagnoses were analyzed.
Results
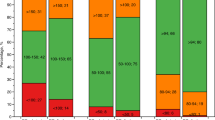
Overall, 243 of 19,854 ED patients (1.22%) were treated in the resuscitation room. After exclusion of trauma patients, 193 (0.97%) CINT were included. Overall mortality was 29% (n = 56), 24‑h mortality was 13% (n = 25). Patient characteristics (vital signs, blood gas analysis) differed significantly between survivors and nonsurvivors except for respiratory rate and pain scale. An excerpt of conducted resuscitation room measures was as follows: arterial line n = 78 (40%); noninvasive ventilation n = 60 (31%); endotracheal intubation n = 56 (29%); cardiopulmonary resuscitation n = 19 (10%), central venous line n = 8 (4%). The number of conducted measures differed between survivors and nonsurvivors (median and interquartile range, IQR): 4 (IQR 2) vs. 4 (IQR 3) p = 0.0453. The length of ED stay was 148.2 ± 202.7 min until the patient was admitted to an ICU or died within the ED. ED admission diagnoses matched with hospital discharge diagnoses in 78%.
Conclusion
The observed mortality was high and was comparable to patient collectives with septic shock. Nonsurvivors showed significantly more impaired vital parameters and blood gas analysis parameters. Vital parameters together with blood gas analysis might enable ED risk stratification of CINT. Resuscitation room management enables immediate stabilization and diagnostic work-up of CINT even when no ICU bed is available. Furthermore, optimal allocation to specialized ICUs can probably be enabled more accurately after a first diagnostic work-up; however, although a first diagnostic work-up including laboratory tests and computed tomography in many cases was performed, ED admission and hospital discharge diagnoses matched only in 78%.
Zusammenfassung
Einleitung
Die Notfallversorgung für kritische Kranke ist in verschiedenen Gesundheitssystemen heterogen organisiert. Während Traumapatienten immer im Schockraum übergeben und stabilisiert werden, erfolgt speziell in der deutschen Grund- und Regelversorgung bei kritisch kranken Nicht-Traumapatienten häufig eine direkte Aufnahme auf die Intensivstation durch den Rettungsdienst. In dieser retrospektiven Studie wurde daher die Schockraumversorgung nichttraumatologischer Patienten in einem 756-Betten-Lehrkrankenhaus analysiert.
Methode
Schockraumversorgungen kritisch Kranker (01.10.2018 bis 31.03.2019) wurden in Bezug auf Patientencharakteristika, durchgeführte Schockraummaßnahmen und Krankenhaussterblichkeit analysiert. Ferner sollten die Aufnahmecharakteristika zwischen Überlebenden und Nichtüberlebenden evaluiert werden. Aufnahme- und Entlassungsdiagnosen sollten vergleichend ausgewertet werden.
Ergebnisse
Es wurden 243/19.854 Patienten (1,22 %) im Untersuchungszeitraum als Schockraumpatienten behandelt. Nach Ausschluss von Traumapatienten konnten 193 (0,97 %) kritisch kranke nichttraumatologische Patienten eingeschlossen werden. Die Gesamtsterblichkeit lag bei 29 % (n = 56), die 24-h-Sterblichkeit bei 13 % (n = 25). Es wurden im Mittel 4,24 Schockraummaßnahmen (z. B. Intubation, Zentraler Venenkatheter) durchgeführt mit einer Versorgungsdauer in der Notaufnahme von 148 ± 203 min. Die Aufnahmeparameter von Überlebenden und Nichtüberlebenden unterschieden sich signifikant mit Ausnahme von Atemfrequenz und Schmerzskala. Durchgeführte Schockraummaßnahmen bei Überlebenden vs. Nichtüberlebenden: Median 4 (IQR 2) vs. 4 (IQR 3), p = 0,0453. Krankenhausaufnahme- und Entlassungsdiagnosen stimmten in 78 % der Fälle überein.
Schlussfolgerung
Bei insgesamt hoher Krankenhaussterblichkeit zeigten sich signifikant schlechtere Vital- und Blutgasanalyseparameter bei Aufnahme für das Subkollektiv der Nichtüberlebenden. Ein möglicher Score aus Vital- und Blutgaswerten könnte folglich eine zukünftige Risikostratifizierung für nichttraumatologische Schockraumpatienten ermöglichen. Die nichttraumatologische Schockraumversorgung ermöglicht eine sofortige notfallmedizinische Versorgung und genaue Patientenallokation zu spezialisierten Intensivstationen. Nichtsdestotrotz stimmten Krankenhausaufnahme- und Entlassungsdiagnosen in 78 % überein.


