Abstract
Background Many older individuals suffer from difficulty initiating and maintaining sleep, and consequently use hypnosedative medication. The use of sleeping tablets, usually benzodiazepines (BZs) and the newer Z drugs such as zolpidem, is largely unnecessary and problematic since their efficacy is not maintained over an extended period of time and they increase the risk of falls. Withdrawing these medications is challenging because of their propensity for causing dependence and rebound insomnia.
Objectives To describe the use of anxiolytic and hypnosedative medications by patients attending a falls clinic, determine the success of recommendations to cease or reduce use of these medications, and evaluate patient characteristics influencing the success of these recommendations.
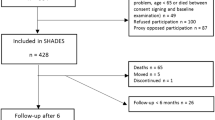
Methods Patients with a first appointment at an Australian falls clinic between January 2006 and December 2008 were identified from letters written by the geriatrician or rehabilitation physician who ran the clinic. Patients who were taking a BZ/Z drug, had attended a follow-up appointment at least 2 months after their index appointment and had received a documented recommendation to alter their BZ/Z drug use at the index appointment were included in this study. The associations between compliance with the specialist physician’s recommendation to alter the BZ/Z drug and BZ/Z drug dose, frequency and duration, patient’s age, sex, residence, co-morbidities and number of regular medications were assessed. Inter-clinician variation in the proportion of patients receiving a follow-up appointment, recording of BZ/Z drug use and the proportion of patients given a recommendation to alter BZ/Z drug use were also analysed in the broader population of all patients receiving a first appointment at the falls clinic in the study period.
Results Data from 302 patient records revealed that 21.5% of patients were using a BZ/Z drug and 27.8% were using any drug for its hypnosedative properties. Over the 3-year study period there was a reduction in BZ use, which was countered by an increase in the use of zolpidem, so that the overall use of BZ/Z drugs did not change. Of those patients taking a BZ/Z drug, 48% (31/65) were followed up and had a documented recommendation to alter their BZ/Z drug use. At least 68% (21/31) of these patients were compliant at follow-up. Patients who were assessed by a geriatrician were more likely to be advised to alter their BZ use than those assessed by a rehabilitation specialist (p = 0.002). Patients were more likely to be compliant if they were given a recommendation to cease their BZ/Z drug compared with advice to reduce the dose or to gradually reduce the dose with the aim of cessation (p = 0.019). There were no sex- or age-specific differences in compliance. Patients who were successful in ceasing or reducing BZ/Z drug use showed nonsignificant trends toward having a reduced number of co-morbidities and regular medications, and lower frequency of use of BZ/Z drugs.
Results We observed a constant proportion of falls clinic patients taking BZs or Z drugs between 2006 and 2008. Specialist recommendation to cease or reduce dosage of these medications was associated with a high success rate.




Similar content being viewed by others
References
Windle A, Elliot E, Duszynski K, et al. Benzodiazepine prescribing in elderly Australian general practice patients. Aust N Z J Public Health 2007; 31(4): 379–81
Morin CM, Colecchi C, Stone J, et al. Behavioral and pharmacological therapies for late-life insomnia: a randomized controlled trial. JAMA 1999; 281(11): 991–9
Hilmer SN, McLachlan AJ, Couteur DGL. Clinical pharmacology in the geriatric patient. Fundam Clin Pharmacol 2007; 21(3): 217–30
Heberlein A, Bleich S, Kornhuber J, et al. Neuroendocrine pathways in benzodiazepine dependence: new targets for research and therapy. Hum Psychopharmacol 2008; 23(3): 171–81
Hajak G, Müller WE, Wittchen HU, et al. Abuse and dependence potential for the non-benzodiazepine hypnotics zolpidem and zopiclone: a review of case reports and epidemiological data. Addiction 2003; 98(10): 1371–8
Curran HV, Collins R, Fletcher S, et al. Older adults and withdrawal from benzodiazepine hypnotics in general practice: effects on cognitive function, sleep, mood and quality of life. Psychol Med 2003; 33: 1223–37
Salzman C, Fisher J, Nobel K, et al. Cognitive improvement following benzodiazepine discontinuation in elderly nursing home residents. Int J Geriatr Psychiatry 1992; 7(2): 89–93
