Abstract
Nowadays, approximately every patient affected from end-stage acute or chronic heart failure may be a potential candidate for MCS; therefore, a careful patient selection for MCS is crucial to establish an effective MCS program, having an impact on both the number of patient treated and the outcomes and the costs of the entire program.
Since MCS is a relatively young and still rapidly developing field, indications and institutional policies have been frequently modified over the past 30 years based on new available technologies or newly found clinical evidences. Nevertheless, due to the high individual variability of the clinical presentation of end stage heart failure it is nearly impossible to produce generally accepted patient selection criteria which guarantee best treatment for each individual patient.
For the last decade a clear paradigm shift has been made in the application of durable VADs in patients with acute, severe hemodynamic deterioration. Due to their higher risk for morbidity and mortality, longer ICU stay, higher incidence of debilitating complications, and significantly increased costs, the application of Temporary Circulatory Support (TCS) systems with lower costs and less invasiveness (percutaneous VAD) has been the first-line choice for those patients in their worst clinical conditions. Durable VADs proof best clinical results with hemodynamic stable end-stage heart failure patients.
The INTERMACS classification, introduced in the 90s, tried to classify the acuity and severity of end-stage heart failure patients based on their expected one year survival. This was one first attempt to introduce a standardization of the terminology for end-stage heart failure patients in order to scientifically compare the results and outcome of this expanding patient population when they were implanted a durable VAD.
Further selection criteria for MCS implantation to be considered:
-
Cost/benefit analysis
-
Device strategy (BTD, BTT, BTC, DT)
-
Underlying disease/etiology and eventual reversibility
-
Patient comorbidities and their reversibility
-
Frailty, nutritional status, and risk of infections
-
Assessment of hemorrhagic and thromboembolic risk
Once the decision of an MCS implantation has been considered as a valuable option, the following criteria should be further investigated:
-
Available risk scores
-
Right Heart Dysfunction Reversibility and/or need of preoperative management of right ventricle to reduce perioperative unplanned RVAD implantation
-
Management of the aortic valve to avoid approach of the aortic valve during mid-/long-term follow-up
-
Surgical management and/or need of eventual concomitant procedures
-
Need of pulsatility and eventual strategies to prevent hemorrhagic complications
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Fleischmann KE, Beckman JA, Buller CE et al (2009) 2009 ACCF/AHA Focused Update on Perioperative Beta Blockade: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation 120(21):2123–2151. http://dx.doi.org/10.1161/CIRCULATIONAHA.109.192689. ISSN 1524–4539
Kirklin JK et al (2015) Seventh INTERMACS annual report: 15,000 patients and counting. JHLT 34(12):1495–1504. doi:10.1016/j.healun.2015.10.003. ISSN 1053-2498
Patel CB, Cowger JA, Zuckermann A (2014) A contemporary review of mechanical circulatory support. J Heart Lung Transplant 33(7):667–674. https://doi.org/10.1016/j.healun.2014.02.014. ISSN 1557–3117
Lund LH, Edwards LB, Kucheryavaya, AY, Dipchand AI, Benden C, Christie JD, et al. The registry of the International Society for Heart and Lung Transplantation: Thirtieth Official Adult Heart Transplant Report—2013; Focus Theme: Age for the International Society for Heart and Lung Transplantation. 2013. doi: 10.1016/j.healun.2013.08.006
