-
PDF
- Split View
-
Views
-
Cite
Cite
H. B. Menz, A. Tiedemann, M. M. S. Kwan, K. Plumb, S. R. Lord, Foot pain in community-dwelling older people: an evaluation of the Manchester Foot Pain and Disability Index, Rheumatology, Volume 45, Issue 7, July 2006, Pages 863–867, https://doi.org/10.1093/rheumatology/kel002
Close - Share Icon Share
Abstract
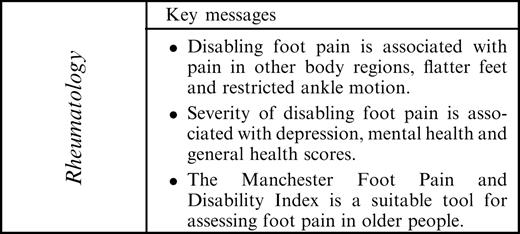
Objectives. The objectives of this study were (i) to examine the psychometric properties of the Manchester Foot Pain and Disability Index (MFPDI) in community-dwelling older people, and (ii) to determine the correlates of disabling foot pain in this age-group.
Methods. A questionnaire consisting of medical history, the MFPDI, the Goldberg Anxiety and Depression Scale (GADS) and the Medical Outcomes Study Short Form 36 (SF-36) was administered to a sample of 301 community-dwelling people (117 men, 184 women) aged between 70 and 95 yr (mean 77.2, s.d. 4.9), who also underwent a clinical assessment of foot problems.
Results. Using the MFPDI case definition, 108 people (36%) were found to have disabling foot pain. Within this subgroup, the MFPDI had high internal consistency (Cronbach's α=0.89). Principal components analysis revealed a four-factor structure representing the constructs of functional limitation, pain intensity, concern about appearance, and activity restriction, which explained 62% of the variance in the original items. Participants with disabling foot pain were more likely to report pain in the back, hips, knees and hands or wrists, and exhibited flatter feet and less range of motion in the ankle joint. The MFPDI and its subscales were significantly associated with scores on the GADS depression subscale and the general health and mental health components of the SF-36.
Conclusions. These findings confirm the high prevalence of disabling foot pain in older people, and suggest that the MFPDI is a suitable tool for assessing foot pain in this population.
Foot pain affects between 20 and 30% of community-dwelling older people [1–4] and is associated with decreased ability to perform activities of daily living [5, 6], problems with balance and gait [7–9] and increased risk of falls [10]. A wide range of factors have been associated with foot pain in older people, including intrinsic foot conditions (such as hallux valgus, toe deformity, corns and calluses [1, 11]), extrinsic factors (such as ill-fitting footwear [12]) and systemic conditions such as obesity [13] and generalized osteoarthritis [7, 13]. These findings indicate that the development of foot symptoms in older people is multifactorial.
Research into foot pain in older people, however, has been hampered by the lack of a clear definition of what constitutes a foot problem and the absence of validated scales of foot pain and impairment. Foot impairment has generally been documented as a dichotomous variable, usually based on the subject's response to the question ‘Do you have problems with your feet?’. In response to these limitations, Garrow et al. [14] developed the Manchester Foot Pain and Disability Index (MFPDI). The MFPDI consists of 19 statements prefaced by the phrase ‘Because of pain in my feet’, formalized under three constructs: functional limitation (10 items), pain intensity (five items) and personal appearance (two items). The remaining two items are concerned with difficulties in performing work or leisure activities, which are omitted if the respondent is of retirement age. To validate the instrument, the MFPDI was tested on 45 rheumatology patients, 33 patients attending general practitioners for a foot-related problem, and 223 responders to a population survey of foot disorders. The instrument was found to have high internal consistency and construct validity, and has since been used in a population survey of foot problems [15] and as an outcome measure in a clinical trial [16].
One of the limitations of the MFPDI is that the validation process involved mostly middle-aged people, so there is some question as to the validity of the tool in an older population. Pain has a greater impact on psychological, social and physical function in older people [17, 18], so pain scales validated in younger people cannot be assumed to be equally valid in older people [18]. Therefore, the aims of this study were: (i) to examine the internal consistency and component structure of the MFPDI in a random sample of community-dwelling older people; and (ii) to determine the correlates of disabling foot pain in this age-group using both the case definition proposed by Garrow et al. [14] and the MFPDI subscales.
