-
PDF
- Split View
-
Views
-
Cite
Cite
Charlotte Medin, Carl‐Gustaf Elinder, Britta Hylander, Birgit Blom, Henryk Wilczek, Survival of patients who have been on a waiting list for renal transplantation, Nephrology Dialysis Transplantation, Volume 15, Issue 5, May 2000, Pages 701–704, https://doi.org/10.1093/ndt/15.5.701
Close - Share Icon Share
Abstract
Introduction. Survival of transplanted patients is generally much better than for those on dialysis. This comparison is, however, incorrect, as in order to be accepted for renal transplantation the patient has to be in a relatively good condition and in addition transplanted patients are usually younger. We compared survival of all renal replacement therapy (RRT) patients who had undergone an identical medical check‐up, been accepted, and put on the waiting list for cadaveric‐kidney transplantation at Huddinge University hospital. A comparison with patients who were transplanted with a kidney from a living related donor (LD) is also included.
Methods. All patients (n=608) accepted and on the waiting list for renal transplantation between January 1987 and April 1996 formed the basis of the study. Follow‐up was terminated on 31 December 1997. Survival was recorded from the date that the patients were accepted and put on the waiting list. As long as the patient was not transplanted and remained on dialysis treatment, survival was considered as ‘survival on dialysis’, and if transplanted, subsequent survival was defined as ‘survival after cadaveric‐kidney transplantation’. A patient who had been transplanted remained in that group for the rest of the observation period even if the transplantation had failed and the patient had to go back to dialysis after the surgery.
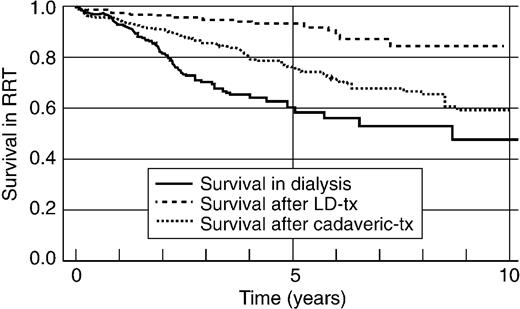
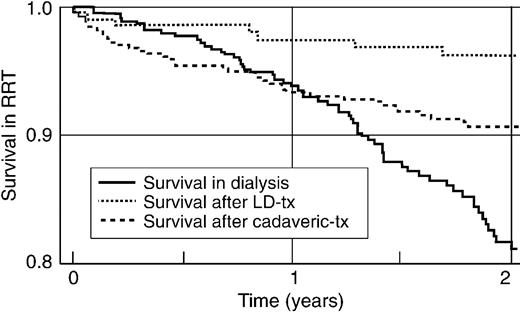
Results. Five‐year survival was considerably better after LD‐kidney transplantation (94%), than after cadaveric‐kidney transplantation (76%) or on chronic dialysis (60%). Cox hazard regression analysis gave an age‐adjusted relative risk for death of 0.46 for LD‐transplanted and 1.49 for remaining on dialysis compared with cadaveric‐transplanted patients. Transplanted patients, however, experienced a higher mortality during the first year after the transplantation than patients still on dialysis.
Conclusions. LD‐kidney transplantation is clearly associated with a superior survival. Mortality is relatively high after cadaveric‐kidney transplantation, especially during the first months after surgery. Nevertheless, in the long term cadaveric kidney transplanted patients have a better survival than those remaining on dialysis.