Kirklin JK, Cantor R, Mohacsi P, Gummert J, De By T, Hannan MM et al (2016) First annual IMACS report: a global International Society for Heart and Lung Transplantation Registry for Mechanical Circulatory Support. J Heart Lung Transplant 35(4):407–412. doi:10.1016/j.healun.2016.01.002
Khazanie P, Rogers JG (2011) Patient selection for left ventricular assist devices. Congest Heart Fail 17(5):227–234. doi:10.1111/j.1751-7133.2011.00236.x
Slaughter MS, Meyer AL, Birks EJ (2011) Destination therapy with left ventricular assist devices: patient selection and outcomes. Curr Opin Cardiol 26(3):232–236. doi:10.1097/HCO.0b013e328345aff4
Miller LW, Guglin M (2013) Patient selection for ventricular assist devices: a moving target. J Am Coll Cardiol 61(12):1209–1221. doi:10.1016/j.jacc.2012.08.1029
Lund LH, Matthews J, Aaronson K (2010) Patient selection for left ventricular assist devices. Eur J Heart Fail 12(5):434–443. doi:10.1093/eurjhf/hfq006
Angelo LD, Bovolo V, Frigerio M (2014) Ventricular assist devices for heart failure: a focus on patient selection and complications. Res Rep Clin Cardiol 5:199–211. doi:10.2147/RRCC.S48886
Long EF, Swain GW, Mangi AA (2014) Comparative survival and cost effectiveness of advanced therapies for end-stage heart failure. Circ Heart Failure. doi:10.1161/CIRCHEARTFAILURE.113.000807
Kirklin JK, Naftel DC, Kormos RL, Stevenson LW, Pagani FD, Miller MA et al (2012) The Fourth INTERMACS Annual Report: 4,000 implants and counting. J Heart Lung Transplant 31(2):117–126
Gilotra NA, Stevens GR (2015) Temporary mechanical circulatory support: a review of the options, indications, and outcomes. Clin Med Insights Cardiol 8(Suppl 1):75–85. doi:10.4137/CMC.s15718
Cowger J, Shah P, Stulak J, Maltais S, Aaronson KD, Kirklin JK et al (2016) INTERMACS profiles and modifiers: heterogeneity of patient classification and the impact of modifiers on predicting patient outcome. J Heart Lung Transplant 35:440–448. doi:10.1016/j.healun.2015.10.037 ISSN 1053-2498
Copeland JG, Copeland H, Gustafson M, Mineburg N, Covington D, Smith RG, Friedman M (2012) Experience with more than 100 total artificial heart implants. J Thorac Cardiovasc Surg 143(3):727–734. doi:10.1016/j.jtcvs.2011.12.002. Epub 2012 Jan 14. PMID: 22245242
Riebandt J, Haberl T, Mahr S, Laufer G, Rajek A, Steinlechner B, Schima H, Zimpfer D (2014) Preoperative patient optimization using extracorporeal life support improves outcomes of INTERMACS Level I patients receiving a permanent ventricular assist device. Eur J Cardiothorac Surg 46(3):486–492. ; discussion 492. doi: 10.1093/ejcts/ezu093. Epub 2014 Mar 18. PMID: 24648428
Young JB (2007) Heart failure’s near dead and dying. J Am Coll Cardiol 50(13):1291–1293. doi:10.1016/j.jacc.2007.07.008
Durinka JB, Bogar LJ, Hirose H, Brehm C, Koerner MM, Pae WE, Cavarocchi NC (2014) End-organ recovery is key to success for extracorporeal membrane oxygenation as a bridge to implantable left ventricular assist device. ASAIO J (American Society for Artificial Internal Organs : 1992) 60(2):189–192. doi:10.1097/MAT.0000000000000043
Shah P, Smith S, Haft JW, Desai SS, Burton NA, Romano MA, Cowger JA (2016) Clinical outcomes of advanced heart failure patients with cardiogenic shock treated with temporary circulatory support before durable lvad implant. ASAIO J 62(1):20–27. doi:10.1097/MAT.0000000000000309
Schumer EM, Ising MS, Trivedi JR, Slaughter MS, Cheng A (2015) Early outcomes with marginal donor hearts compared with left ventricular assist device support in patients with advanced heart failure. Ann Thorac Surg 100:522–527. doi:10.1016/j.athoracsur.2015.02.089
