COVID-19–Related Fatalities and Intensive-Care-Unit Admissions by Age Groups in Europe: A Meta-Analysis
- 1Université de Paris, Centre of Research in Epidemiology and Statistics-CRESS, INSERM, Paris, France
- 2Department of General Pediatrics and Pediatric Infectious Diseases, AP-HP, Necker Hospital for Sick Children, Université de Paris, Paris, France
- 3Department of Respiratory Medicine, Amsterdam University Medical Center, University of Amsterdam, Amsterdam, Netherlands
Objectives: Precise international estimates of the age breakdown of COVID-19–related deaths and intensive-care-unit (ICU) admissions are lacking. We evaluated the distribution of COVID-19–related fatalities and ICU admissions by age groups in Europe.
Materials and methods: On April 6, 2020, we systematically reviewed official COVID-19–related data from 32 European countries. We included countries that provided data regarding more than 10 COVID-19–related deaths stratified by age according to pre-specified age groups (i.e., <40, 40–69, ≥70 years). We used random-effects meta-analysis to summarize the data.
Results: Thirteen European countries were included in the review, for a total of 31,864 COVID-19–related deaths (range: 27–14,381 per country). In the main meta-analysis (including data from Germany, Hungary, Italy, The Netherlands, Portugal, Spain, Switzerland; 21,522 COVID-19–related fatalities), the summary proportions of individuals <40, 40–69, and ≥70 years old among all COVID-19–related deaths were 0.1% (0.0–0.2; I2 28.6%), 13.0% (10.8–15.4; I2 91.5%), and 86.6% (84.2–88.9; I2 91.5%), respectively. ICU data were available for four countries (France, Greece, Spain, Sweden). The summary proportions of individuals around <40–50, around 40–69, and around ≥60–70 years old among all COVID-19–related ICU admissions were 5.4% (3.4–7.8; I2 89.0%), 52.6% (41.8–63.3; I2 98.1%), and 41.8% (32.0–51.9; I2 99%), respectively.
Conclusions: People under 40 years old represent a small fraction of most severe COVID-19 cases in Europe. These results may help health authorities respond to public concerns and guide future physical distancing and mitigation strategies. Specific measures to protect older people should be considered.
Introduction
As of April 6, 2020, more than 1,000,000 confirmed cases and 65,000 deaths due to coronavirus disease 2019 (COVID-19) have been reported globally (1). Data from China and Italy have indicated that older adults are at higher risk of dying from COVID-19 than are younger people (2–4). However, most studies have emphasized the case-fatality rate (4–6) (i.e., the conditional probability of death among classified COVID-19 cases). This indicator is likely to be biased in the early phase of an outbreak, mostly because of preferential testing of people with more severe disease (e.g., hospitalized patients) and delays between the time of death and its official registration (7).
Despite a growing sense that SARS-CoV-2 can result in severe disease regardless of age (8), precise estimates of the age breakdown of COVID-19–related deaths and intensive-care-unit (ICU) admissions are lacking. Here we evaluated the distribution of COVID-19–related fatalities and ICU admissions by age in Europe. Such an analysis is critical to direct any potential relaxation of physical distancing and mitigation measures, which have been highly effective in reducing the number of cases but have severe economic and social consequences (9). We hypothesized that people <40 years old represent a small fraction of most severe COVID-19 cases, as suggested by early reports from the Chinese Centers for Disease Control and Prevention (2).
Materials and Methods
On April 6, 2020, one of the authors (JFC) systematically reviewed and extracted COVID-19–related mortality data from all 32 European countries participating in the European Center for Disease Prevention and Control surveillance network (i.e., European Union/European Economic Area and the United Kingdom), by collating official reports provided by local Public Health or Ministry of Health websites (Supplementary Table 1). We included countries if they provided data for more than 10 COVID-19–related deaths stratified by age according to pre-specified groups (i.e., <40, 40–69, ≥70 years old). For the included countries, we also extracted data regarding ICU admissions by age groups. A second author (DAK) verified study selection and data extraction, and disagreements were discussed to achieve consensus. We applied no language restrictions.
