Abstract
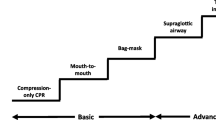
Airway care of the patient with life threatening haemorrhage presents many challenges during damage control resuscitation. The essential requirements are to maintain oxygenation at all stages of care and when necessary deliver general anaesthesia to facilitate invasive haemorrhage control procedures. In the remote, pre-hospital setting, providers must be able to assess the airway and intervene with a range of strategies to prevent hypoxaemia. These interventions may vary from basic airway opening manoeuvres to advanced techniques such as drug-assisted rapid sequence intubation. The initial delivery of these skills in remote settings will be the responsibility of whichever medical provider is present, and so their training, equipment and decision-making skills must reflect the challenges they will face. Rapid sequence intubation skills may not be widely available in remote environments and so providers must be equipped with alternative airway management strategies including cricothyrotomy and use of extraglottic airway devices. When invasive haemorrhage control procedures are required for patients with life threatening haemorrhage, rapid sequence intubation will need to be performed. This procedure carries significant risk in the presence of haemorrhagic shock. Providers must be aware of the hypotensive effects of induction agents and the adverse impact of positive pressure ventilation upon cardiac output in the presence of life threatening haemorrhage. The risks of intubation should be minimised with appropriate blood production administration and ventilation techniques as part of a coordinated damage control resuscitation strategy.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
Abbreviations
- BURP:
-
Backwards upwards rightwards pressure
- DO2 :
-
Oxygen delivery
- EAD:
-
Extraglottic airway device
- ELM:
-
External laryngeal manipulation
- EMS:
-
Emergency medical services
- EtCO2 :
-
End-tidal carbon dioxide
- ETI:
-
Endotracheal intubation
- ETT:
-
Endotracheal tube
- HEMS:
-
Helicopter emergency medical services
- LMA:
-
Laryngeal mask airway
- MILS:
-
Manual in line stabilisation
- MTF:
-
Medical treatment facility
- NMBA:
-
Neuromuscular blocking agent
- NPA:
-
Nasopharyngeal airway
- OPA:
-
Oropharyngeal airway
- PALM:
-
Pharmacologically assisted laryngeal mask
- RSI:
-
Rapid sequence intubation
- TBI:
-
Traumatic brain injury
- TCCC:
-
Tactical combat casualty care
- TECC:
-
Tactical emergency casualty care
References
Davis JS, Satahoo SS, Butler FK, Dermer H, Naranjo D, Julien K, Van Haren RM, Namias N, Blackbourne LH, Schulman CI. An analysis of prehospital deaths: who can we save? J Trauma Acute Care Surg. 2014;77(2):213–8.
Kleber C, Giesecke MT, Tsokos M, Haas NP, Buschmann CT. Trauma-related preventable deaths in Berlin 2010: need to change prehospital management strategies and trauma management education. World J Surg. 2013;37(5):1154–61.
Eastridge BJ, Mabry RL, Seguin P, Cantrell J, Tops T, Uribe P, Mallett O, Zubko T, Oetjen-Gerdes L, Rasmussen TE, et al. Death on the battlefield (2001-2011): implications for the future of combat casualty care. J Trauma Acute Care Surg. 2012;73(6 Suppl 5):S431–7.
Kotwal RS, Montgomery HR, Kotwal BM, Champion HR, Butler FK Jr, Mabry RL, Cain JS, Blackbourne LH, Mechler KK, Holcomb JB. Eliminating preventable death on the battlefield. Arch Surg. 2011;146(12):1350–8.
Barbee RW, Reynolds PS, Ward KR. Assessing shock resuscitation strategies by oxygen debt repayment. Shock. 2010;33(2):113–22.
Adams BD, Cuniowski PA, Muck A, De Lorenzo RA. Registry of emergency airways arriving at combat hospitals. J Trauma. 2008;64(6):1548–54.
Lockey DJ, Healey B, Crewdson K, Chalk G, Weaver AE, Davies GE. Advanced airway management is necessary in prehospital trauma patients. Br J Anaesth. 2015;114(4):657–62.
Ruppert M, Reith MW, Widmann JH, Lackner CK, Kerkmann R, Schweiberer L, Peter K. Checking for breathing: evaluation of the diagnostic capability of emergency medical services personnel, physicians, medical students, and medical laypersons. Ann Emerg Med. 1999;34(6):720–9.