Stewart GC, Kittleson MM, Cowger JA, Johnson FL, Patel CB, Mountis MM et al (2015) Who wants a left ventricular assist device for ambulatory heart failure? Early insights from the MEDAMACS screening pilot. J Heart Lung Transplant 34(12):1630–1633. doi:10.1016/j.healun.2015.07.009
Estep JD, Starling RC, Horstmanshof DA, Milano CA, Selzman CH, Shah KB, et al., for the ROADMAP Study Investigators. Risk assessment and comparative effectiveness of left ventricular assist device and medical management in ambulatory heart failure patients. J Am Coll Cardiol. 2016;66(16):1747–1761. doi:10.1016/j.jacc.2015.07.075
Miller LW, Guglin M, Rogers J (2013) Cost of ventricular assist devices can we afford the progress? Circulation 127(6):743–748. doi:10.1161/CIRCULATIONAHA.112.13982
Slaughter MS (2010) Advances in LVAD patient management: clinical strategies to minimize adverse events. PARADIGM Adv Heart Fail Technol 3:1–2
Pulikottil-Jacob R, Suri G, Connock M, Kandala NB, Sutcliffe P, Maheswaran H, Banner NR, Clarke A. Comparative cost-effectiveness of the HeartWare versus HeartMate II left ventricular assist devices used in the United Kingdom National Health Service bridge-to-transplant program for patients with heart failure J Heart Lung Transplant 2014;33(4):350–358. doi:10.1016/j.healun.2014.01.003. Epub 2014 Jan 19. PMID: 24582838
Liao L, Allen LA, Whellan DJ (2008) Economic burden of heart failure in the elderly. PharmacoEconomics 26:447–462
Uriel N, Jorde UP, Woo Pak S, Jiang J, Clerkin K, Takayama H, Mancini DM (2013) Impact of long term left ventricular assist device therapy on donor allocation in cardiac transplantation. J Heart Lung Transplant 32(2):188–195. doi:10.1016/j.healun.2012.11.010
Fang JC, Stehlik J (2013) Moving beyond “bridges”∗. JACC Heart Failure 1(5):379–381. doi:10.1016/j.jchf.2013.08.003
Drakos SG, Kfoury AG, Stehlik J, Selzman CH, Reid BB, Terrovitis JV, Li DY (2012) Bridge to recovery: understanding the disconnect between clinical and biological outcomes. Circulation 126(2):230–241. doi:10.1161/CIRCULATIONAHA.111.040261
Ammirati E et al (2014) Current indications for heart transplantation and left ventricular assist device: a practical point of view. Eur J Intern Med 25(5):422–429. doi:10.1016/j.ejim.2014.02.006
Tsipouras MG, Karvounis EC, Tzallas AT, Katertsidis NS, Goletsis Y, Frigerio M, Verde A, Trivella MG, Fotiadis DI (2013) Adverse event prediction in patients with left ventricular assist devices. Conf Proc IEEE Eng Med Biol Soc 2013:1314–1317. doi:10.1109/EMBC.2013.6609750
Akhter SA, Badami A, Murray M, Kohmoto T, Lozonschi L, Osaki S, Lushaj EB (2015) Hospital readmissions after continuous-flow left ventricular assist device implantation: incidence, causes, and cost analysis. Ann Thorac Surg 100(3):884–889. doi:10.1016/j.athoracsur.2015.03.010. Epub 2015 Jun 19
Meyns BP, Simon A, Klotz S, Wittwer T, Schlensak C, Rega F, Burkhoff D. Clinical benefits of partial circulatory support in New York Heart Association Class IIIB and Early Class IV patients.Eur J Cardiothorac Surg 2011;39(5):693–698. doi: 10.1016/j.ejcts.2010.07.049. Epub 2010 Oct 8. PMID: 20934882
Zucchetta F, Tarzia V, Bottio T, Gerosa G (2014) The Jarvik-2000 ventricular assist device implantation: how we do it. Ann Cardiothorac Surg 3(5):525–531. doi:10.3978/j.issn.2225-319X.2014.09.09
Frazier OH, Myers TJ, Westaby S, Gregoric ID (2003) Use of the Jarvik 2000 left ventricular assist system as a bridge to heart transplantation or as destination therapy for patients with chronic heart failure. Ann Surg 237(5):631–636; discussion 636–637. doi:10.1097/01.SLA.0000064359.90219.44