Introduction
Kidney transplantation is, when possible, a superior treatment for renal replacement therapy (RRT) compared to dialysis treatment. The 5‐year survival of kidney‐transplanted patients is commonly reported as being in the range 80–90% whereas among dialysis patients it is usually 50–60% [1]. The 5‐year survival for dialysis patients in Sweden between 1991 and 1997 for patients younger than 15 years was 81%, for patients between 15 and 40 years 64%, and between 40 and 65 years 33%; for patients older than 65 years the 5‐year survival was 16% [2]. The overall 5‐year survival rates for transplanted patients with living donors are 94%, for patients with cadaveric kidneys 81%, and for all transplanted diabetics 78% [2]. The comparison between these two groups of dialysis and transplanted patients is, however, severely biased, as there are selection processes. The patients accepted for transplantation are younger and healthier than those who remain on dialysis treatment [3]. A patient has to undergo a thorough medical assessment to be accepted for renal transplantation in Sweden. There are a number of relative and absolute contraindications for renal transplantation, such as current or recent malignancy, overt cardiovascular disease, high age (>70 years), cachexia, severe overweight, chronic infections etc. In addition the adult patients (aged >15 years), have to be started on dialysis before they can be put on the waiting list. Pre‐emptive transplantation was only performed in children or when there was a living‐related (LD) kidney available.
In this study we have made an attempt to make a more appropriate comparison between RRT patients who undergo transplantation and those who remain on dialysis. We compared survival of all RRT patients who had undergone the same medical check‐up, been accepted, and put on a waiting list for cadaver kidney transplantation at Huddinge University hospital. One could say that all patients on the waiting list had passed through the same ‘needle's eye’. The intention to treat was the same for all. Based on various circumstances, not related to the general condition of the patient or the cause of the renal disease at the time of acceptance, the dialysis patient eventually became transplanted or not. Our approach is very similar to that of Port et al. [4], who examined survival of RRT patients on a waiting list in Michigan, USA. In addition to the American study, we also include a comparison of patients who are transplanted with a kidney from an LD.
Subjects and methods
All patients (n=608, 380 men and 228 women) accepted and on the waiting list for renal transplantation at Huddinge hospital between January 1987 and April 1996 formed the basis for our study. Huddinge hospital is the only place were renal transplantations are performed in greater Stockholm, a catchment area having a population size of about 2 million. The waiting list comprised patients treated with peritoneal dialysis as well as haemodialysis. Twelve were children with ages less than 16 years. Fifty‐seven individuals already on the list before January 1987 were excluded, as they comprise a ‘surviving selection’. Follow‐up was terminated on 31 December 1997, when censoring took place if the patient had not died before that date. Survival time was recorded from the date that the patients were accepted and put on the waiting list. As long as the patient was not transplanted and remained on dialysis treatment, survival was considered as ‘survival on dialysis’. If transplanted, subsequent survival was defined as ‘survival after cadaveric‐kidney transplantation’. A patient who had been transplanted remained in that group for the rest of the observation period even if the transplantation failed and the patient had to go back to dialysis after the surgery. If the general condition of the patient accepted for transplantation deteriorated, and the patient had to be taken down from the waiting‐list before any transplantation, survival was still followed and the patient was included in the ‘survival on dialysis’ group. Comparison was also made with patients who during the same time‐period were transplanted with a LD kidney presented as ‘Survival after LD kidney transplantation’. For each patient the following information was retrieved; date of birth, date of first dialysis, primary renal diagnosis based on the EDTA–ERA (European Dialysis and Transplantation Association–European Renal Association) codes for renal diseases, date of transplantation, and date of death. No individuals were lost to follow‐up.
Survival was examined by conventional Kaplan–Meier analysis and Cox proportional hazard regression analysis, the latter enabling adjustments for co‐variates such as age and diagnosis. Software programs used were; StatView® March 1998 and JMP® from SAS Institute Inc.
Results
One‐third of the patients were on peritoneal dialysis treatment when put on the list and the remaining two‐thirds were on haemodialysis treatment. Of the 596 adult (aged >15) patients on the waiting list, 426 were transplanted before 30 April 1996, whereas 170 remained on dialysis until death or the end of the observation period. During the same time‐period 197 adult patients were transplanted with a LD kidney. Table 1 presents the primary renal disease in the three groups. Most children were transplanted with a LD kidney. A total of 228 individuals died during the observation period; of these 97 were on the waiting list, 114 had been transplanted with a cadaveric kidney, and 17 transplanted with a LD kidney. Cardiovascular deaths were most common in all three groups: 87, 69, and 58% in the LD group, cadaveric group, and those who remained on dialysis. Infections were the cause of death in 20% in the cadaveric‐kidney group and 19% in the group remaining on dialysis.