We used random-effects meta-analysis with Freeman-Tukey double arcsine transformation and exact confidence intervals (CIs) to estimate the proportion of age groups (<40, 40–69, ≥70 years old) among all COVID-19–related fatalities. We excluded participants with missing data for age. For mortality data, we conducted a sensitivity analysis that also included countries reporting data using slightly different age groups, with the following inclusion criteria: (1) the cutoff to define the “younger” age group was within 40–50 years and (2) the “intermediate” age group covered at least 20 years (e.g., United Kingdom, <40, 40–59, ≥60 years). We used the same age criteria to evaluate the distribution of age groups among COVID-related ICU admissions. Heterogeneity was quantified with the I2 statistic. Statistical analyses involved use of Stata 15/SE (Stata Corp., College Station, TX, USA).
Results
Descriptive Data
We identified official reports of COVID-19–related mortality data for all European countries except Cyprus. Eighteen countries (accounting for 1,113 deaths) were excluded because of unusable data: 11 were excluded because of lack of age breakdown of COVID-19 deaths, 5 because of fewer than 10 fatalities, and 2 because of age cutoffs not matching our pre-defined groups (Supplementary Table 1). Thirteen European countries were included in the review, for a total of 31,864 COVID-19–related deaths (range 27–14,381 per country; Table 1) (10–22).
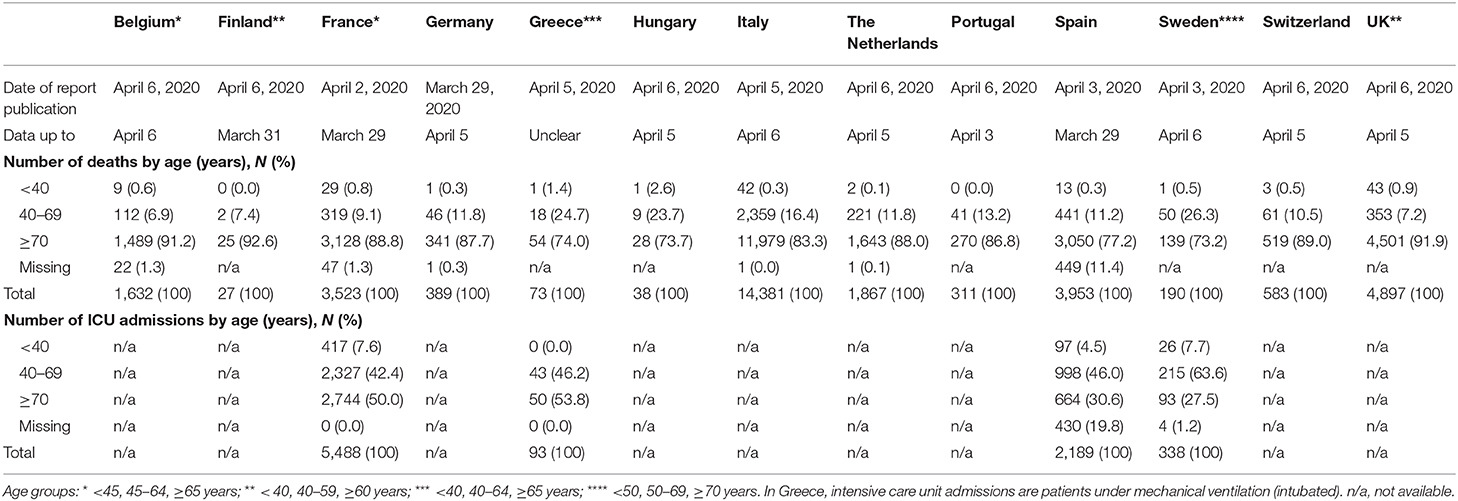
Table 1. COVID-19–related fatalities and intensive-care-unit (ICU) admissions by age groups in Europe (as of April 6, 2020).
COVID-19–Related Fatalities by Age Groups
In the main meta-analysis (7 countries; 21,522 COVID-19–related fatalities), the summary proportions of individuals <40, 40–69, and ≥70 years old among all COVID-19–related deaths were 0.1% (0.0–0.2; I2 28.6%), 13.0% (10.8–15.4; I2 91.5%), and 86.6% (84.2–88.9; I2 91.5%), respectively (Figure 1). In a sensitivity analysis also including countries that reported slightly different age groups (13 countries; 31,864 COVID-19–related deaths), the summary proportions of individuals around <40–50, around 40–69, and around ≥60–70 years old among all COVID-19–related deaths were 0.2% (0.1–0.4; I2 74.6%), 12.7% (10.0–15.7; I2 97.4%), and 86.8% (84.0–89.4; I2 97.1%), respectively (Supplementary Figure 2).
