Abstract
Background
The identification of risk factors for severe injury is crucial in trauma triage and trauma team activation (TTA) depends on a sufficient triage. The aim of this study was to determine whether or not elevated serum lactate levels and age are risk factors for severe injury in TTA due to trauma mechanism.
Methods
We conducted a retrospective cohort study in a single level one trauma center between September 2019 and May 2021 and analysed every TTA due to trauma mechanism. Primary endpoint of interest was the association of serum lactate as well as age with injury severity assessed by the injury severity score (ISS).
Results
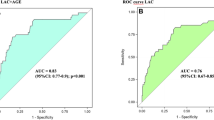
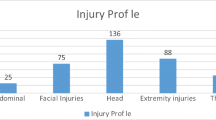
During the study period, we included 250 patients. Mean age was 43.3 years (Min.: 11, Max.: 90, SD: 18.7) and the initial lactate level was 1.7 mmol/L (SD: 0.95) with a mean ISS of 8.4 (SD: 8.99). The adjusted odds ratio (OR) for age > 65 being associated with an ISS > 16 is 9.7 (p < 0.001; 95% CI 4.01–25.58) and for lactate > 2.2 mmol/L being associated with an ISS > 16 is 6.29 (p < 0.001; 95% CI 2.93–13.48). A lactate level of > 4 mmol/L results in a 36-fold higher risk of severe injury with an ISS > 16 (OR 36.06; 95% CI 4–324.29).
Conclusion
This study identifies age (> 65) and lactate (> 2.2 mmol/L) as independent risk factors for severe injury in a TTA due to trauma mechanism. Existing triage protocols might benefit from congruous amendments.

Similar content being viewed by others
Availability of data and materials
The dataset generated and analyzed during the current study is not publicly accessible but is available from the corresponding author on reasonable request.
Code availability
Not applicable.
References
Van Rein EAJ, Houwert RM, Gunning AC, Lichtveld RA, Leenen LPH, Van Heijl M. Accuracy of prehospital triage protocols in selecting severely injured patients: a systematic review. J Trauma Acute Care Surg. 2017;83:328–39. https://doi.org/10.1097/TA.0000000000001516.
Rotondo M, Cribari C, Smith R. Resources for optimal care of the traumatised patient. 6th ed. Chicago: American College of Surgeons; 2014.
Polites SF, Leonard JM, Glasgow AE, Zielinski MD, Jenkins DH, Habermann EB. Undertriage after severe injury among United States trauma centers and the impact on mortality. Am J Surg. 2018;216:813–8. https://doi.org/10.1016/j.amjsurg.2018.07.061.
Holst JA, Perman SM, Capp R, Haukoos JS, Ginde AA. Undertriage of trauma-related deaths in U.S. emergency departments. West J Emerg Med. 2016;17:315–23. https://doi.org/10.5811/westjem.2016.2.29327.
Newgard CD, Staudenmayer K, Hsia RY, Mann NC, Bulger EM, Holmes JF, et al. The cost of overtriage: more than one-third of low-risk injured patients were taken to major trauma centers. Health Aff (Millwood). 2013;32:1591–9. https://doi.org/10.1377/hlthaff.2012.1142.
Faul M, Wald MM, Sullivent EE, Sasser SM, Kapil V, Lerner EB, et al. Large cost savings realized from the 2006 Field Triage Guideline: reduction in overtriage in U.S. trauma centers. Prehosp Emerg Care. 2012;16:222–9. https://doi.org/10.3109/10903127.2011.615013.
Ochsner MG, Schmidt JA, Rozycki GS, Champion HR. The evaluation of a two-tier trauma response system at a major trauma center: is it cost effective and safe? J Trauma. 1995;39:971–7. https://doi.org/10.1097/00005373-199511000-00025.