Westaby S, Siegenthaler M, Beyersdorf F, Massetti M, Pepper J, Khayat A, Frazier OH (2010) Destination therapy with a rotary blood pump and novel power delivery. Eur J Cardiothorac Surg 37(2):350–356. doi:10.1016/j.ejcts.2009.03.071
Wever-Pinzon O, Selzman CH, Drakos SG, Saidi A, Stoddard GJ, Gilbert EM, Labedi M, Reid BB, Davis ES, Kfoury AG, Li DY, Stehlik J, Bader F (2013) Pulsatility and the risk of nonsurgical bleeding in patients supported with the continuous-flow left ventricular assist device HeartMate II. Circ Heart Fail 6(3):517–526. doi:10.1161/CIRCHEARTFAILURE.112.000206. Epub 2013 Mar 11
Moazami N, Dembitsky WP, Adamson R, Steffen RJ, Soltesz EG, Starling RC, Fukamachi K (2015) Does pulsatility matter in the era of continuous-flow blood pumps? J Heart Lung Transplant 34(8):999–1004. doi:10.1016/j.healun.2014.09.012. Epub 2014 Sep 28
Imamura T, Kinugawa K, Nitta D, Hatano M, Kinoshita O, Nawata K, Ono M. Advantage of pulsatility in left ventricular reverse remodeling and aortic insufficiency prevention during left ventricular assist device treatment Circ J 2015;79(9):1994–9. doi: 10.1253/circj.CJ-15-0419. Epub 2015 Jun 25 PMID: 26118343
Tolpen S, Janmaat J, Reider C, Kallel F, Farrar D, May-Newman K (2015) Programmed speed reduction enables aortic valve opening and increased pulsatility in the LVAD-assisted heart. ASAIO J 61(5):540–547. doi:10.1097/MAT.0000000000000241
Ising MS, Sobieski MA, Slaughter MS, Koenig SC, Giridharan GA. Feasibility of pump speed modulation for restoring vascular pulsatility with rotary blood pumps ASAIO J 2015;61(5):526–532. doi: 10.1097/MAT.0000000000000262. PMID: 26102173
Bourque K, Cotter C, Dague C, Harjes D, Dur O, Duhamel J, Spink K, Walsh K, Burke E (2016) Design rationale and preclinical evaluation of the HeartMate 3 left ventricular assist system for hemocompatibility. ASAIO J 62(4):375–383. doi:10.1097/MAT.0000000000000388
Kimura M, Kinoshita O, Nawata K, Nishimura T, Hatano M, Imamura T, Endo M, Kagami Y, Kubo H, Kashiwa K, Kinugawa K, Kyo S, Komuro I, Ono M (2015) Midterm outcome of implantable left ventricular assist devices as a bridge to transplantation: Single-center experience in Japan. J Cardiol 65(5):383–389. doi:10.1016/j.jjcc.2014.06.007. Epub 2014 Jul 14. PMID: 25034705
Jabbar HR, Abbas A, Ahmed M, Klodell CT Jr, Chang M, Dai Y, Draganov PV (2015) The incidence, predictors and outcomes of gastrointestinal bleeding in patients with left ventricular assist device (LVAD). Dig Dis Sci 60(12):3697–3706. doi:10.1007/s10620-015-3743-4. Epub 2015 Jun 14
Jorde UP (2016) Relative preservation of high molecular weight von Willebrand factor multimers during HM 3 support–plain physics or a matter of clinical consequence? J Heart Lung Transplant 35(7):857–859. doi:10.1016/j.healun.2016.06.007
Cheng A, Williamitis CA, Slaughter MS (2014) Comparison of continuous-flow and pulsatile-flow left ventricular assist devices: is there an advantage to pulsatility? Ann Cardiothorac Surg 3(6):573–581. doi:10.3978/j.issn.2225-319X.2014.08.24
John R, Aaronson KD, Pae WE, Acker MA, Hathaway DR, Najarian KB, Slaughter MS, HeartWare Bridge to Transplant ADVANCE Trial Investigators (2014) Drive-line infections and sepsis in patients receiving the HVAD system as a left ventricular assist device. J Heart Lung Transplant 33(10):1066–1073. doi:10.1016/j.healun.2014.05.010. Epub 2014 Jun 4.PMID: 25087103
Gray BW, Haft JW, Hirch JC, Annich GM, Hirschl RB, Bartlett RH, Support EL (2015) ASAIO J 61:2–7. doi:10.1097/MAT.0000000000000150
Chang CH, Chen HC, Caffrey JL et al (2011) Survival analysis after extracorporeal membrane oxygenation in critically ill adults: a comparison with conventional cardiopulmonary resuscitation. Crit Care Med 39:1. doi:10.1097/CCM.0b013e3181feb339
