Abstract
Background/aims
Quality assurance and funding of care become a major challenge against the background of demographic changes in western societies. The primary aim of the study was to identify possible misclassification, respectively over and undersupply of care by comparing the Barthel Index of clients of home care service with the level of care (Stage 0, I, II, III) according to the statutory German long-term care insurance.
Methods
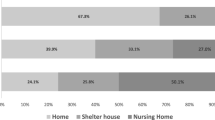
In 2012, a multi-center point prevalence study of 878 randomly selected clients of 100 randomly selected home care services across Germany was conducted. According to a standardized study protocol, demographics, the Barthel Index and the nurses’ professional judgment—whether a client requires more nursing care—were assessed. Associations of the Barthel items and professional judgment were analyzed using univariate (Chi-square) and multivariate (logistic regression and classification-regression-tree-models) statistics.
Results
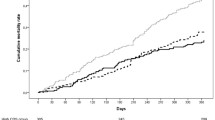
In each level of care, the Barthel Index showed large variability e.g. in level II ranging from 0 to 100 points. Multivariate logistic regression regarding possible under- and oversupply revealed occasionally fecal incontinence (2.1; 95 % CI 1.2–3.7), urinary incontinence (2.0; 95 % CI 1.1–3.6), feeding (1.7; 95 % CI 1.0–2.9), immobility (0.2; 95 % CI 0.1–0.6) and to be female (1.8; 95 % CI 1.2–2.6) to be statistically significantly associated.
Conclusion
The variability in Barthel Index in each level of care found in this study indicated a large general misclassification of home care clients according to their actual need of care. Professional caregivers identified occasional incontinence, help with eating and drinking and mobility (especially in female clients) as areas of possible under- and oversupply of care. The statutory German long-term care insurance classification should be modified according to the above finding to increase the quality of care in home care clients.



Similar content being viewed by others
References
Thorslund M, Norstrom T, Wernberg K (1991) The utilization of home help in Sweden—a multivariate-analysis. Gerontologist 31(1):116–119
Deutschland Statistisches Bundesamt (2011) Ältere Menschen in Deutschland und der EU: im Blickpunkt. DeStatis: wissen, nutzen. Statistisches Bundesamt, Wiesbaden
Sager MA, Franke T, Inouye SK, Landefeld CS, Morgan TM, Rudberg MA, Sebens H, Winograd CH (1996) Functional outcomes of acute medical illness and hospitalization in older persons. Arch Intern Med 156(6):645–652
Covinsky KE, Palmer RM, Fortinsky RH, Counsell SR, Stewart AL, Kresevic D, Burant CJ, Landefeld CS (2003) Loss of independence in activities of daily living in older adults hospitalized with medical illnesses: increased vulnerability with age. J Am Geriatr Soc 51(4):451–458
Morris JN, Hawes C, Fries BE, Phillips CD, Mor V, Katz S, Murphy K, Drugovich ML, Friedlob AS (1990) Designing the national resident assessment instrument for nursing homes. Gerontologist 30(3):293–307
Dijkstra A, Buist G, Dassen T (1996) Nursing-care dependency. Development of an assessment scale for demented and mentally handicapped patients. Scand J Caring Sci 10(3):137–143
Mahoney FI, Barthel DW (1965) Functional Evaluation: the Barthel Index. Maryland State Med J 14:61–65
Collister B, Stein G, Katz D, DeBruyn J, Andrusiw L, Cloutier S (2012) Service guidelines based on Resource Utilization Groups Version III for Home Care provide decision-making support for case managers. Healthc Q 15(2):75–81
Sales AE, Bostrom AM, Bucknall T, Draper K, Fraser K, Schalm C, Warren S (2012) The use of data for process and quality improvement in long term care and home care: a systematic review of the literature. J Am Med Dir Assoc 13(2):103–113. doi:10.1016/j.jamda.2011.01.004
Wingenfeld K, Büscher A (2011) Instrumente zur Einschätzung von Pflegebedürftigkeit. In: Reuschenbach B, Mahler C (eds) Pflegebezogene Assessmentinstrumente. Internationales Handbuch für Pflegeforschung und- praxis. Verlag Hans Huber, Hogrefe, Bern, p 632
Lubke N, Meinck M, Von Renteln-Kruse W (2004) The Barthel Index in geriatrics. A context analysis for the Hamburg Classification Manual. Z Gerontol Geriatr 37(4):316–326. doi:10.1007/s00391-004-0233-2