Methods
Participants
The study population comprised men and women aged 70 yr and over living in private households in the eastern suburbs metropolitan area of Sydney, New South Wales, Australia. These people were randomly drawn from the state electoral roll and initially contacted by letter and asked to participate in the study. Individuals were then contacted by telephone (or in person for those who did not have a telephone number) and invited to the Prince of Wales Medical Research Institute for assessment. Potential participants were excluded from the study if they had minimal English language skills, were blind, or had a Mini-Mental State Examination Score (MMSE) less than 24 [19]. Transport was provided for those who could not make their own way to the study site, in order to maximize the participation rates of older people with mobility limitations. Of the 1080 people initially contacted by letter and/or telephone, 329 (30.5%) agreed to participate and, of these, 301 (117 men, 184 women) aged 70–95 yr (mean = 77.2, s.d. = 4.9) met the inclusion criteria and underwent the assessments. The study was approved by the Human Ethics Committee, University of New South Wales, and informed consent was obtained from all participants.
When compared with data from the national census and health survey for Australians aged over 70 living at home, the study group differed as follows: a higher proportion (61.1 vs 56.5%) were female; a higher proportion (70.1 vs 46%) were aged 70–79 yr, a higher proportion (74.8 vs 66.7%) were Australian born and a higher proportion (41.9 vs 32.7%) were living alone.
Medical history questionnaire and demographic information
Age, medical history and pain location were determined by an interviewer-administered questionnaire. The medical history questionnaire required participants to select from a list of 15 common conditions, using the question ‘Do you have, or have you ever been told that you have any of the following conditions?’. Participants who reported pain were also requested to report the location of their pain. Height was then measured in metres, weight in kilograms, and body mass index (BMI) was calculated as body weight/height2.
Disabling foot pain was documented as a dichotomous variable, using the case definition proposed by Garrow et al. [14], which requires participants to have had current foot pain and pain in the last month, as well as recording at least one disability item on the MFPDI. A total MFPDI score was also calculated for those with disabling foot pain, using the following scoring system for each of the 17 items: none of the time (score = 0); some days (score = 1); on most days/every day (score = 2). The total MFPDI score therefore ranges from a minimum of 0 to a maximum possible score of 34. MFPDI subscale scores were also determined following the principal components analysis. The last two items on the MFPDI pertaining to difficulties with work or leisure activities were omitted as the sample group were of retirement age.
Depression was assessed using the Goldberg Anxiety and Depression Scale (GADS) [20]. The GADS comprises 18 closed questions divided into two subscales of nine items, which make it possible to calculate a depression score, an anxiety score and an overall score. General health was assessed using the Medical Outcomes Study Short Form 36 (SF-36) subscales, which have been validated for use in the Australian population [21].
Foot assessment
Arch height was assessed by measuring the height of the navicular tuberosity in millimetres while the subject was fully weight-bearing. This score was then corrected for differences in foot size by dividing it by the length of the foot [22]. Ankle flexibility was measured in degrees using a modified version of the weight-bearing lunge test. The lateral malleolus and head of the fibula were first located and marked with an ink pen. Participants then stood with their right foot placed alongside a vertically aligned clear acrylic plate inscribed with 2° protractor markings, and were instructed to take a comfortable step forward with the left leg. In this position, participants were instructed to bend their knees to squat down as low as possible, without lifting the right heel from the ground and while keeping the trunk upright. Participants leaned on a bench placed alongside them at waist height to support their body weight. The position of the fibular head was marked on the clear acrylic plate, and the angle formed between the lateral malleolus and the fibular head was measured. The test was completed three times, and the average score documented as the test result [23]. The presence and severity of hallux valgus (bunions) was determined using the Manchester Scale [24, 25]. This instrument consists of standardized photographs of feet with four degrees of hallux valgus: none (score = 0); mild (score = 1); moderate (score = 2); and severe (score = 3), which were matched to the subject's feet. An overall measure of hallux valgus severity was determined by summing the scores for right and left feet. The presence of lesser digital deformity (hammer toes and claw toes), corns and calluses was determined according to previously published criteria, and a sum of the total number of each of these abnormalities plus the Manchester Scale score for both feet was combined to provide an overall foot problem score. The reliability of navicular height, ankle flexibility and foot problem score measurements when performed on older people has been established previously [8, 23].