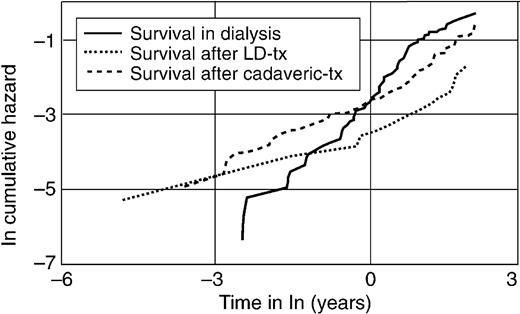
Figure 1 presents the survival of patients in the three groups; ‘survival on dialysis’, ‘survival after cadaveric‐kidney transplantation’, and ‘survival after LD‐kidney transplantation’. To make the groups more comparable, children aged less than 16 years were excluded in the Cox regression survival analysis. After 5 years, survival was considerably better after LD‐kidney transplantation (94%), than after cadaveric‐kidney transplantation (76%), or during continued dialysis (60%). However, as shown in Figure 2, transplanted patients during the first year after transplantation experienced a higher mortality than patients still on dialysis. The average age was somewhat different in the three groups: 40 years (SD 13) at LD‐kidney transplantation, 47 years (SD 13) at cadaveric kidney transplantation, and 49 (SD 13) when put on the waiting list. Obviously this difference in age has consequences on the survival. We therefore proceeded with a Cox regression analysis where age was adjusted. Table 2 presents the relative risk ratio for death in the LD‐transplanted group and those remaining on dialysis compared to the cadaveric kidney transplanted group. Again the LD group has a considerably reduced risk of death than patients transplanted with a cadaveric kidney, which, nevertheless, have a better survival than patients remaining on dialysis. The relative risk ratio, however, is not constant over time and thus it is not really appropriate to present crude risk ratios [4,5]. Figure 3 displays the logarithm of cumulative hazard for death in the three groups over time. Shortly after a patient has been put on the waiting list, the risk of death is less than for transplanted patients. The lines for LD‐ and cadaveric‐kidney transplanted patients are parallel, whereas the dialysis group have a steeper slope. After about 1 year (Figure 3, ln‐time=0) the hazard line for dialysis patients crosses the cadaveric transplanted group. Thus survival in the first year is better for patients on dialysis, but as time goes on survival is better for transplanted patients, in particular patients who have received a LD‐kidney.
Cause of renal disease in patients who had been transplanted with a LD kidney (n=197), a cadaveric‐kidney (n=426), and those who remained on dialysis (n=170)
| LD | Cadaveric | Remaining on dialysis | |
| Chronic glomerulonephritis | 46% | 35% | 29% |
| Diabetic nephropathy | 15% | 23% | 22% |
| Polycystic kidney disease | 12% | 13% | 11% |
| Nephrosclerosis | 7% | 9% | 9% |
| Interstitial and chronic pyelonephritis | 5% | 9% | 8% |
| Other causes | 8% | 10% | 10% |
| Unknown cause | 6% | 1% | 11% |
| LD | Cadaveric | Remaining on dialysis | |
| Chronic glomerulonephritis | 46% | 35% | 29% |
| Diabetic nephropathy | 15% | 23% | 22% |
| Polycystic kidney disease | 12% | 13% | 11% |
| Nephrosclerosis | 7% | 9% | 9% |
| Interstitial and chronic pyelonephritis | 5% | 9% | 8% |
| Other causes | 8% | 10% | 10% |
| Unknown cause | 6% | 1% | 11% |
Cause of renal disease in patients who had been transplanted with a LD kidney (n=197), a cadaveric‐kidney (n=426), and those who remained on dialysis (n=170)
| LD | Cadaveric | Remaining on dialysis | |
| Chronic glomerulonephritis | 46% | 35% | 29% |
| Diabetic nephropathy | 15% | 23% | 22% |
| Polycystic kidney disease | 12% | 13% | 11% |
| Nephrosclerosis | 7% | 9% | 9% |
| Interstitial and chronic pyelonephritis | 5% | 9% | 8% |
| Other causes | 8% | 10% | 10% |
| Unknown cause | 6% | 1% | 11% |
| LD | Cadaveric | Remaining on dialysis | |
| Chronic glomerulonephritis | 46% | 35% | 29% |
| Diabetic nephropathy | 15% | 23% | 22% |
| Polycystic kidney disease | 12% | 13% | 11% |
| Nephrosclerosis | 7% | 9% | 9% |
| Interstitial and chronic pyelonephritis | 5% | 9% | 8% |
| Other causes | 8% | 10% | 10% |
| Unknown cause | 6% | 1% | 11% |
Relative risk of death, according to Cox regression, for two groups of RRT patients: those transplanted with a living related kidney donor (LD), and those remaining on dialysis. Transplantation with a cadaveric‐kidney comprised the reference