Similar content being viewed by others
References
Adler C, Paul C, Michels G et al (2019) One year experience with fast track algorithm in patients with refractory out-of-hospital cardiac arrest. Resuscitation 144:157–165. https://doi.org/10.1016/j.resuscitation.2019.07.035
Ali AB, Lefering R, Fortun Moral M, Belzunegui Otano T (2017) Epidemiological comparison between the Navarra Major Trauma Registry and the German Trauma Registry (TR-DGU®). Scand J Trauma Resusc Emerg Med 25:107. https://doi.org/10.1186/s13049-017-0453-2
ARISE Investigators, ANZICS Clinical Trials Group, Peake SL et al (2014) Goal-directed resuscitation for patients with early septic shock. N Engl J Med 371:1496–1506. https://doi.org/10.1056/NEJMoa1404380
Atamna A, Shiber S, Yassin M et al (2019) The accuracy of a diagnosis of pneumonia in the emergency department. Int J Infect Dis 89:62–65. https://doi.org/10.1016/j.ijid.2019.08.027
Bernhard M, Bax SN, Hartwig T et al (2019) Airway Management in the Emergency Department (The OcEAN-Study)—a prospective single centre observational cohort study. Scand J Trauma Resusc Emerg Med 27:20. https://doi.org/10.1186/s13049-019-0599-1
Bernhard M, Döll S, Hartwig T et al (2018) Resuscitation room management of critically ill nontraumatic patients in a German emergency department (OBSERvE-study). Eur J Emerg Med 25:e9. https://doi.org/10.1097/MEJ.0000000000000543
Brink A, Alsma J, Verdonschot RJCG et al (2019) Predicting mortality in patients with suspected sepsis at the Emergency Department; a retrospective cohort study comparing qSOFA, SIRS and National Early Warning Score. Plos One 14:e211133. https://doi.org/10.1371/journal.pone.0211133
Carbó M, Fresco L, Osorio G et al (2020) Predictors of mortality in emergency department patients with sepsis scored 2 or 3 on the Quick Sequential Organ Failure Assessment scale. Emerg Rev Soc Espanola Med Emerg 32:169–176
von Dg EEAME et al (2014) The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg. https://doi.org/10.1016/j.ijsu.2014.07.013
Galvagno SM, Nahmias JT, Young DA (2019) Advanced trauma life support® update 2019: management and applications for adults and special populations. Anesthesiol Clin 37:13–32. https://doi.org/10.1016/j.anclin.2018.09.009
Goto Y, Funada A, Maeda T et al (2019) Field termination-of-resuscitation rule for refractory out-of-hospital cardiac arrests in Japan. J Cardiol 73:240–246. https://doi.org/10.1016/j.jjcc.2018.12.002
Gregers E, Kjærgaard J, Lippert F et al (2018) Refractory out-of-hospital cardiac arrest with ongoing cardiopulmonary resuscitation at hospital arrival—survival and neurological outcome without extracorporeal cardiopulmonary resuscitation. Crit Care Lond Engl 22:242. https://doi.org/10.1186/s13054-018-2176-9
Hadaya J, Dobaria V, Aguayo E et al (2020) National trends in utilization and outcomes of extracorporeal support for in- and out-of-hospital cardiac arrest. Resuscitation. https://doi.org/10.1016/j.resuscitation.2020.02.034
Hilbert-Carius P, Wurmb T, Lier H et al (2017) Care for severely injured persons : update of the 2016 S3 guideline for the treatment of polytrauma and the severely injured. Anaesthesist 66:195–206. https://doi.org/10.1007/s00101-017-0265-9
Jiang J, Kang N, Li B et al (2020) Comparison of adverse events between video and direct laryngoscopes for tracheal intubations in emergency department and ICU patients‑a systematic review and meta-analysis. Scand J Trauma Resusc Emerg Med 28:10. https://doi.org/10.1186/s13049-020-0702-7
Keijzers G, Macdonald SP, Udy AA et al (2020) The Australasian resuscitation in sepsis evaluation: fluids or vasopressors in emergency department sepsis (ARISE FLUIDS), a multi-centre observational study describing current practice in Australia and new zealand. Emerg Med Australas. https://doi.org/10.1111/1742-6723.13469