Statistical analysis
All statistical tests were conducted using SPSS Release 11 for Windows (SPSS, Chicago, IL, USA). In order to determine the suitability of the data for factor analysis, the Kaiser–Meyer–Olkin Measure Of Sampling Adequacy (KMO) and Bartlett's Test of Sphericity were calculated. The KMO was found to be 0.84, which exceeds the recommended minimum value of 0.60 [26]. Bartlett's Test of Sphericity was highly significant (χ2 = 764.55, P<0.001), supporting the suitability of the data for factor analysis [27]. Internal consistency was determined using Cronbach's α and the item–total correlation coefficients. Principal components analysis was then performed to determine whether the 17 items in the questionnaire could be combined into separate components reflecting different aspects of foot pain and disability. A four-component solution was extracted using the Kaiser–Guttman rule (eigenvalues >1.0), and varimax rotation was performed to minimize the complexity of loadings for each component.
Differences in the prevalence of medical conditions and pain between the disabling foot pain and no disabling foot pain groups were determined using the χ2 statistic and odds ratios [including 95% confidence intervals (CIs)]. Differences in foot characteristics between the groups were determined using independent samples t-tests. In those with disabling foot pain, correlations between the total MFPDI and MFPDI subscales with the GADS and SF-36 subscales were determined using the Pearson's r correlation coefficient.
Results
Characteristics of sample
The prevalence of major medical conditions, medication use and the use of walking aids in study population is shown in Table 1.
Sample characteristics, including prevalence of major medical conditions, medication use, and use of walking aids
| Condition . | Number (%) . |
|---|---|
| Medical conditions | |
| Heart condition | 71 (23.6) |
| Parkinson's disease | 5 (1.7) |
| Stroke | 9 (3.0) |
| High blood pressure | 134 (44.5) |
| Osteoarthritis | 174 (57.8) |
| Diabetes | 16 (5.3) |
| Incontinence | 63 (20.9) |
| More than 4 medications | 184 (61.1) |
| Occasionally use a walking aid | 22 (7.3) |
| Condition . | Number (%) . |
|---|---|
| Medical conditions | |
| Heart condition | 71 (23.6) |
| Parkinson's disease | 5 (1.7) |
| Stroke | 9 (3.0) |
| High blood pressure | 134 (44.5) |
| Osteoarthritis | 174 (57.8) |
| Diabetes | 16 (5.3) |
| Incontinence | 63 (20.9) |
| More than 4 medications | 184 (61.1) |
| Occasionally use a walking aid | 22 (7.3) |
Sample characteristics, including prevalence of major medical conditions, medication use, and use of walking aids
| Condition . | Number (%) . |
|---|---|
| Medical conditions | |
| Heart condition | 71 (23.6) |
| Parkinson's disease | 5 (1.7) |
| Stroke | 9 (3.0) |
| High blood pressure | 134 (44.5) |
| Osteoarthritis | 174 (57.8) |
| Diabetes | 16 (5.3) |
| Incontinence | 63 (20.9) |
| More than 4 medications | 184 (61.1) |
| Occasionally use a walking aid | 22 (7.3) |
| Condition . | Number (%) . |
|---|---|
| Medical conditions | |
| Heart condition | 71 (23.6) |
| Parkinson's disease | 5 (1.7) |
| Stroke | 9 (3.0) |
| High blood pressure | 134 (44.5) |
| Osteoarthritis | 174 (57.8) |
| Diabetes | 16 (5.3) |
| Incontinence | 63 (20.9) |
| More than 4 medications | 184 (61.1) |
| Occasionally use a walking aid | 22 (7.3) |
Internal consistency
The Cronbach's α calculation for the 17 items of the MFPDI was 0.89, indicating a high degree of internal consistency [28]. The item–total correlation coefficients ranged between 0.40 and 0.68 with four exceptions: item 1 (0.15), item 13 (0.25), item 15 (0.29) and item 17 (0.26).
Principal components analysis
Results of the principal components analysis are shown in Table 2, along with the factor structure reported in the original validation study. A four-factor model was extracted that accounted for 62% of the total variance. Component 1 represented seven items pertaining to functional limitation (items 2–8), component 2 represented six items pertaining to pain intensity (items 10, 11, 14–17), component 3 represented two items pertaining to concern about appearance (items 12 and 13), and component 4 represented two items pertaining to activity restriction (items 1 and 9).