| Co‐variate | Risk ratio | 95% confidence interval |
| Age | 1.049 | 1.038–1.061 |
| LD‐transplanted | 0.46 | 0.27–0.78 |
| On dialysis treatment | 1.49 | 1.12–1.99 |
| Co‐variate | Risk ratio | 95% confidence interval |
| Age | 1.049 | 1.038–1.061 |
| LD‐transplanted | 0.46 | 0.27–0.78 |
| On dialysis treatment | 1.49 | 1.12–1.99 |
Relative risk of death, according to Cox regression, for two groups of RRT patients: those transplanted with a living related kidney donor (LD), and those remaining on dialysis. Transplantation with a cadaveric‐kidney comprised the reference
| Co‐variate | Risk ratio | 95% confidence interval |
| Age | 1.049 | 1.038–1.061 |
| LD‐transplanted | 0.46 | 0.27–0.78 |
| On dialysis treatment | 1.49 | 1.12–1.99 |
| Co‐variate | Risk ratio | 95% confidence interval |
| Age | 1.049 | 1.038–1.061 |
| LD‐transplanted | 0.46 | 0.27–0.78 |
| On dialysis treatment | 1.49 | 1.12–1.99 |
Kaplan–Meier survival curves for three groups of RRT patients: those transplanted with a living‐related kidney donor (LD), those transplanted with a cadaveric kidney, and those remaining on dialysis. Follow‐up for 10 years.
Kaplan–Meier hazard plot for three groups of RRT patients: those transplanted with a living‐related kidney donor (LD), those transplanted with a cadaveric kidney, and those remaining on dialysis. Note that these are logarithmic scales.
Discussion
Kidney transplantation is the preferred form of RRT when feasible. Long‐term survival is better [1,6,7], costs are considerably less than for dialysis [8] and quality of life is much better [9,10]. If crude unadjusted comparisons are made between dialysis and transplantation without considering diagnosis, age, and co‐morbidities, the differences between survival on dialysis and after transplantation become vast. This is, however, an unfair comparison as preferentially relatively young and healthy patients are transplanted, whereas the individuals who remain on dialysis treatment to a great extent comprise a precipitate of elderly with one or several co‐morbidities severe enough to prevent acceptance for transplantation. Our approach has been to compare survival of patients who have all been accepted for cadaveric kidney transplantation after a careful medical examination. For all patients on the waiting list there was the same initial intention to treat. The algorithm for allocation of cadaveric kidneys to patients on the waiting list between 1987 and 1997 was based on best HLA match between donor and recipient, blood group compatibility, and the existence of a negative cross‐match. Priority was also given to children aged less than 16. Age, gender, and size matching was not used. In relatively few cases priority for receiving a cadaveric‐kidney was given to patients who had been on the waiting list for a very long time or who for some other reasons had particular problems in coping with the dialysis treatment. Thus the allocation of organs cannot be regarded as at random. After exclusion of children, the average age of patients who received a cadaveric graft was nevertheless similar and not significantly different from those who remained on dialysis: 47 and 49 respectively. Likewise, the causes of renal disease were similar (Table 1). No selection of recipients was based on expected survival. Thus, we feel that although the comparison between transplanted and non‐transplanted patients is not ideal from a purely methodological viewpoint, it is the best achievable. In particular after adjustment of age in the Cox regression (Table 2) the comparison between transplanted and non‐transplanted should be sound. Port et al. [4] examined mortality in all RRT patients aged <65 who were placed on a waiting list for renal transplantation between January 1984 and December 1989 in Michigan, USA. About 50% of the patients on the waiting list (n=799) received a cadaveric graft. Survival was compared between transplanted and non‐transplanted