Rehn M, Lossius HM, Tjosevik KE, Vetrhus M, OstebaO O, Eken T. Efficacy of a two-tiered trauma team activation protocol in a Norwegian trauma centre. Br J Surg. 2012;99:199–208. https://doi.org/10.1002/bjs.7794.
Jenkins P, Rogers J, Kehoe A, Smith JE. An evaluation of the use of a two-tiered trauma team activation system in a UK major trauma centre. Emerg Med J. 2015;32:364–7. https://doi.org/10.1136/emermed-2013-203402.
Linder F, Holmberg L, Bjorck M, Juhlin C, Thorbjornsen K, Wisinger J, et al. A prospective stepped wedge cohort evaluation of the new national trauma team activation criteria in Sweden - The TRAUMALERT study. Scand J Trauma Resusc Emerg Med. 2019;27:1–10. https://doi.org/10.1186/s13049-019-0619-1.
Davis T, Dinh M, Roncal S, Byrne C, Petchell J, Leonard E, et al. Prospective evaluation of a two-tiered trauma activation protocol in an Australian major trauma referral hospital. Injury. 2010;41:470–4. https://doi.org/10.1016/j.injury.2010.01.003.
Voskens FJ, Van Rein EAJ, Van Der Sluijs R, Houwert RM, Lichtveld RA, Verleisdonk EJ, et al. Accuracy of prehospital triage in selecting severely injured trauma patients. JAMA Surg. 2018;153:322–7. https://doi.org/10.1001/jamasurg.2017.4472.
Jagan N, Morrow LE, Walters RW, Plambeck RW, Patel TM, Moore DR, et al. Sympathetic stimulation increases serum lactate concentrations in patients admitted with sepsis: implications for resuscitation strategies. Ann Intensive Care. 2021;11:24. https://doi.org/10.1186/s13613-021-00805-9.
Kushimoto S, Akaishi S, Sato T, Nomura R, Fujita M, Kudo D, et al. Lactate, a useful marker for disease mortality and severity but an unreliable marker of tissue hypoxia/hypoperfusion in critically ill patients. Acute Med Surg. 2016;3:293–7. https://doi.org/10.1002/ams2.207.
Baxter J, Cranfield KR, Clark G, Harris T, Bloom B, Gray AJ. Do lactate levels in the emergency department predict outcome in adult trauma patients? A systematic review. J Trauma Acute Care Surg. 2016;81:555–66. https://doi.org/10.1097/TA.0000000000001156.
Vandromme MJ, Griffin RL, Weinberg JA, Rue LW 3rd, Kerby JD. Lactate is a better predictor than systolic blood pressure for determining blood requirement and mortality: could prehospital measures improve trauma triage? J Am Coll Surg. 2010;210:861–867,867–869. https://doi.org/10.1016/j.jamcollsurg.2010.01.012.
Guyette FX, Meier EN, Newgard C, McKnight B, Daya M, Bulger EM, et al. A comparison of prehospital lactate and systolic blood pressure for predicting the need for resuscitative care in trauma transported by ground. J Trauma Acute Care Surg. 2015;78:600–6. https://doi.org/10.1097/TA.0000000000000549.
Oh TK, Song I-A, Bae H-J, Jeon Y-T. Serum lactate level upon admission to the neuro-intensive care unit and 90-day mortality: a retrospective study. J Clin Neurosci. 2019;70:173–7. https://doi.org/10.1016/j.jocn.2019.08.029.
Richards JE, Mazzeffi MA, Massey MS, Rock P, Galvagno SM, Scalea TM. The bitter and the sweet: relationship of lactate, glucose, and mortality after severe blunt trauma. Anesth Analg. 2020. https://doi.org/10.1213/ane.0000000000005335.
Raa A, Sunde GA, Bolann B, Kvåle R, Bjerkvig C, Eliassen HS, et al. Validation of a point-of-care capillary lactate measuring device (Lactate Pro 2). Scand J Trauma Resusc Emerg Med. 2020;28:83. https://doi.org/10.1186/s13049-020-00776-z.