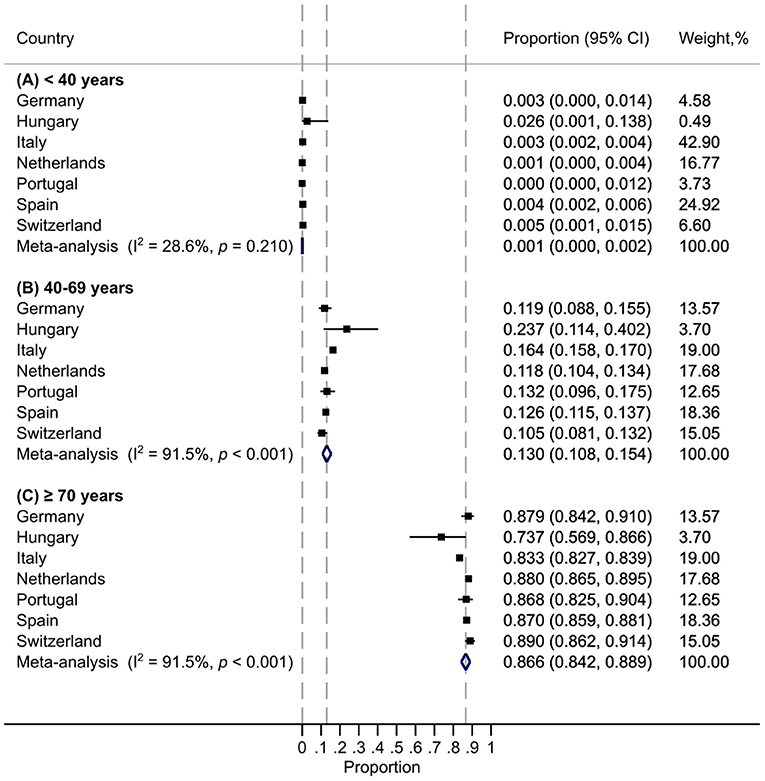
Figure 1. Distribution of age groups for all COVID-19–related deaths in Europe: meta-analysis. Each vertical dashed line is aligned with the meta-analysis summary estimate of the corresponding age group.
COVID-19–Related ICU Admissions by Age Groups
The meta-analysis of ICU admissions included data from 4 countries (8,088 COVID-19–related ICU admissions). The summary proportions of individuals around <40–50, around 40–69, and around ≥60–70 years old among all COVID-19–related ICU admissions were 5.4% (3.4–7.8; I2 89.0%), 52.6% (41.8–63.3; I2 98.1%), and 41.8% (32.0–51.9; I2 99%), respectively (Table 1 and Supplementary Figure 3).
Discussion
This report describes the current distribution of COVID-19–related deaths and ICU admissions in Europe across age groups, using official reports from 13 countries. These data represent about half of the total of COVID-19–related deaths reported worldwide as of April 6, 2020 (1). Individuals <40 years old represented about 0.1 and 5% of COVID-19–related deaths and ICU admissions, respectively, whereas those >70 years old represented about 85 and 40%, respectively.
The distribution of COVID-19–related deaths by age in Europe differs from what was observed in the early phase of the pandemic in mainland China (as of February 11, 2020: <40, 40–69, ≥70 years old, representing 2.5, 46.6, and 50.8% of 1,023 COVID-19–related deaths, respectively) (4) and what is currently observed in the United States (as of April 7: <45, 45–64, ≥65 years old, representing 3.3, 17.6, and 79.0% of 2,214 COVID-19–related deaths, respectively) (23). This observation could reflect different patterns of patient characteristics, underlying risk factors, and management across settings as well as variability in the organization of healthcare and identification of causes of death across countries (24, 25). The age structure of each population might also be key: in 2019, Italy had the highest proportion of people aged ≥80 years in Europe (7.2%), whereas in the United States, for example, this proportion was as low as 3.6% in 2010 (26). However, the overall prevalence of obesity (body mass index ≥ 30 kg/m2), reported as a risk factor for severe COVID-19, is much higher in the United States than Italy (42.4 vs. 10.5%) (27).
Our study has limitations. First, we could not include all European countries, mainly because official reports on COVID-19–related mortality data by age group were not always available. Second, we could not investigate the potential burden of underlying health conditions and other risk factors such as obesity and diabetes because this information was rarely reported. Third, we investigated COVID-19–related mortality data, but we acknowledge that methods for case ascertainment, case definitions, and SARS-CoV-2 RT-PCR testing strategies varied across countries. Some countries, such as France, provided detailed information for only in-hospital fatalities at the time of the study, which does not account for COVID-related deaths that occurred in other settings such as nursing homes (28), for a potential overrepresentation of younger patients. The definition of ICU cases also varied across countries, and Greece only reported the number of intubated patients.