Component coefficients of the individual items of the MFPDI in older people and comparison to factor structure of the original validation study by Garrow et al. [14]
| . | Component 1 . | Component 2 . | Component 3 . | Component 4 . | Garrow et al. . | Current . |
|---|---|---|---|---|---|---|
| Variance explained (%) . | 25.8 . | 17.4 . | 10.9 . | 7.9 . | [14] . | study . |
| Item | ||||||
| 1. I avoid walking outside at all | 0.717 | 0.903 | FL | ARa | ||
| 2. I avoid walking distances | 0.630 | FL | FL | |||
| 3. I don't walk in a normal way | 0.766 | FL | FL | |||
| 4. I walk slowly | 0.753 | FL | FL | |||
| 5. I have to stop and rest my feet | 0.679 | FL | FL | |||
| 6. I avoid hard or rough surfaces where possible | 0.733 | FL | FL | |||
| 7. I avoid standing for a long time | 0.806 | FL | FL | |||
| 8. I catch the bus or use the car more often | FL | FL | ||||
| 9. I need help with housework/shopping | 0.492 | FL | ARa | |||
| 10. I still do everything but with more pain or discomfort | 0.570 | PI | PI | |||
| 11. I get irritable when my feet hurt | 0.570 | FL | PIa | |||
| 12. I feel self-conscious about my feet | 0.870 | CA | CA | |||
| 13. I get self-conscious about the shoes I have to wear | 0.832 | CA | CA | |||
| 14. I have constant pain in feet | 0.736 | PI | PI | |||
| 15. My feet are worse in the morning | 0.720 | PI | PI | |||
| 16. My feet are more painful in the evening | 0.523 | PI | PI | |||
| 17. I get shooting pains in my feet | 0.728 | PI | PI |
| . | Component 1 . | Component 2 . | Component 3 . | Component 4 . | Garrow et al. . | Current . |
|---|---|---|---|---|---|---|
| Variance explained (%) . | 25.8 . | 17.4 . | 10.9 . | 7.9 . | [14] . | study . |
| Item | ||||||
| 1. I avoid walking outside at all | 0.717 | 0.903 | FL | ARa | ||
| 2. I avoid walking distances | 0.630 | FL | FL | |||
| 3. I don't walk in a normal way | 0.766 | FL | FL | |||
| 4. I walk slowly | 0.753 | FL | FL | |||
| 5. I have to stop and rest my feet | 0.679 | FL | FL | |||
| 6. I avoid hard or rough surfaces where possible | 0.733 | FL | FL | |||
| 7. I avoid standing for a long time | 0.806 | FL | FL | |||
| 8. I catch the bus or use the car more often | FL | FL | ||||
| 9. I need help with housework/shopping | 0.492 | FL | ARa | |||
| 10. I still do everything but with more pain or discomfort | 0.570 | PI | PI | |||
| 11. I get irritable when my feet hurt | 0.570 | FL | PIa | |||
| 12. I feel self-conscious about my feet | 0.870 | CA | CA | |||
| 13. I get self-conscious about the shoes I have to wear | 0.832 | CA | CA | |||
| 14. I have constant pain in feet | 0.736 | PI | PI | |||
| 15. My feet are worse in the morning | 0.720 | PI | PI | |||
| 16. My feet are more painful in the evening | 0.523 | PI | PI | |||
| 17. I get shooting pains in my feet | 0.728 | PI | PI |
Factor loadings less than 0.45 have been omitted in order to improve clarity.
FL, functional limitation; PI, pain intensity; CA, concern about appearance; AR, activity restriction.
aDifferent factor loading from original validation study.