Silvestri S, Ralls GA, Krauss B, Thundiyil J, Rothrock SG, Senn A, Carter E, Falk J. The effectiveness of out-of-hospital use of continuous end-tidal carbon dioxide monitoring on the rate of unrecognized misplaced intubation within a regional emergency medical services system. Ann Emerg Med. 2005;45(5):497–503.
Hyldmo PK, Vist GE, Feyling AC, Rognas L, Magnusson V, Sandberg M, Soreide E. Does turning trauma patients with an unstable spinal injury from the supine to a lateral position increase the risk of neurological deterioration?–A systematic review. Scand J Trauma Resusc Emerg Med. 2015;23:65.
Ramasamy A, Midwinter M, Mahoney P, Clasper J. Learning the lessons from conflict: pre-hospital cervical spine stabilisation following ballistic neck trauma. Injury. 2009;40(12):1342–5.
Kaups KL, Davis JW. Patients with gunshot wounds to the head do not require cervical spine immobilization and evaluation. J Trauma. 1998;44(5):865–7.
Stoneham MD. The nasopharyngeal airway. Assessment of position by fibreoptic laryngoscopy. Anaesthesia. 1993;48(7):575–80.
Steinbruner D, Mazur R, Mahoney PF. Intracranial placement of a nasopharyngeal airway in a gun shot victim. Emerg Med J. 2007;24(4):311.
Zwank M. Middle turbinectomy as a complication of nasopharyngeal airway placement. Am J Emerg Med. 2009;27(4):513 e3–4.
Paix BR, Griggs WM. Emergency surgical cricothyroidotomy: 24 successful cases leading to a simple ‘scalpel-finger-tube’ method. Emerg Med Australas. 2012;24(1):23–30.
Langvad S, Hyldmo PK, Nakstad AR, Vist GE, Sandberg M. Emergency cricothyrotomy – a systematic review. Scand J Trauma Resusc Emerg Med. 2013;21:43.
Barnard EB, Ervin AT, Mabry RL, Bebarta VS. Prehospital and en route cricothyrotomy performed in the combat setting: a prospective, multicenter, observational study. J Spec Oper Med. 2014;14(4):35–9.
Katzenell U, Lipsky AM, Abramovich A, Huberman D, Sergeev I, Deckel A, Kreiss Y, Glassberg E. Prehospital intubation success rates among Israel Defense Forces providers: epidemiologic analysis and effect on doctrine. J Trauma Acute Care Surg. 2013;75(2. Suppl 2):S178–83.
Kyle T, le Clerc S, Thomas A, Greaves I, Whittaker V, Smith JE. The success of battlefield surgical airway insertion in severely injured military patients: a UK perspective. J R Army Med Corps. 2016;162(6):460–4.
Moss R, Porter K, Greaves I, Consensus Group Faculty of Pre-Hospital C. Pharmacologically assisted laryngeal mask insertion: a consensus statement. Emerg Med J. 2013;30(12):1073–5.
Otten EJ, Montgomery HR, Butler FK Jr. Extraglottic airways in tactical combat casualty care: TCCC guidelines change 17-01 28 August 2017. J Spec Oper Med. 2017;17(4):19–28.
Bernard SA, Nguyen V, Cameron P, Masci K, Fitzgerald M, Cooper DJ, Walker T, Std BP, Myles P, Murray L, et al. Prehospital rapid sequence intubation improves functional outcome for patients with severe traumatic brain injury: a randomized controlled trial. Ann Surg. 2010;252(6):959–65.
Cobas MA, De la Pena MA, Manning R, Candiotti K, Varon AJ. Prehospital intubations and mortality: a level 1 trauma center perspective. Anesth Analg. 2009;109(2):489–93.
Stockinger ZT, McSwain NE Jr. Prehospital endotracheal intubation for trauma does not improve survival over bag-valve-mask ventilation. J Trauma. 2004;56(3):531–6.
Band RA, Salhi RA, Holena DN, Powell E, Branas CC, Carr BG. Severity-adjusted mortality in trauma patients transported by police. Ann Emerg Med. 2014;63(5):608–14 e3.
Huber S, Cronlein M, von Matthey F, Hanschen M, Seidl F, Kirchhoff C, Biberthaler P, Lefering R, Huber-Wagner S, TraumaRegister DGU. Effect of private versus emergency medical systems transportation in trauma patients in a mostly physician based system – a retrospective multicenter study based on the TraumaRegister DGU(R). Scand J Trauma Resusc Emerg Med. 2016;24:60.