Hacking DF, Best D, d’Udekem Y, Brizard CP, Konstantinov IE, Millar J, Butt W (2015) Elective decompression of the left ventricle in pediatric patients may reduce the duration of venoarterial extracorporeal membrane oxygenation. Artif Organs 39(4):319–326. doi:10.1111/aor.12390. Epub 2014 Oct 20
Lee M, Akashi H, Kato TS, Takayama H, Wu C, Xu K, Collado E, Weber MP, Kennel PJ, Brunjes DL, Ji R, Naka Y, George I, Mancini D, Farr M, Christian Schulze P (2016) Vascular inflammation and abnormal aortic histomorphometry in patients after pulsatile- and continuous-flow left ventricular assist device placement. J Heart Lung Transplant. pii: S1053–2498(16)00022-X. doi:10.1016/j.healun.2015.12.027 [Epub ahead of print]
Topilsky Y, Pereira NL, Shah DK, Boilson B, Schirger JA, Kushwaha SS, Joyce LD, Park SJ (2011) Left ventricular assist device therapy in patients with restrictive and hypertrophic cardiomyopathy. Circ Heart Fail 4:266–275. doi:10.1161/CIRCHEARTFAILURE.110.959288
Ammash NM, Seward JB, Bailey KR, Edwards WD, Tajik AJ (2000) Clinical profile and outcome of idiopathic restrictive cardiomyopathy. Circulation 101:2490–2496
Frazier OH, Gregoric ID, Messner GN (2005) Total circulatory support with an LVAD in an adolescent with a previous Fontan procedure. Tex Heart Inst J 32(3):402–404. PMID: 16392230
Weinstein S, Bello R, Pizarro C, Fynn-Thompson F, Kirklin J, Guleserian K, Woods R, Tjossem C, Kroslowitz R, Friedmann P, Jaquiss R (2014) The use of the Berlin Heart EXCOR in patients with functional single ventricle. J Thorac Cardiovasc Surg 147(2):697–704; discussion 704–705. doi:10.1016/j.jtcvs.2013.10.030. Epub 2013 Nov 28
Ryan TD, Jefferies JL, Zafar F, Lorts A, Morales DL (2015) The evolving role of the total artificial heart in the management of end-stage congenital heart disease and adolescents. ASAIO J 61(1):8–14. doi:10.1097/MAT.0000000000000156. Review
Takeda K, Naka Y, Yang JA, Uriel N, Colombo PC, Jorde UP, Takayama H (2014) Outcome of unplanned right ventricular assist device support for severe right heart failure after implantable left ventricular assist device insertion. J Heart Lung Transplant 33(2):141–148. doi:10.1016/j.healun.2013.06.025. Epub 2013 Aug 6. PMID: 23932442
Patlolla B, Beygui R, Haddad F (2013) Right-ventricular failure following left ventricle assist device implantation. Curr Opin Cardiol 28(2):223–233. doi:10.1097/HCO.0b013e32835dd12c
Lampert BC, Teuteberg JJ (2015) Right ventricular failure after left ventricular assist devices. J Heart Lung Transplant 34(9):1123–1130. doi:10.1016/j.healun.2015.06.015
Dandel M et al (2015) Left ventricular vs. biventricular mechanical support: decision making and strategies for avoidance of right heart failure after left ventricular assist device implantation. Int J Cardiol 198:241–250. doi:10.1016/j.ijcard.2015.06.103
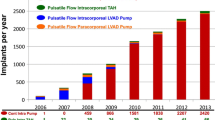
Reichenspurner H (2015) When is the patient sick enough to implant MCS ? – importance and assessment of RV function ISHLT number of transplants by year, 2014–2015
Ihnken KA, Ramzy D, Esmailian F, Trento A, Arabía FA (2016) Surgical technique to facilitate explanation of mechanical circulatory support devices: LVADs, BiVADs, and TAHs before heart transplantation. ASAIO J 62(2):211–213. doi:10.1097/MAT.0000000000000318. PMID: 26692405
Slaughter MS, Pagani FD, Rogers JG, Miller LW, Sun B, Russell SD et al (2010) Clinical management of continuous-flow left ventricular assist devices in advanced heart failure. J Heart Lung Transplant 29(4 SUPPL):S1–S39. doi:10.1016/j.healun.2010.01.011