Component coefficients of the individual items of the MFPDI in older people and comparison to factor structure of the original validation study by Garrow et al. [14]
| . | Component 1 . | Component 2 . | Component 3 . | Component 4 . | Garrow et al. . | Current . |
|---|---|---|---|---|---|---|
| Variance explained (%) . | 25.8 . | 17.4 . | 10.9 . | 7.9 . | [14] . | study . |
| Item | ||||||
| 1. I avoid walking outside at all | 0.717 | 0.903 | FL | ARa | ||
| 2. I avoid walking distances | 0.630 | FL | FL | |||
| 3. I don't walk in a normal way | 0.766 | FL | FL | |||
| 4. I walk slowly | 0.753 | FL | FL | |||
| 5. I have to stop and rest my feet | 0.679 | FL | FL | |||
| 6. I avoid hard or rough surfaces where possible | 0.733 | FL | FL | |||
| 7. I avoid standing for a long time | 0.806 | FL | FL | |||
| 8. I catch the bus or use the car more often | FL | FL | ||||
| 9. I need help with housework/shopping | 0.492 | FL | ARa | |||
| 10. I still do everything but with more pain or discomfort | 0.570 | PI | PI | |||
| 11. I get irritable when my feet hurt | 0.570 | FL | PIa | |||
| 12. I feel self-conscious about my feet | 0.870 | CA | CA | |||
| 13. I get self-conscious about the shoes I have to wear | 0.832 | CA | CA | |||
| 14. I have constant pain in feet | 0.736 | PI | PI | |||
| 15. My feet are worse in the morning | 0.720 | PI | PI | |||
| 16. My feet are more painful in the evening | 0.523 | PI | PI | |||
| 17. I get shooting pains in my feet | 0.728 | PI | PI |
| . | Component 1 . | Component 2 . | Component 3 . | Component 4 . | Garrow et al. . | Current . |
|---|---|---|---|---|---|---|
| Variance explained (%) . | 25.8 . | 17.4 . | 10.9 . | 7.9 . | [14] . | study . |
| Item | ||||||
| 1. I avoid walking outside at all | 0.717 | 0.903 | FL | ARa | ||
| 2. I avoid walking distances | 0.630 | FL | FL | |||
| 3. I don't walk in a normal way | 0.766 | FL | FL | |||
| 4. I walk slowly | 0.753 | FL | FL | |||
| 5. I have to stop and rest my feet | 0.679 | FL | FL | |||
| 6. I avoid hard or rough surfaces where possible | 0.733 | FL | FL | |||
| 7. I avoid standing for a long time | 0.806 | FL | FL | |||
| 8. I catch the bus or use the car more often | FL | FL | ||||
| 9. I need help with housework/shopping | 0.492 | FL | ARa | |||
| 10. I still do everything but with more pain or discomfort | 0.570 | PI | PI | |||
| 11. I get irritable when my feet hurt | 0.570 | FL | PIa | |||
| 12. I feel self-conscious about my feet | 0.870 | CA | CA | |||
| 13. I get self-conscious about the shoes I have to wear | 0.832 | CA | CA | |||
| 14. I have constant pain in feet | 0.736 | PI | PI | |||
| 15. My feet are worse in the morning | 0.720 | PI | PI | |||
| 16. My feet are more painful in the evening | 0.523 | PI | PI | |||
| 17. I get shooting pains in my feet | 0.728 | PI | PI |
Factor loadings less than 0.45 have been omitted in order to improve clarity.
FL, functional limitation; PI, pain intensity; CA, concern about appearance; AR, activity restriction.
aDifferent factor loading from original validation study.
Proportions and correlates of disabling foot pain
Using the MFPDI case definition, 108 people (36%) were found to have disabling foot pain. Of these, 76 (70%) reported pain in the forefoot, 51 (47%) reported pain in the heel and 50 (46%) reported pain in the arch. Participants with disabling foot pain were more likely to report back pain [χ2 = 11.70, P = 0.001; odds ratio (OR) = 2.72, 95% CI 1.51–4.89], hip pain (χ2 = 7.07, P = 0.029; OR = 1.88, 95% CI 1.15–3.07), knee pain (χ2 = 11.41, P = 0.001; OR = 2.36, 95% CI 1.42–3.90) and pain in the hands or wrists (χ2 = 26.02, P<0.001; OR = 3.52, 95% CI 2.15–5.76). There were no significant associations between disabling foot pain and any of the major medical conditions.
Characteristics of participants with and without disabling foot pain are shown in Table 3. There were no differences in age, gender or BMI between those with and without disabling foot pain. Participants with disabling foot pain had lower arches (t = 2.71, P = 0.007) and less ankle joint motion (t = 2.65, P = 0.008); however, there was no difference in the overall foot problem score between the two groups.