and with those who had never been on the waiting list (n=5020). The crude death rate was considerably less for patients accepted for renal transplantation (10.7% per year) as compared to RRT patients not considered suitable to be placed on the waiting list (20.6% per year). According to a Cox regression, the relative risk of death for patients on the waiting list was 0.60 compared to those who were not on the list. After transplantation the death rate was still lower (8.6% per year). After adjustment for age, sex, primary cause of ESRD, and year of first diagnosis, the Cox regression revealed that the average relative risk of dying for transplanted patients more than 1 year after transplantation was considerably less (40%) than among those who were still waiting for a renal transplantation. This is very similar to what we report here (Figure 1, Table 2). Also similar to our report (Figures 2 and 3), the relative risk of mortality was significantly higher for the transplanted group during the first 4 months after surgery. This is an expected finding as the transplantation surgery, and in particular the subsequent immunosuppressive treatment, carries a considerable risk of mortality, particularly in infectious and cardiovascular diseases. Our results are also in accordance with the more recent findings of Schnuelle et al. [11].
It may be concluded that there is a clear long‐term survival benefit for patients being transplanted as compared to those patients who remained on dialysis, although mortality is increased initially.
The most pronounced difference, however, is not between cadaveric transplanted or dialysis, but rather between patients receiving a LD‐ or cadaveric‐kidney transplant (Figures 2 and 3, Table 2). After 5 years, 94% of the LD‐transplanted patients were still alive, compared to 76% of the cadaveric transplanted group. The relative risk ratio of death in the LD group was 0.44, or in other words, the risk for death during any given time period is, in the LD group, about 44% of that in the cadaveric‐group. This risk ratio is very similar to that reported from one centre in The Netherlands in a follow‐up study of survival for all kidney transplanted patients in Leiden between 1966 and 1994, which comprised 86 living related and 916 cadaver donors [12]. After adjustment for age and sex the relative risk of mortality was 0.5 (95% CI 0.2–1.03) in the LD group.
To summarize, LD‐kidney transplantation is clearly associated with a superior survival. Mortality is relatively high after cadaveric‐kidney transplantation, especially during the first months after surgery. In the long term, however, cadaveric‐kidney transplanted patients have a considerably better survival than those remaining on dialysis.
Correspondence and offprint requests to: Charlotte Medin MD, Department of Nephrology, Karolinska Hospital, S‐171 76 Stockholm, Sweden.
References
Mailloux LU, Henrich WL. Patient survival and the adequacy of maintenance dialysis. Up To Date, Sept 25,
Swedish Registry for Active Uremia. Staffan Schön, ed.
Schwab SJ, Paul LC. Survival with end‐stage renal failure in the 1990s.
Port FK, Wolfe RA, Mauger EA, Berling DP, Jiang K. Comparison of survival probabilities for dialysis patients vs. cadaveric renal transplant recipients.
Bradley JR, Evans DB, Calne RY. Long‐term survival in haemodialysis patients.
Harris SAC, Brown EA. Patients surviving more then 10 years on haemodialysis. The natural history of the complications of the treatment.
Karlberg I, Nyberg G. Cost‐effectiveness studies of renal transplantation.
Churchill DN, Torrance GW, Taylor DW et al. Measurement of quality of life in end‐stage renal disease. The time trade‐off approach.
Bremer BA, McCausley CR, Wrona RM, Johnson JP. Quality of life in end‐stage renal disease.
Schnuelle P, Lorenz D, Trede M, Van der Woude FJ. Impact of renal cadaveric transplantation on survival in end‐stage renal failure: Evidence for reduced mortality risk compared with hemodialysis during long‐term follow‐up.





Comments