Cowger, J., Romano, M.A, Stulak, J., Pagani, F. D., & Aaronson, K.D. (2011). Left ventricular assist device management in patients chronically supported for advanced heart failure. Curr Opin Cardiol, 26(2), 149–154. doi:10.1097/HCO.0b013e3283438258
Danchin N, Puymirat E (2011) 1980–2010: the three glorious decades of cardiology. A comprehensive and collective effort rewarded by outstanding clinical results. Rev Española Cardiología (English Ed) 64(11):959–961. doi:10.1016/j.rec.2011.08.001
Lee S, Fukamachi K, Golding L, Moazami N, Starling RC (2013) Left ventricular assist devices: from the bench to the clinic. Cardiology 125(1):1–12. doi:10.1159/000346865. PMID: 10831523
Patel AM, Adeseun G a, Ahmed I, Mitter N, Rame JE, Rudnick MR (2013) Renal failure in patients with left ventricular assist devices. Clin J Am Soc Nephrol CJASN 8:484–496. doi:10.2215/CJN.06210612
Kirklin JK et al (2013) Quantifying the effect of cardiorenal syndrome on mortality after left ventricular assist device implant. J Heart Lung Transplant 32(12):1205–1213
Nguyen PH, Tuzun E, Quick CM (2016) Aortic pulse pressure homeostasis emerges from physiologic adaptation of systemic arteries to local mechanical stresses. Am J Physiol Regul Integr Comp Physiol 311(3):R522–R531. doi:10.1152/ajpregu.00402.2015
Flint KM, Matlock DD, Lindenfeld J, Allen LA (2012) Frailty and the selection of patients for destination therapy left ventricular assist device. Circ Heart Fail 5(2):286–293. doi:10.1161/CIRCHEARTFAILURE.111.963215
Ravichandran AK, Cowger J (2015) Left ventricular assist device patient selection: do risk scores help? J Thorac Dis 7(12):2080–2087. doi:10.3978/j.issn.2072-1439.2015.11.02
Scandroglio AM, Pieri M, Zangrillo A, Kaufmann F, Falk V, Potapov E, Krabatsch T (2016) Role of survival scores before left ventricular assist device implantation. ASAIO J 62(4):438–441. doi:10.1097/MAT.0000000000000376
Yang Q, Zimmerman J, Steinfeld A, Carey L, Antaki JF (2016) Investigating the heart pump implant decision process: opportunities for decision support tools to help. In: Proceedings of the 2016 CHI conference on human factors in computing systems (CHI ‘16). ACM, New York, pp 4477–4488. doi: http://dx.doi.org/10.1145/2858036.2858373
Kilic A, Acker MA, Atluri P (2015) Dealing with surgical left ventricular assist device complications. Journal of Thoracic Disease. AME Publications. doi:10.3978/j.issn.2072-1439.2015.10.64
Himmelreich G, Ullmann H, Riess H, Rosch R, Loebe M, Schiessler A, Hetzer R (1995) Pathophysiologic role of contact activation in bleeding followed by thromboembolic complications after implantation of a ventricular assist device. ASAIO J 41:M790–M794. PMID: 8573916
Atluri P, Goldstone AB, Kobrin DM, Cohen JE, MacArthur JW, Howard JL, Jessup ML, Rame JE, Acker MA, Woo YJ (2013) Ventricular assist device implant in the elderly is associated with increased, but respectable risk: a multi-institutional study. Ann Thorac Surg 96(1):141–147. doi:10.1016/j.athoracsur.2013.04.010
Crow S, Chen D, Milano C, Thomas W, Joyce L, Piacentino V, Sharma R, Wu J, Arepally G, Bowles D, Rogers J, Villamizar-Ortiz N (2010) Acquired von Willebrand syndrome in continuous-flow ventricular assist device recipients. Ann Thorac Surg 90:1263–1269. doi:10.1016/j.athoracsur.2010.04.099
Munoz SJ, Stravitz RT, Gabriel DA (2009) Coagulopathy of acute liver failure. Clin Liver Dis 13(1):95–107. doi:10.1016/j.cld.2008.10.001
Uriel N, Pak SW, Jorde UP, Jude B, Susen S, Vincentelli A, Ennezat PV, Cappelman S, Naka Y, Mancini D (2010) Acquired von Willebrand syndrome after continuous-flow mechanical device support contributes to a high prevalence of bleeding during long-term support and at the time of transplantation. J Am Coll Cardiol 56:1207–1213. doi:10.1016/j.jacc.2010.05.016. Epub 2010 Jul 2