Iyer S, Naganathan V, McLachlan AJ, et al. Medication withdrawal trials in people aged 65 years and older: a systematic review. Drugs Aging 2008; 25(12): 1021–31
Wright RM, Roumani YF, Boudreau R, et al. Effect of central nervous system medication use on decline in cognition in community-dwelling older adults: findings from the Health, Aging and Body Composition study. J Am Geriatr Soc 2009; 57(2): 243–50
Glass J, Lanctot KL, Herrmann N, et al. Sedative hypnotics in older people with insomnia: meta-analysis of risks and benefits. BMJ 2005; 331(7526): 1169–75
Clements RM. Reducing psychotropic medications in elderly rehabilitation inpatients with a fall-related admission: how often is it happening? Geriatr Gerontol Int 2008; 8(3): 139–42
Hartikainen S, Klaukka T. Use of psychotropics is high among very old people. Eur J Clin Pharmacol 2004; 59(11): 849–50
Tinetti ME. Preventing falls in elderly persons. N Engl J Med 2003; 348(1): 42–9
Nevitt MC, Cummings SR, Kidd S, et al. Risk factors for recurrent nonsyncopal falls: a prospective study. JAMA 1989; 261(18): 2663–8
Thapa PB, Gideon P, Fought RL, et al. Psychotropic drugs and risk of recurrent falls in ambulatory nursing home residents. Am J Epidemiol 1995; 142(2): 202–11
Hanlon JT, Boudreau RM, Roumani YF, et al. Number and dosage of central nervous system medications on recurrent falls in community elders: the Health, Aging and Body Composition study. J Gerontol A Biol Sci Med Sci 2009; 64A(4): 492–8
Campbell AJ, Robertson MC, Gardner MM, et al. Psychotropic medication withdrawal and a home-based exercise program to prevent falls: a randomized, controlled trial. J Am Geriatr Soc 1999; 47(7): 850–3
Brodie MJ, Kwan P. Epilepsy in elderly people. BMJ 2005; 331(7528): 1317–22
Pulska T, Pahkala K, Laippala P, et al. Follow up study of longstanding depression as predictor of mortality in elderly people living in the community. BMJ 1999; 318(7181): 432–3
Noel PH, Williams Jr JW, Unutzer J, et al. Depression and comorbid illness in elderly primary care patients: impact on multiple domains of health status and well-being. Ann Fam Med 2004; 2(6): 555–62
Tu K, Mamdani MM, Hux JE, et al. Progressive trends in the prevalence of benzodiazepine prescribing in older people in Ontario, Canada. J Am Geriatr Soc 2001; 49(10): 1341–5
Kennedy GA, Bruck D. Australasian Sleep Association, NSW central west division of general practice GP mental health supplement: sleep disorders [online]. Available from URL: http://www.sleepaus.on.net/kennedybrucksleepdisordersforgps.pdf/ [Accessed 2010 Jul 7]
Jorm AF, Grayson D, Creasey H, et al. Long-term benzodiazepine use by elderly people living in the community. Aust N Z J Public Health 2000; 24(1): 7–10
Hill KD, Moore KJ, Dorevitch MI, et al. Effectiveness of falls clinics: an evaluation of outcomes and client adherence to recommended interventions. J Am Geriatr Soc 2008; 56(4): 600–8
Hoffmann F, Scharffetter W, Glaeske G. Verbrauch von Zolpidem und Zopiclon auf Privatrezepten zwischen 1993 und 2007. Nervenarzt 2009; 80(5): 578–83
Parr JM, Kavanagh DJ, Cahill L, et al. Effectiveness of current treatment approaches for benzodiazepine discontinuation: a meta-analysis. Addiction 2009; 104(1): 13–24
Salonoja M, Salminen M, Aarnio P, et al. One-time counselling decreases the use of benzodiazepines and related drugs among community-dwelling older persons. Age Ageing 2010; 39(3): 313–9
Tulner LR, Kuper IMJA, Frankfort SV, et al. Discrepancies in reported drug use in geriatric outpatients: relevance to adverse events and drug-drug interactions. Am J Geriatr Pharmacother 2009; 7(2): 93–104
Acknowledgements
No sources of funding were used to conduct this study or prepare this manuscript. The authors have no conflicts of interest that are directly relevant to the content of this study. The authors would like to acknowledge the support of the Geoff and Elaine Penney Ageing Research Unit, RNSH. The authors would also like to thank the administration and clinic staff in the Department of Aged Care and Rehabilitation at RNSH and Dr Mark Haran for their assistance with data collection.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Joester, J., Vogler, C.M., Chang, K. et al. Hypnosedative Use and Predictors of Successful Withdrawal in New Patients Attending a Falls Clinic. Drugs Aging 27, 915–924 (2010). https://doi.org/10.2165/11584480-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11584480-000000000-00000