Crewdson K, Rehn M, Brohi K, Lockey DJ. Pre-hospital emergency anaesthesia in awake hypotensive trauma patients: beneficial or detrimental? Acta Anaesthesiol Scand. 2018;62:504.
Baraka AS, Taha SK, Aouad MT, El-Khatib MF, Kawkabani NI. Preoxygenation: comparison of maximal breathing and tidal volume breathing techniques. Anesthesiology. 1999;91(3):612–6.
Pavlov I, Medrano S, Weingart S. Apneic oxygenation reduces the incidence of hypoxemia during emergency intubation: a systematic review and meta-analysis. Am J Emerg Med. 2017;35(8):1184–9.
Wimalasena Y, Burns B, Reid C, Ware S, Habig K. Apneic oxygenation was associated with decreased desaturation rates during rapid sequence intubation by an Australian helicopter emergency medicine service. Ann Emerg Med. 2015;65(4):371–6.
Shafer SL. Shock values. Anesthesiology. 2004;101(3):567–8.
Upchurch CP, Grijalva CG, Russ S, Collins SP, Semler MW, Rice TW, Liu D, Ehrenfeld JM, High K, Barrett TW, et al. Comparison of etomidate and ketamine for induction during rapid sequence intubation of adult trauma patients. Ann Emerg Med. 2017;69(1):24–33 e2.
Morris C, Perris A, Klein J, Mahoney P. Anaesthesia in haemodynamically compromised emergency patients: does ketamine represent the best choice of induction agent? Anaesthesia. 2009;64(5):532–9.
Chernow B, Lake CR, Cruess D, Coyle J, Hughes P, Balestrieri F, Casey L, Rainey TG, Fletcher JR. Plasma, urine, and CSF catecholamine concentrations during and after ketamine anesthesia. Crit Care Med. 1982;10(9):600–3.
Gelissen HP, Epema AH, Henning RH, Krijnen HJ, Hennis PJ, den Hertog A. Inotropic effects of propofol, thiopental, midazolam, etomidate, and ketamine on isolated human atrial muscle. Anesthesiology. 1996;84(2):397–403.
Miller M, Kruit N, Heldreich C, Ware S, Habig K, Reid C, Burns B. Hemodynamic response after rapid sequence induction with ketamine in out-of-hospital patients at risk of shock as defined by the shock index. Ann Emerg Med. 2016;68(2):181–8.e2.
Bruder EA, Ball IM, Ridi S, Pickett W, Hohl C. Single induction dose of etomidate versus other induction agents for endotracheal intubation in critically ill patients. Cochrane Database Syst Rev. 2015;1:CD010225.
Lockey D, Davies G, Coats T. Survival of trauma patients who have prehospital tracheal intubation without anaesthesia or muscle relaxants: observational study. BMJ. 2001;323(7305):141.
Magorian T, Flannery KB, Miller RD. Comparison of rocuronium, succinylcholine, and vecuronium for rapid-sequence induction of anesthesia in adult patients. Anesthesiology. 1993;79(5):913–8.
Tran DT, Newton EK, Mount VA, Lee JS, Wells GA, Perry JJ. Rocuronium versus succinylcholine for rapid sequence induction intubation. Cochrane Database Syst Rev. 2015;(10):CD002788.
Adnet F, Le Moyec L, Smith CE, Galinski M, Jabre P, Lapostolle F. Stability of succinylcholine solutions stored at room temperature studied by nuclear magnetic resonance spectroscopy. Emerg Med J. 2007;24(3):168–9.
Levitan RM, Mickler T, Hollander JE. Bimanual laryngoscopy: a videographic study of external laryngeal manipulation by novice intubators. Ann Emerg Med. 2002;40(1):30–7.
Takahata O, Kubota M, Mamiya K, Akama Y, Nozaka T, Matsumoto H, Ogawa H. The efficacy of the “BURP” maneuver during a difficult laryngoscopy. Anesth Analg. 1997;84(2):419–21.
Ellis DY, Harris T, Zideman D. Cricoid pressure in emergency department rapid sequence tracheal intubations: a risk-benefit analysis. Ann Emerg Med. 2007;50(6):653–65.
Mort TC. Emergency tracheal intubation: complications associated with repeated laryngoscopic attempts. Anesth Analg. 2004;99(2):607–13, table of contents.
Cournand A, Motley HL, et al. Physiological studies of the effects of intermittent positive pressure breathing on cardiac output in man. Am J Phys. 1948;152(1):162–74.