Kulminski AM, Ukraintseva SV, Culminskaya IV et al (2008) Cumulative deficits and physiological indices as predictors of mortality and long life. J Gerontol A Biol Sci Med Sci 63:1053–1059. PMID: 18948555 PMCID: PMC2684458
Chung CJ, Wu JM, Kato TS, Dam TT, Givens RC, Templeton DL, Maurer MS, Naka Y, Takayama H, Mancini DM, Schulze PC (2014) Reduced handgrip strength as a marker of frailty predicts clinical outcomes in patients with heart failure undergoing ventricular assist device placement. J Card Fail 20(5):310–315. doi:10.1016/j.cardfail.2014.02.008. Epub 2014 Feb 22
Kobrin DM, Donnelly JP, Acker AL, Howard JL, Zalewski CM, Walsh SL, Hill CE, O’Hara ML, Marble JF, Atluri P, Wald JW, Goldberg LR, Woo YJ, Acker MA, Rame JE (2013) Dynamic BMI changes in patients implanted with continuous flow left ventricular assist devices: evidence for reversibility of cardiac cachexia and impact on survival. J Heart Lung Transplant 32(4S):S90–S91
Sileshi B, O’Hara BK, Davis ME, Haglund NA, Meng X, Deegan R et al (2016) Outcomes of patients implanted using a left thoracotomy technique for a miniaturized centrifugal continuous-flow pump. ASAIO J. doi:10.1097/MAT.0000000000000407
Sileshi B, Haglund NA, Davis ME, Tricarico NM, Stulak JM, Khalpey Z et al (2015) In-hospital outcomes of a minimally invasive off-pump left thoracotomy approach using a centrifugal continuous-flow left ventricular assist device. J Heart Lung Transplant 34(1):107–112. doi:10.1016/j.healun.2014.09.023
Hanke JS, Haverich A, Schmitto JD (2016) Right heart failure after left ventricular assist devices: surgical considerations. J Heart Lung Transplant 35(3):395–396. doi:10.1016/j.healun.2015.12.013
Leprince P et al Patients with a body surface area less than 1.7 m2 have a good outcome with the cardiowest total artificial heart. J Heart Lung Transplant 24(10):1501–1505. doi: http://dx.doi.org/10.1016/j.healun.2005.01.016
Kalya A, Jaroszewski D, Pajaro O, et al (2013) Role of total artificial heart in the management of heart transplant rejection and retransplantation: case report and review. Clin Transplant. 2013;27(4):E348–50. doi:10.1111/ctr.12146. Epub 2013 May 31
Wells D, Villa CR, Simón Morales DL. (2017) The 50/50 cc Total Artificial Heart Trial: Extending the Benefits of the Total Artificial Heart to Underserved Populations. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu. 2017;20:16–19. doi:10.1053/j.pcsu.2016.09.004
Saffarzadeh A, Bonde P (2015) Options for temporary mechanical circulatory support. J Thorac Dis AME Publications. doi:10.3978/j.issn.2072-1439.2015.09.14
Acharya D, Loyaga-Rendon RY, Pamboukian SV, Tallaj JA, Holman WL, Cantor RS et al (2016) Ventricular assist device in acute myocardial infarction. J Am Coll Cardiol 67(16):1871–1880. doi:10.1016/j.jacc.2016.02.025.
Raman L, Dalton HJ (2016) Year in review 2015: Extracorporeal membrane oxygenation. Respir Care 61(7):986–991. doi:10.4187/respcare.04985
Author information
Authors and Affiliations
Corresponding authors
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Amarelli, C., Buonocore, M., Maiello, C., Montalto, A., Wieselthaler, G. (2017). MCS Candidate Selection Criteria. In: Montalto, A., Loforte, A., Musumeci, F., Krabatsch, T., Slaughter, M. (eds) Mechanical Circulatory Support in End-Stage Heart Failure. Springer, Cham. https://doi.org/10.1007/978-3-319-43383-7_4
Download citation
DOI: https://doi.org/10.1007/978-3-319-43383-7_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-43381-3
Online ISBN: 978-3-319-43383-7
eBook Packages: MedicineMedicine (R0)