Characteristics of subjects with and without disabling foot pain (DFP)
| . | No DFP (n = 193) . | DFP (n = 108) . |
|---|---|---|
| Age | 77.38 (4.89) | 76.88 (4.90) |
| Gender (% female) | 58 | 66 |
| BMI | 0.26 (0.04) | 0.27 (0.04) |
| Navicular heighta,b | 0.184 (0.026) | 0.174 (0.032) |
| Ankle flexibilityb | 38.99 (9.04) | 36.07 (8.75) |
| Foot problem score | 5.98 (5.31) | 6.56 (5.07) |
| . | No DFP (n = 193) . | DFP (n = 108) . |
|---|---|---|
| Age | 77.38 (4.89) | 76.88 (4.90) |
| Gender (% female) | 58 | 66 |
| BMI | 0.26 (0.04) | 0.27 (0.04) |
| Navicular heighta,b | 0.184 (0.026) | 0.174 (0.032) |
| Ankle flexibilityb | 38.99 (9.04) | 36.07 (8.75) |
| Foot problem score | 5.98 (5.31) | 6.56 (5.07) |
Data are mean (s.d.) unless otherwise indicated.
aNormalized for foot length;
bP<0.01.
Characteristics of subjects with and without disabling foot pain (DFP)
| . | No DFP (n = 193) . | DFP (n = 108) . |
|---|---|---|
| Age | 77.38 (4.89) | 76.88 (4.90) |
| Gender (% female) | 58 | 66 |
| BMI | 0.26 (0.04) | 0.27 (0.04) |
| Navicular heighta,b | 0.184 (0.026) | 0.174 (0.032) |
| Ankle flexibilityb | 38.99 (9.04) | 36.07 (8.75) |
| Foot problem score | 5.98 (5.31) | 6.56 (5.07) |
| . | No DFP (n = 193) . | DFP (n = 108) . |
|---|---|---|
| Age | 77.38 (4.89) | 76.88 (4.90) |
| Gender (% female) | 58 | 66 |
| BMI | 0.26 (0.04) | 0.27 (0.04) |
| Navicular heighta,b | 0.184 (0.026) | 0.174 (0.032) |
| Ankle flexibilityb | 38.99 (9.04) | 36.07 (8.75) |
| Foot problem score | 5.98 (5.31) | 6.56 (5.07) |
Data are mean (s.d.) unless otherwise indicated.
aNormalized for foot length;
bP<0.01.
Correlates of MFPDI scores in those with disabling foot pain
The MFPDI total score was significantly associated with the GADS depression subscale (r = 0.34, P<0.001), as was the MFPDI functional limitation subscale (r = 0.32, P = 0.001), the MFPDI pain intensity subscale (r = 0.23, P = 0.015) and the MFPDI concern about appearance subscale (r = 0.28, P = 0.004).
The MFPDI functional limitation subscale was significantly correlated with the SF-36 mental health subscale (r = 0.20, P = 0.039). The MFPDI activity restriction subscale was significantly associated with the SF-36 general health subscale (r = 0.21, P = 0.029).
There were no significant associations between the MFPDI total score (or its subscales) and age, gender, BMI, the presence of osteoarthritis or pain in the back, hips, knees hands or wrists.
Discussion
The purpose of this study was to evaluate the psychometric properties of the Manchester Foot Pain and Disability Index (MFPDI) in a random sample of older people and to determine the correlates of disabling foot pain in this age-group. Before discussing these findings, however, it needs to be acknowledged that the response rate was relatively low (31%). Furthermore, due to the study exclusion criteria and despite our attempt to maximize the participation rates of older people with mobility limitations, we acknowledge that the majority of the participants was independent community-dwelling people and the findings may not be generalizable beyond this group. Nevertheless, the performance of the MFPDI in our sample was similar to the initial validation study, which involved three groups of younger people (rheumatology patients, median age 53; people attending a general practitioner, median age 61; and community-dwelling people, median age 50). The internal consistency reported in our study was slightly lower (Cronbach's α was 0.89 compared with 0.99), although well above the lower limit of 0.70 considered acceptable [28]. Indeed, it could be argued that the very high α reported by Garrow et al. [14] represents a high degree of item redundancy in the MFPDI when applied to their middle-aged population.