Pepe PE, Lurie KG, Wigginton JG, Raedler C, Idris AH. Detrimental hemodynamic effects of assisted ventilation in hemorrhagic states. Crit Care Med. 2004;32(9 Suppl):S414–20.
Convertino VA, Ryan KL, Rickards CA, Cooke WH, Idris AH, Metzger A, Holcomb JB, Adams BD, Lurie KG. Inspiratory resistance maintains arterial pressure during central hypovolemia: implications for treatment of patients with severe hemorrhage. Crit Care Med. 2007;35(4):1145–52.
Taghavi S, Jayarajan SN, Ferrer LM, Vora H, McKee C, Milner RE, Gaughan JP, Dujon J, Sjoholm LO, Pathak A, et al. “Permissive hypoventilation” in a swine model of hemorrhagic shock. J Trauma Acute Care Surg. 2014;77(1):14–9.
Herff H, Paal P, von Goedecke A, Lindner KH, Severing AC, Wenzel V. Influence of ventilation strategies on survival in severe controlled hemorrhagic shock. Crit Care Med. 2008;36(9):2613–20.
van Wessem KJ, Hennus MP, Heeres M, Koenderman L, Leenen LP. Mechanical ventilation is the determining factor in inducing an inflammatory response in a hemorrhagic shock model. J Surg Res. 2013;180(1):125–32.
Dutton RP. Resuscitative strategies to maintain homeostasis during damage control surgery. Br J Surg. 2012;99(Suppl 1):21–8.
Himmelseher S, Durieux ME. Revising a dogma: ketamine for patients with neurological injury? Anesth Analg. 2005;101(2):524–34, table of contents.
Zeiler FA, Teitelbaum J, West M, Gillman LM. The ketamine effect on ICP in traumatic brain injury. Neurocrit Care. 2014;21(1):163–73.
Chesnut RM, Marshall LF, Klauber MR, Blunt BA, Baldwin N, Eisenberg HM, Jane JA, Marmarou A, Foulkes MA. The role of secondary brain injury in determining outcome from severe head injury. J Trauma. 1993;34(2):216–22.
Manley G, Knudson MM, Morabito D, Damron S, Erickson V, Pitts L. Hypotension, hypoxia, and head injury: frequency, duration, and consequences. Arch Surg. 2001;136(10):1118–23.
Spaite DW, Hu C, Bobrow BJ, Chikani V, Barnhart B, Gaither JB, Denninghoff KR, Adelson PD, Keim SM, Viscusi C, et al. The effect of combined out-of-hospital hypotension and hypoxia on mortality in major traumatic brain injury. Ann Emerg Med. 2017;69(1):62–72.
Denninghoff KR, Griffin MJ, Bartolucci AA, Lobello SG, Fine PR. Emergent endotracheal intubation and mortality in traumatic brain injury. West J Emerg Med. 2008;9(4):184–9.
Hussmann B, Lefering R, Waydhas C, Ruchholtz S, Wafaisade A, Kauther MD, Lendemans S. Prehospital intubation of the moderately injured patient: a cause of morbidity? A matched-pairs analysis of 1,200 patients from the DGU Trauma Registry. Crit Care. 2011;15(5):R207.
Halford FJ. A critique of intravenous anesthesia in war surgery. Anesthesiology. 1943;4:67–9.
Chou D, Harada MY, Barmparas G, Ko A, Ley EJ, Margulies DR, Alban RF. Field intubation in civilian patients with hemorrhagic shock is associated with higher mortality. J Trauma Acute Care Surg. 2016;80(2):278–82.
Fevang E, Perkins Z, Lockey D, Jeppesen E, Lossius HM. A systematic review and meta-analysis comparing mortality in pre-hospital tracheal intubation to emergency department intubation in trauma patients. Crit Care. 2017;21(1):192.
Green RS, Butler MB, Erdogan M. Increased mortality in trauma patients who develop post-intubation hypotension. J Trauma Acute Care Surg. 2017;83:569.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Hudson, T. (2020). Airway Management of Patients with Life Threatening Haemorrhage: Principles of Safe and Effective Care. In: Spinella, P. (eds) Damage Control Resuscitation. Springer, Cham. https://doi.org/10.1007/978-3-030-20820-2_14
Download citation
DOI: https://doi.org/10.1007/978-3-030-20820-2_14
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-20819-6
Online ISBN: 978-3-030-20820-2
eBook Packages: MedicineMedicine (R0)