Abstract
Introduction and objective
Geriatric patients with multiple comorbidities are at high risk of experiencing an adverse drug reaction (ADR) during hospitalisation. The aim of the study was to compare the rate of ADRs as predicted by a computerised pharmacological database to the actual rate determined by direct observation in a sample of geriatric patients.
Study design
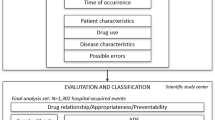
During a 4-month period, geriatric patients were monitored using prospective observation. Patients were intensively screened for ADRs by a pharmacoepidemiological team (PET), consisting of two pharmacists and a physician. Actual ADRs detected by the PET were compared with those predicted by a computerised drug database. Furthermore, the set of actual ADRs, which resulted from drug-drug interactions (DDIs), were contrasted with potential DDIs signalled by the database. The main outcome measures were the incidence of actual ADRs. For the detection rate of the database we focused on frequent ADRs (>1% according to product information and database) and all DDIs indicated automatically by the database.
Results
163 patients (121 female), mean age 79.8 ± 7.1 years (range 60–98), were included in the study which was conducted on a geriatric rehabilitation hospital ward. The mean duration of hospitalisation was 24.3 ± 8.4 days. Elderly patients received an average of 14.0 drugs (range 2–35) during their hospital stay.
Of all patients, 60.7% experienced at least one ADR. The PET detected a total of 153 ADRs, with a mean of 0.9 ADRs per patient (range 0–5). The computerised drug database predicted an average of 309 potential ADRs for each patient; however, only 21 ADRs per patient were of high frequency. In 48% of ADR-positive patients (defined by PET) at least one of these frequent ADRs occurred.
DDIs were detected by the PET in 14.7% of patients. Our database indicated a mean of 12 potential DDIs per patient. In 14 out of 24 DDI-positive patients, at least one signal indicated a real DDI. The database sensitivity was consequently 58.3%.
Conclusion
In geriatric patients the incidence of ADRs is high. Computerised drug databases are a useful tool for detecting and avoiding ADRs. Our software, however, also produced a large number of signals that did not relate to actual ADRs found by the PET. The sheer number of these ‘false’ signals shows the need for refinement and optimisation of databases for daily clinical use.






Similar content being viewed by others
References
Leape LL, Brennan TA, Laird N, et al. The nature of adverse events in hospitalized patients: results of the Harvard Medical Practice Study II. N Engl J Med 1991; 324(6): 377–84
Bates DW, Leape LL, Petrycki S. Incidence and preventability of adverse drug events in hospitalized adults. J Gen Intern Med 1993; 8(6): 289–94
Lazarou J, Pomeranz BH, Corey PN. Incidence of adverse drug reactions in hospitalized patients: a meta-analysis of prospective studies. JAMA 1998; 279(15): 1200–5
Atkin PA, Veitch PC, Veitch EM, et al. The epidemiology of serious adverse drug reactions among the elderly. Drugs Aging 1999; 14(2): 141–52
Beyth RJ, Shorr RI. Epidemiology of adverse drug reactions in the elderly by drug class. Drugs Aging 1999; 14(3): 231–9
Classen DC, Pestotnik SL, Evans RS, et al. Adverse drug events in hospitalized patients: excess length of stay, extra costs, and attributable mortality. JAMA 1997; 277(4): 301–6
Bates DW, Spell N, Cullen DJ, et al. The costs of adverse drug events in hospitalized patients: Adverse Drug Events Prevention Study Group. JAMA 1997; 277(4): 307–11
Bates DW, Teich JM, Lee J, et al. The impact of computerized physician order entry on medication error prevention. J Am Med Inform Assoc 1999; 6(4): 313–21
Jha AK, Kuperman GJ, Teich JM, et al. Identifying adverse drug events: development of a computer-based monitor and comparison with chart review and stimulated voluntary report. J Am Med Inform Assoc 1998; 5(3): 305–14
Dormann H, Muth-Selbach U, Krebs S, et al. Incidence and costs of adverse drug reactions during hospitalisation: computerised monitoring versus stimulated spontaneous reporting. Drug Saf 2000; 22(2): 161–8
Azaz-Livshits T, Levy M, Sadan B, et al. Computerized survelliance of adverse drug reactions in hospital: pilot study. Br J Clin Pharmacol 1998; 45(3): 309–14
Langdorf MI, Fox JC, Marwah RS, et al. Physician versus computer knowledge of potential drug interactions in the emergency department. Acad Emerg Med 2000; 7(11): 1321–9
Del Fiol G, Rocha BH, Kuperman GJ, et al. Comparison of two knowledge bases on the detection of drug-drug interactions. Proc AMIA Symp 2000, 171–5
Goldberg RM, Mabee J, Mammone M, et al. A comparison of drug interaction software programs: applicability to the emergency department. Ann Emerg Med 1994; 24(4): 619–25
Jankel CA, Martin BC. Evaluation of six computerized drug interaction screening programs. Am J Hosp Pharm 1992; 49(6): 1430–5
Bates DW, Leape LL, Cullen DJ, et al. Effect of computerized physician order entry and a team intervention on prevention of serious medication errors. JAMA 1998; 280(15): 1311–6
Raschke RA, Gollihare B, Wunderlich TA, et al. A computer alert system to prevent injury from adverse drug events: development and evaluation in a community teaching hospital [published erratum appears in JAMA 1999 Feb 3; 281 (5): 420]. JAMA 1998; 280(15): 1317–20
Fricke U, Günther J. Anatomisch-therapeutisch-chemische Klassifikation mit Tagesdosen für den deutschen Arzneimittelmarkt. 2002
WHO. International statistical classification of diseases and related health problems. 10th rev ed. Geneva: WHO, 1992
Edward IR, Aronson JK. Adverse drug reactions: definitions, diagnosis and management. Lancet 2000; 356(9237): 1255–9
Naranjo CA, Busto U, Sellers EM, et al. A method for estimating the probability of adverse drug reactions. Clin Pharmacol Ther 1981; 30(2): 239–45
Rieder MJ. Mechanisms of unpredictable adverse drug reactions. Drug Saf 1994; 11(3): 196–212
Schumock GT, Thornton JP. Focusing on the preventability of adverse drug reactions [letter]. Hosp Pharm 1992; 27(6): 538
Hanlon JT, Schmader KE, Koronkowski MJ, et al. Adverse drug events in high risk older outpatients. J Am Geriatr Soc1997; 45(8): 945–8
Bates DW. Drugs and adverse drug reactions: how worried should we be? JAMA 1998; 279(15): 1216–7
Gurwitz JH, Avorn J. Old age: is it a risk for adverse drug reactions? Agents Actions Suppl 1990; 29: 13–25
Dormann H, Criegee-Rieck M, Neubert A, et al. Lack of awareness of community-acquired adverse drug reactions upon hospital admission: dimensions and consequences of a dilemma. Drug Saf 2003; 26(5): 353–62
Acknowledgements
This study was supported by grants from Bundesministerium für Bildung und Forschung (BMBF) 01EC940317, BMBF 08NM061D and German Israeli Fundation No. G 690221.912000, health initiative “Bayern Aktiv” No 3.8/8600. The authors have provided no information on conflicts of interest directly relevant to the content of this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Egger, T., Dormann, H., Ahne, G. et al. Identification of Adverse Drug Reactions in Geriatric Inpatients Using a Computerised Drug Database. Drugs Aging 20, 769–776 (2003). https://doi.org/10.2165/00002512-200320100-00005
Published:
Issue Date:
DOI: https://doi.org/10.2165/00002512-200320100-00005