Despite these similarities, important differences were revealed by the principal components analysis. Garrow et al. [14] extracted a four-component solution reflecting three constructs: functional limitation, pain intensity and concern about personal appearance, the pain intensity construct being split between two components. Although we also extracted a four-component model, there appeared to be a distinct fourth construct consisting of two items, ‘I avoid walking outside at all’ and ‘I need help with housework/shopping’, which we have designated ‘activity restriction’. The wording of these items appears to represent a more severe degree of impairment. Whereas the functional limitation component relates to reduced ability to perform some mobility tasks, the fourth component relates more to inability to perform the two tasks. The delineation of this additional construct is consistent with the body of literature, which indicates that interference from pain with everyday activities is highly prevalent in this age group [4, 29–31]. Based on this finding, it may be worthwhile separating the MFPDI into four subscales rather than the original three when the tool is used in an older population, as the additional subscale may assist in the identification of people with more pronounced foot pain-related disability.
The other difference in our factor structure was that item 11 (‘I get irritable when my feet hurt’) was located within the pain intensity component rather than the functional impairment component. The wording of this item is somewhat ambiguous, in that it could be interpreted as either a measure of the sensory experience of pain (the word ‘irritating’ being similar to other commonly used descriptors such as ‘annoying’, ‘troublesome’ and ‘miserable’) or as a measure of frustration with the activity limitations associated with the pain. The factor loadings reported here suggest that older people may be more likely to interpret this question as a pain construct rather than a functional limitation construct.
The prevalence of foot pain in our group, using the case definition proposed by Garrow et al. [14], was slightly higher than in previous population-based studies of older people [1–3, 7, 13], possibly due to the higher mean age of our sample (77.2 yr). The associations between foot symptoms and pain at other body regions is consistent with previous reports [2, 11, 13, 15], indicating that chronic and severe foot pain in some older people may be part of a generalized osteoarthritis or systemic pain condition. Although the differences were small, participants with disabling foot pain also had lower arches and less motion available at the ankle joint. This finding is in contrast to that of Garrow et al. [15], who found no association between undefined pes planus (flat feet) and disabling foot pain in a population study of 281 people. This inconsistency may be due to differences in arch height assessment; while we used a continuous measure of arch height using a validated technique [22], Garrow et al. [15] used a dichotomous classification based on visual observation. The association between disabling foot pain and reduced ankle joint motion is a novel finding, and may be an indicator of overall lower limb inflexibility due to inactivity or osteoarthritis. The associations between low arches, ankle inflexibility and foot pain in older people are plausible, as previous research has implicated flat feet and reduced range of motion as a risk factor for a range of musculoskeletal conditions affecting the leg and foot [32].
The association reported between disabling foot pain and the depression subscale of the GADS is also a novel finding. Although it has long been recognized that many older people with chronic pain have significant depressive symptoms [33], such an association has been suggested [34] but not confirmed with specific reference to foot pain. Interestingly, when the MFPDI was broken down into its subscales, three (functional limitation, pain intensity and concern about appearance) were significantly associated with depression. The association with functional limitation is consistent with Gibson et al. [35], who have recently shown that self-reported interference from pain was a significant independent predictor of depressive symptoms in a sample of older people attending a pain management clinic. The association between depression and concern about the appearance of the foot or footwear has not been studied previously; however, reduced self-esteem due to concerns about physical appearance has been reported in people with fungal nail infection [36], a common foot problem in older people. Furthermore, concern regarding footwear aesthetics has been postulated as an explanation for low levels of compliance associated with medical-grade footwear [37]. The relationship between foot pain, deformity, aesthetic concerns and depression warrants further investigation, as it may provide some useful clinical insights into the management of unresponsive cases of chronic foot pain in older people.
Conclusion
The findings of this study indicate that disabling foot pain in older people is associated with pain in other body regions, depression, flatter feet and reduced range of ankle joint motion. Furthermore, the MFPDI appears to be a useful instrument for assessing foot pain in older people, although the component structure differs from the original validation of the instrument due to the delineation of an activity restriction construct. Increased use of the instrument in both epidemiological studies and clinical trials will further develop our understanding of this common and disabling condition.
H.B.M. is currently NHMRC Australian Clinical Research Fellow (id: 234424). This study was supported by the NHMRC Health Research Partnerships Grant ‘Prevention of Injuries in Older People’. Dr Kaarin Anstey provided useful comments on an earlier draft of this manuscript.
The authors have no conflicts of interest to declare.
References
Benvenuti F, Ferrucci L, Guralnik JM, Gangemi S, Baroni A. Foot pain and disability in older persons: an epidemiologic survey.