Wilson MS, Konda SR, Seymour RB, Karunakar MA. Early predictors of mortality in geriatric patients with trauma. J Orthop Trauma. 2016;30:e299-304. https://doi.org/10.1097/BOT.0000000000000615.
Hashmi A, Ibrahim-Zada I, Rhee P, Aziz H, Fain MJ, Friese RS, et al. Predictors of mortality in geriatric trauma patients: a systematic review and meta-analysis. J Trauma Acute Care Surg. 2014;76:894–901. https://doi.org/10.1097/TA.0b013e3182ab0763.
Kodadek LM, Selvarajah S, Velopulos CG, Haut ER, Haider AH. Undertriage of older trauma patients: is this a national phenomenon? J Surg Res. 2015;199:220–9. https://doi.org/10.1016/j.jss.2015.05.017.
Uribe-Leitz T, Jarman MP, Sturgeon DJ, Harlow AF, Lipsitz SR, Cooper Z, et al. National study of triage and access to trauma centers for older adults. Ann Emerg Med. 2020;75:125–35. https://doi.org/10.1016/j.annemergmed.2019.06.018.
Bertil Bouillon, Pieper D. S3-Leitlinie Polytrauma/Schwerverletzten-Behandlung. AWMF Regist. 2016.
Bolorunduro OB, Villegas C, Oyetunji TA, Haut ER, Stevens KA, Chang DC, et al. Validating the injury severity score (ISS) in different populations: ISS predicts mortality better among hispanics and females. J Surg Res. 2011;166:40–4. https://doi.org/10.1016/j.jss.2010.04.012.
Abouleish AE, Leib ML, Cohen NH. ASA provides examples to each ASA physical status class. ASA Newsl. 2015;79:38–49.
Hurwitz EE, Simon M, Vinta SR, Zehm CF, Shabot SM, Minhajuddin A, et al. Adding examples to the ASA-physical status classification improves correct assignment to patients. Anesthesiology. 2017;126:614–22. https://doi.org/10.1097/ALN.0000000000001541.
Andersen LW, Mackenhauer J, Roberts JC, Berg KM, Cocchi MN, Donnino MW. Etiology and therapeutic approach to elevated lactate Lars. Mayo Clin Proc. 2013;88:1127–40. https://doi.org/10.1016/j.mayocp.2013.06.012.
Brown JB, Lerner EB, Sperry JL, Billiar TR, Peitzman AB, Guyette FX. Prehospital lactate improves accuracy of prehospital criteria for designating trauma activation level. J Trauma Acute Care Surg. 2016;81:445–52. https://doi.org/10.1097/TA.0000000000001085.
St John AE, McCoy AM, Moyes AG, Guyette FX, Bulger EM, Sayre MR. Prehospital lactate predicts need for resuscitative care in non-hypotensive trauma patients. West J Emerg Med. 2018;19:224–31. https://doi.org/10.5811/westjem.2017.10.34674.
Demidenko E. Sample size and optimal design for logistic regression with binary interaction. Stat Med. 2008;27:36–46. https://doi.org/10.1002/sim.2980.
Schoeneberg C, Schilling M, Keitel J, Kauther MD, Burggraf M, Hussmann B, et al. TraumaNetwork, Trauma Registry of the DGU®, Whitebook, S3 guideline on treatment of polytrauma/severe injuries—an approach for validation by a retrospective analysis of 2304 patients (2002–2011) of a Level 1 Trauma Centre TT—Traumanetzwerk, TraumaReg. Zentralbl Chir. 2017;142:199–208. https://doi.org/10.1055/s-0033-1360225.
Marzi I, Lustenberger T, Störmann P, Mörs K, Wagner N, Wutzler S. Steigender Vorhalteaufwand für den SchockraumIncreasing overhead ressources of the trauma room. Unfallchirurg. 2019;122:53–8. https://doi.org/10.1007/s00113-018-0484-9.