Kramer A, Urban N, Döll S et al (2019) Early lactate dynamics in critically ill non-traumatic patients in a resuscitation room of a German emergency department (OBSERvE-lactate-study). J Emerg Med 56:135–144. https://doi.org/10.1016/j.jemermed.2018.10.033
Levin N, Horton D, Sanford M et al (2019) Failure of vital sign normalization is more strongly associated than single measures with mortality and outcomes. Am J Emerg Med. https://doi.org/10.1016/j.ajem.2019.12.024
Meidert AS, Dolch ME, Mühlbauer K et al (2020) Oscillometric versus invasive blood pressure measurement in patients with shock: a prospective observational study in the emergency department. J Clin Monit Comput. https://doi.org/10.1007/s10877-020-00482-2
Mouncey PR, Osborn TM, Power GS et al (2015) Trial of early, goal-directed resuscitation for septic shock. N Engl J Med 372:1301–1311. https://doi.org/10.1056/NEJMoa1500896
Navarro S, Montmany S, Rebasa P et al (2014) Impact of ATLS training on preventable and potentially preventable deaths. World J Surg 38:2273–2278. https://doi.org/10.1007/s00268-014-2587-y
Ospina-Tascón GA, Hernandez G, Alvarez I et al (2020) Effects of very early start of norepinephrine in patients with septic shock: a propensity score-based analysis. Crit Care 24:52. https://doi.org/10.1186/s13054-020-2756-3
Permpikul C, Tongyoo S, Viarasilpa T et al (2019) Early use of norepinephrine in septic shock resuscitation (CENSER). A randomized trial. Am J Respir Crit Care Med 199:1097–1105. https://doi.org/10.1164/rccm.201806-1034OC
ProCESS Investigators, Yealy DM, Kellum JA et al (2014) A randomized trial of protocol-based care for early septic shock. N Engl J Med 370:1683–1693. https://doi.org/10.1056/NEJMoa1401602
Schoeneberg C, Schilling M, Burggraf M et al (2014) Reduction in mortality in severely injured patients following the introduction of the “Treatment of patients with severe and multiple injuries” guideline of the German society of trauma surgery—a retrospective analysis of a level 1 trauma center (2010–2012). Injury 45:635–638. https://doi.org/10.1016/j.injury.2013.11.024
Sulser S, Ubmann D, Schlaepfer M et al (2016) C‑MAC videolaryngoscope compared with direct laryngoscopy for rapid sequence intubation in an emergency department: A randomised clinical trial. Eur J Anaesthesiol 33:943–948. https://doi.org/10.1097/EJA.0000000000000525
Swol J, Belohlávek J, Brodie D et al (2018) Extracorporeal life support in the emergency department: a narrative review for the emergency physician. Resuscitation 133:108–117. https://doi.org/10.1016/j.resuscitation.2018.10.014
Thelen S, Michael M, Ashmawy H et al (2019) Schockraummanagement bei traumatologischen Patienten. Anaesthesist 68:49–66. https://doi.org/10.1007/s00101-018-0523-5
Viglino D, L’her E, Maltais F et al (2020) Evaluation of a new respiratory monitoring tool “Early Warning ScoreO2” for patients admitted at the emergency department with dyspnea. Resuscitation 148:59–65. https://doi.org/10.1016/j.resuscitation.2020.01.004
Funding
The study was performed and funded solely by departmental resources.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
H. Haake reports personal fees from Berlin Chemie, Novartis, Bayer Chemie and Maquet all outside the submitted work. J.S. Kreß, M. Rüppel, J. vom Dahl and S. Bergrath declare that they have no competing interests.
Due to the process that only routine data were collected, and all data analyses were performed in a pseudonymized way, the ethics committee (University hospital Aachen, Germany) waived personal consent by patients or ED personnel (EK051/20).
Rights and permissions
About this article
Cite this article
Kreß, J.S., Rüppel, M., Haake, H. et al. Short-term outcome and characteristics of critical care for nontrauma patients in the emergency department. Anaesthesist 71, 30–37 (2022). https://doi.org/10.1007/s00101-021-00953-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00101-021-00953-4