Physical distancing is currently recommended in many countries for all age groups to slow the spread of COVID-19 and protect older people and, more broadly, the healthcare system. People <40 years old represent a small fraction of the total number of most severe COVID-19 cases in Europe. These results, together with evaluations of the impact of comorbidities and risk factors in the course of COVID-19, may help health authorities respond to public concerns and guide future physical distancing and mitigation strategies. Relaxed physical distancing measures could be considered in people under 40 years of age, but specific measures aiming at protecting older people should be developed (29).
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Materials, further inquiries can be directed to the corresponding author/s.
Ethics Statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent from the participants' legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author Contributions
JC, MC, and JT: conceptualization. JC and JT: methodology. JC: statistical analysis. JC and DK: data extraction and management. JC and JT: writing—original draft preparation. JC, DK, SM, SA, MC, and JT: writing—review and editing. MC and JT: supervision. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We thank Prof. Richard Malley (Boston Children's Hospital, USA) and Prof. Henrique Barros (Institute of Public Health, University of Porto, Portugal) for their valuable feedback on the manuscript.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2020.560685/full#supplementary-material
References
1. WHO. Coronavirus Disease 2019 (COVID-19) Situation Report-77. Geneva: World Health Organization (2020).
2. Novel Coronavirus Pneumonia Emergency Response Epidemiology Team. Vital Surveillances: the epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19)-China, 2020. China CDC Wkly. (2020) 2:113–22. doi: 10.46234/ccdcw2020.032
3. Sorbello M, El-Boghdadly K, Di Giacinto I, Cataldo R, Esposito C, Falcetta S, et al. The Italian coronavirus disease 2019 outbreak: recommendations from clinical practice. Anaesthesia. (2020) 75:724–32. doi: 10.1111/anae.15049
4. Onder G, Rezza G, Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA. (2020) 323:1775–6. doi: 10.1001/jama.2020.4683
5. Verity R, Okell LC, Dorigatti I, Winskill P, Whittaker C, Imai N, et al. Estimates of the severity of coronavirus disease 2019: a model-based analysis. Lancet Infect Dis. (2020) 20:669–77. doi: 10.1016/S1473-3099(20)30243-7
6. Baud D, Qi X, Nielsen-Saines K, Musso D, Pomar L, Favre G. Real estimates of mortality following COVID-19 infection. Lancet Infect Dis. (2020) 20:773. doi: 10.1016/S1473-3099(20)30195-X
7. Lipsitch M, Donnelly CA, Fraser C, Blake IM, Cori A, Dorigatti I, et al. Potential biases in estimating absolute and relative case-fatality risks during outbreaks. PLoS Negl Trop Dis. (2015) 9:e0003846. doi: 10.1371/journal.pntd.0003846
8. Severe outcomes among patients with coronavirus disease 2019 (COVID-19) - United States, February 12-March 16 2020. MMWR Morb Mortal Wkly Rep. (2020) 69:343–6. doi: 10.15585/mmwr.mm6912e2
9. Anderson RM, Heesterbeek H, Klinkenberg D, Hollingsworth TD. How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet. (2020) 395:931–4. doi: 10.1016/S0140-6736(20)30567-5
10. Belgian Institute for Health (2020). Available online at: http://epidemio.wiv-isp.be/ID/Pages/2019-nCoV_epidemiological_situation.aspx (accessed April 6, 2020).
11. Finnish Institute for Health and Welfare (2020). Available online at: http://thl.fi/fi/web/infektiotaudit-ja-rokotukset/ajankohtaista/ajankohtaista-koronaviruksesta-covid-19/tilannekatsaus-koronaviruksesta (accessed April 6, 2020).
12. French Public Health Agency (2020). Available online at: http://www.santepubliquefrance.fr/maladies-et-traumatismes/maladies-et-infections-respiratoires/infection-a-coronavirus/articles/infection-au-nouveau-coronavirus-sars-cov-2-covid-19-france-et-monde (accessed April 6, 2020).
13. Robert Koch Institute (2020). Available online at: http://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/nCoV.html (accessed April 6, 2020).