Hagebusch P, Faul P, Naujoks F, Klug A, Hoffmann R, Schweigkofler U. Trauma-team-activation in Germany: how do emergency service professionals use the activation due to trauma mechanism? Results from a nationwide survey. Eur J Trauma Emerg Surg. 2020. https://doi.org/10.1007/s00068-020-01425-x.
Fröhlich M, Caspers M, Lefering R, Driessen A, Bouillon B, Maegele M, et al. Do elderly trauma patients receive the required treatment? Epidemiology and outcome of geriatric trauma patients treated at different levels of trauma care. Eur J Trauma Emerg Surg. 2020;46:1463–9. https://doi.org/10.1007/s00068-019-01285-0.
Bardes JM, Benjamin E, Schellenberg M, Inaba K, Demetriades D. Old age with a traumatic mechanism of injury should be a trauma team activation criterion. J Emerg Med. 2019;57:151–5. https://doi.org/10.1016/j.jemermed.2019.04.003.
Demetriades D, Sava J, Alo K, Newton E, Velmahos GC, Murray JA, et al. Old age as a criterion for trauma team activation. J Trauma Inj Infect Crit Care. 2001;51:754–6. https://doi.org/10.1097/00005373-200110000-00022.
Caterino JM, Brown NV, Hamilton MW, Ichwan B, Khaliqdina S, Evans DC, et al. Effect of geriatric-specific trauma triage criteria on outcomes in injured older adults: a statewide retrospective cohort study. J Am Geriatr Soc. 2016;64:1944–51. https://doi.org/10.1111/jgs.14376.
Fernandez FB, Ong A, Martin AP, Schwab CW, Wasser T, Butts CA, et al. Success of an expedited emergency department triage evaluation system for geriatric trauma patients not meeting trauma activation criteria. Emerg Med. 2019;11:241–7. https://doi.org/10.2147/OAEM.S212617.
Baron BJ, Nguyen A, Stefanov D, Shetty A, Zehtabchi S. Clinical value of triage lactate in risk stratifying trauma patients using interval likelihood ratios. Am J Emerg Med. 2018;36:784–8. https://doi.org/10.1016/j.ajem.2017.10.015.
Wentling J, Krall SP, McNierney A, Dewey K, Richman PB, Blow O. Predictive value of point-of-care lactate measurement in patients meeting level II and III trauma team activation criteria that present to the emergency department: a prospective study. J Emerg Trauma Shock. 2019;12:203–8. https://doi.org/10.4103/JETS.JETS_120_18.
Martín-Rodríguez F, López-Izquierdo R, Castro Villamor MA, Mangas IM, Del Brío IP, Delgado Benito JF, et al. Prognostic value of lactate in prehospital care as a predictor of early mortality. Am J Emerg Med. 2019;37:1627–32. https://doi.org/10.1016/j.ajem.2018.11.028.
Davis JW, Dirks RC, Kaups KL, Tran P. Base deficit is superior to lactate in trauma. Am J Surg. 2018;215:682–5. https://doi.org/10.1016/j.amjsurg.2018.01.025.
Davis JW, Sue LP, Dirks RC, Kaups KL, Kwok AM, Wolfe MM, et al. Admission base deficit is superior to lactate in identifying shock and resuscitative needs in trauma patients. Am J Surg. 2020;220:1480–4. https://doi.org/10.1016/j.amjsurg.2020.10.005.
Gale SC, Kocik JF, Creath R, Crystal JS, Dombrovskiy VY. A comparison of initial lactate and initial base deficit as predictors of mortality after severe blunt trauma. J Surg Res. 2016;205:446–55. https://doi.org/10.1016/j.jss.2016.06.103.
Raux M, Le Manach Y, Gauss T, Baumgarten R, Hamada S, Harrois A, et al. Comparison of the prognostic significance of initial blood lactate and base deficit in trauma patients. Anesthesiology. 2017;126:522–33. https://doi.org/10.1097/ALN.0000000000001490.