Chen J, Devine A, Dick IM, Dhaliwal SS, Prince RL. Prevalence of lower extremity pain and its association with functionality and quality of life in elderly women in Australia.
Dunn JE, Link CL, Felson DT, Crincoli MG, Keysor JJ, McKinlay JB. Prevalence of foot and ankle conditions in a multiethnic community sample of older adults.
Thomas E, Peat G, Harris L, Wilkie R, Croft PR. The prevalence of pain and pain interference in a general population of older adults: cross-sectional findings from the North Staffordshire Osteoarthritis Project (NorStOP).
Black JR, Hale WE. Prevalence of foot complaints in the elderly.
Bowling A, Grundy E. Activities of daily living: changes in functional ability in three samples of elderly and very elderly people.
Gorter KJ, Kuyvenhoven MM, deMelker RA. Nontraumatic foot complaints in older people. A population-based survey of risk factors, mobility, and well-being.
Menz HB, Lord SR. The contribution of foot problems to mobility impairment and falls in older people.
Menz HB, Morris ME, Lord SR. Foot and ankle characteristics associated with impaired balance and functional ability in older people.
Leveille SG, Bean J, Bandeen-Roche K, Jones R, Hochberg M, Guralnik JM. Musculoskeletal pain and risk of falls in older disabled women living in the community.
Menz HB, Morris ME. Determinants of disabling foot pain in retirement village residents.
Menz HB, Morris ME. Footwear characteristics and foot problems in older people.
Leveille SG, Guralnik JM, Ferrucci L, Hirsch R, Simonsick E, Hochberg MC. Foot pain and disability in older women.
Garrow AP, Papageorgiou AC, Silman AJ, Thomas E, Jayson MIV, Macfarlane GJ. Development and validation of a questionnaire to assess disabling foot pain.
Garrow AP, Silman AJ, Macfarlane GJ. The Cheshire Foot Pain and Disability Survey: a population survey assessing prevalence and associations.
Waxman R, Woodburn H, Powell M, Woodburn J, Blackburn S, Helliwell P. FOOTSTEP: a randomized controlled trial investigating the clinical and cost effectiveness of a patient self-management program for basic foot care in the elderly.
Gibson SJ, Katz B, Corran TM, Farrell MJ, Helme RD. Pain in older persons.
Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician.
Goldberg D, Bridges K, Duncan-Jones P. Detecting anxiety and depression in general medical settings.
McCallum J. The SF-36 in an Australian sample: validating a new, generic health status measure.
Menz HB, Munteanu SE. Validity of 3 clinical techniques for the measurement of static foot posture in older people.
Menz HB, Tiedemann A, Kwan MMS, Latt MD, Lord SR. Reliability of clinical tests of foot and ankle characteristics in older people.
Garrow AP, Papageorgiou A, Silman AJ, Thomas E, Jayson MI, Macfarlane GJ. The grading of hallux valgus. The Manchester Scale.
Menz HB, Munteanu SE. Radiographic validation of the Manchester scale for the classification of hallux valgus deformity.
Bartlett MS. A note on the multiplying factors for various chi square approximations.
Cronbach LJ. Coefficient alpha and the internal structure of tests.
Scudds RJ, Ostbye T. Pain and pain-related interference with function in older Canadians: the Canadian Study of Health and Aging.
Reid MC, Guo Z, Towle VR, Kerns RD, Concato J. Pain-related disability among older male veterans receiving primary care.
Reyes-Gibby CC, Aday L, Cleeland C. Impact of pain on self-rated health in the community-dwelling older adults.
Kaufman KR, Brodine SK, Shaffer RA, Johnson CW, Cullison TR. The effect of foot structure and range of motion on musculoskeletal overuse injuries.
Romano JM, Turner JA.
Helfand AE. Foot pain in later life. Some psychological correlates.
Gibson SJ, Helme RD. Cognitive factors and the experience of pain and suffering in older persons.
Lubeck DP, Patrick DL, McNulty P, Fifer SK, Birnbaum J. Quality of life of persons with onychomycosis.
Author notes
1Musculoskeletal Research Centre, Faculty of Health Sciences, La Trobe University, Bundoora, Vic. and 2Prince of Wales Medical Research Institute, Randwick, NSW, Australia.



Comments