14. Greek National Public Health Organization (2020). Available online at: http://eody.gov.gr/neos-koronaios-covid-19/ (accessed April 6, 2020).
15. Hungarian National Center for Public Health (2020). Available online at: http://koronavirus.gov.hu/ (accessed April 6, 2020).
16. Italian Higher Institute of Health (2020). Available online at: http://www.epicentro.iss.it/coronavirus/ (accessed April 6, 2020).
17. Dutch National Institute for Public Health and the Environment (2020). Available online at: https://www.rivm.nl/coronavirus-covid-19/actueel (accessed April 6, 2020).
18. Portuguese Directorate-General of Health (2020). Available online at: http://covid19.min-saude.pt/relatorio-de-situacao/ (accessed April 6, 2020).
19. Spanish Institute of Health Carlos III (2020). Available online at: http://www.isciii.es/QueHacemos/Servicios/VigilanciaSaludPublicaRENAVE/EnfermedadesTransmisibles/Paginas/InformesCOVID-19.aspx (accessed April 6, 2020).
20. Public Health Agency of Sweden (2020). Available online at: http://www.folkhalsomyndigheten.se/folkhalsorapportering-statistik/statistik-a-o/sjukdomsstatistik/covid-19-veckorapporter/senaste-covidrapporten/ (accessed April 6, 2020).
21. Swiss Federal Office of Public Health (2020). Available online at: http://www.bag.admin.ch/bag/fr/home/krankheiten/ausbrueche-epidemien-pandemien/aktuelle-ausbrueche-epidemien/novel-cov/situation-schweiz-und-international.html#1164290551 (accessed April 6, 2020).
22. National Health Service England (2020). Available from: http://www.england.nhs.uk/statistics/statistical-work-areas/covid-19-daily-deaths/ (accessed April 6, 2020).
23. Provisional Death Counts for Coronavirus Disease (COVID-19). Available online at: https://www.cdc.gov/nchs/nvss/vsrr/COVID19/index.htm (accessed April 6, 2020).
24. Fang FC, Benson CA, Del Rio C, Edwards KM, Fowler VG Jr, Fredricks DN, et al. COVID-19 - lessons learned and questions remaining. Clin Infect Dis. (2020). doi: 10.1093/cid/ciaa1654. [Epub ahead of print].
25. Sorci G, Faivre B, Morand S. Explaining among-country variation in COVID-19 case fatality rate. Sci Rep. (2020) 10:18909. doi: 10.1038/s41598-020-75848-2
26. Howden L, Meyer J. Age and Sex Composition in the United States: 2010 Census Brief (2011). Available online at: https://www.census.gov/library/publications/2011/dec/c2010br-03.html (accessed April 6, 2020).
27. Hales C, Carroll M, Fryar C, Ogden C. Prevalence of Obesity and Severe Obesity Among Adults: United States, 2017-2018. Hyattsville, MD: National Center for Health Statistics (2020).
28. ECDC Public Health Emergency Team Danis K Fonteneau L Georges S Daniau C Bernard-Stoecklin S . High impact of COVID-19 in long-term care facilities, suggestion for monitoring in the EU/EEA, May 2020. Euro Surveill. (2020) 25:2000956. doi: 10.2807/1560-7917.ES.2020.25.22.2000956
Keywords: coronavirus, SARS-CoV-2, COVID-19, mortality, epidemiology, age, meta-analysis, intensive care unit
Citation: Cohen JF, Korevaar DA, Matczak S, Chalumeau M, Allali S and Toubiana J (2021) COVID-19–Related Fatalities and Intensive-Care-Unit Admissions by Age Groups in Europe: A Meta-Analysis. Front. Med. 7:560685. doi: 10.3389/fmed.2020.560685
Received: 12 May 2020; Accepted: 17 December 2020;
Published: 14 January 2021.
Edited by:
Ata Murat Kaynar, University of Pittsburgh, United StatesReviewed by:
Natalija Vukovic, University of Niš, SerbiaMassimiliano Sorbello, Gaspare Rodolico Hospital, Italy
Copyright © 2021 Cohen, Korevaar, Matczak, Chalumeau, Allali and Toubiana. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jérémie F. Cohen, jeremie.cohen@inserm.fr orcid.org/0000-0003-3572-8985
 Jérémie F. Cohen
Jérémie F. Cohen Daniël A. Korevaar3
Daniël A. Korevaar3  Julie Toubiana
Julie Toubiana