Ter Avest E, Griggs J, Wijesuriya J, Russell MQ, Lyon RM. Determinants of prehospital lactate in trauma patients: a retrospective cohort study. BMC Emerg Med. 2020;20:18. https://doi.org/10.1186/s12873-020-00314-1.
Cerović O, Golubović V, Špec-Marn A, Kremžar B, Vidmar G. Relationship between injury severity and lactate levels in severely injured patients. Intensive Care Med. 2003;29:1300–5. https://doi.org/10.1007/s00134-003-1753-8.
Vincent J, Quintairos E, Silva A, Couto L, Taccone F. The value of blood lactate kinetics in critically ill patients: a systematic review. Crit Care. 2016;20:257. https://doi.org/10.1186/S13054-016-1403-5.
Dekker SE, de Vries H-M, Lubbers WD, van de Ven PM, Toor EJ, Bloemers FW, et al. Lactate clearance metrics are not superior to initial lactate in predicting mortality in trauma. Eur J Trauma Emerg Surg. 2017;43:841–51. https://doi.org/10.1007/s00068-016-0733-y.
Klein K, Lefering R, Jungbluth P, Lendemans S, Hussmann B. Is prehospital time important for the treatment of severely injured patients? A matched-triplet analysis of 13,851 patients from the TraumaRegister DGU®. Biomed Res Int. 2019. https://doi.org/10.1155/2019/5936345.
Martín-Rodríguez F, López-Izquierdo R, Delgado Benito JF, Sanz-García A, del Pozo VC, Castro Villamor MÁ, et al. Prehospital point-of-care lactate increases the prognostic accuracy of national early warning score 2 for early risk stratification of mortality: results of a multicenter, observational study. J Clin Med. 2020;9:1156. https://doi.org/10.3390/jcm9041156.
Martín-Rodríguez F, López-Izquierdo R, Medina-Lozano E, Ortega Rabbione G, del Pozo Vegas C, Carbajosa Rodríguez V, et al. Accuracy of prehospital point-of-care lactate in early in-hospital mortality. Eur J Clin Invest. 2020;50:e13341. https://doi.org/10.1111/eci.13341.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
PH (BG Unfallklinik Frankfurt am Main—Department of Trauma and Orthopedic Surgery) is the corresponding author. PF (BG Unfallklinik Frankfurt am Main—Department of Trauma and Orthopedic Surgery) made substantial contributions to the conception, the design of the work, the acquisition, the analysis and interpretation of data and was a major contributor in writing the manuscript. AK (BG Unfallklinik Frankfurt am Main—Department of Trauma and Orthopedic Surgery) made substantial contributions to the conception, the design of the work, the acquisition, the analysis and interpretation of data. YG (Ministry of Health—City of Frankfurt) made substantial contributions to the conception and the design of the work. RH (BG Unfallklinik Frankfurt am Main—Department of Trauma and Orthopedic Surgery) made substantial contributions to the conception and design of the work and substantively revised it. US (BG Unfallklinik Frankfurt am Main—Department of Trauma and Orthopedic Surgery) made substantial contributions to the conception, the design of the work, the acquisition, the analysis and interpretation of data and substantively revised it. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors listed below declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Ethics approval
The protocol of investigation was checked and approved by the Regional Ethics Committee (2020-1746-evBO).
Consent to participate
The requirement for informed consent was waived due to the retrospective study design.
Rights and permissions
About this article
Cite this article
Hagebusch, P., Faul, P., Klug, A. et al. Elevated serum lactate levels and age are associated with an increased risk for severe injury in trauma team activation due to trauma mechanism. Eur J Trauma Emerg Surg 48, 2717–2723 (2022). https://doi.org/10.1007/s00068-021-01811-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-021-01811-z