Gandjour A, Ihle P, Schubert I (2008) Impact of demographic changes on health care expenditure in Germany: an analysis considering the expenditures of decedents. Gesundheitswesen 70(2):77–80. doi:10.1055/s-2008-1046774
Boeckxstaens P, De Graaf P (2011) Primary care and care for older persons: position paper of the European forum for primary care. Quality Prim Care 19(6):369–389
Medizinischer Dienst der Spitzenverbñde der Krankenkassen (2005) Richtlinien/Erhebungsbogen/MDK-Anleitungen : Grundlagen der MDK-Qualitätsprüfungen in der häuslichen Pflege; Grundlagen der Begutachtung. Spitzenverbände der Krankenkassen, Essen
Blinkert B, Klie T (2006) Investment of time in long-term care. Z Gerontol Geriatr 39(3):202–210. doi:10.1007/s00391-006-0387-1
Büscher A, Budroni H, Hartenstein A, Holle B, Vosseler B (2007) Auswirkungen von Vergütungsregelungen in der häuslichen Pflege. Ein Modellprojekt zur Einführung personenbezogener Budgets. Pflege and Gesellschaft 12.Jg. (4):343–359
Pohl C (2006) On reform of nursing insurance. The position of the German Professional Society for nursing affairs. Pflege aktuell/DBfK Deutscher Berufsverband fur Pflegeberufe 60:186–189
Grass-Kapanke B, Kunczik T, Gutzmann H (2008) Studie zur Demenzversorgung im ambulanten Sektor–DIAS. Schriftenreihe der Deutschen Gesellschaft f*r Gerontopsychiatrie und–psychotherapie (DGGPP), vol 7, 1. Aufl. edn. DGGPP, Berlin
Wade DT, Collin C (1988) The Barthel ADL Index: a standard measure of physical disability? Internatl Disability Stud 10(2):64–67
Maidhof R, Schneider F, Rachold U, Gerber J, Niehoff JU, Sann J (2002) The “Barthel Index”: alternative to expertising in compulsory care insurance? Gesundheitswesen 64(1):54–59. doi:10.1055/s-2002-19506
Della Pietra GL, Savio K, Oddone E, Reggiani M, Monaco F, Leone MA (2011) Validity and reliability of the Barthel Index administered by telephone. Stroke J Cereb Circ 42(7):2077–2079. doi:10.1161/STROKEAHA.111.613521
Oveisgharan S, Shirani S, Ghorbani A, Soltanzade A, Baghaei A, Hosseini S, Sarrafzadegan N (2006) Barthel Index in a Middle-East country: translation, validity and reliability. Cerebrovasc Dis 22(5–6):350–354. doi:10.1159/000094850
Tukey JW (1977) Some thoughts on clinical trials, especially problems of multiplicity. Science 198(4318):679–684
Bundesamt DS (2013) Pflegestatistik 2011 : Pflege im Rahmen der Pflegeversicherung Ländervergleich—Pflegebedürftige. Januar 2013 edn. Statistisches Bundesamt, Bonn
Gattinger H, Ott S, Saxer S (2014) Nursin Care Assessments BESA and RAI: comparison of Outcomes in Minutes. Pflege 27(1):31–40. doi:10.1024/1012-5302/a000337
Miranda-Castillo C, Woods B, Orrell M (2010) People with dementia living alone: what are their needs and what kind of support are they receiving? Internatl Psychogeriatrics/IPA 22(4):607–617. doi:10.1017/S104161021000013X
Becher K, Oelke M, Grass-Kapanke B, Flohr J, Mueller EA, Papenkordt U, Schulte-Frei B, Steinwachs KC, Suss S, Wehling M (2013) Improving the health care of geriatric patients: management of urinary incontinence: a position paper. Z Gerontol Geriatr 46(5):456–464. doi:10.1007/s00391-013-0491-y
Tariq SH, Morley JE, Prather CM (2003) Fecal incontinence in the elderly patient. Am j Med 115(3):217–227
Chromy J, Abeyasekera S (2005) Chapter 19—Statistical analysis of survey data. Household surveys in developing and transition countries. United Nations, New York
Inouye SK, Studenski S, Tinetti ME, Kuchel GA (2007) Geriatric syndromes: clinical, research, and policy implications of a core geriatric concept. J Am Geriatr Soc 55(5):780–791. doi:10.1111/j.1532-5415.2007.01156.x
Conflict of interest
We certify that there is no conflict of interest with any financial organization regarding the material discussed in the manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
N. A. Lahmann and R. Suhr shared first authorship.
Box 1 level of care
Box 1 level of care
For the assignment to a specific level of care, the requirements can be distinguished:
-
1.
Basic care regarding nutrition, mobility and hygiene
-
2.
Household assistance (e.g. cleaning up the room, shopping food and cook the meal, etc.).
Stage of care | Benefits in Euro | Minimum time | Care requirements |
|---|---|---|---|
Level 0 (with dementia) | 225 | 45 min daily | Care and observation necessary |
Level 1 | 450 | Daily 90 min | Minimum of support in two areas of basic care + household assistance |
Level 1 (with dementiaa) | 665 | ||
Level 2 | 1,100 | 3 h/day → to assume that 2 h/day for basic care | Minimum three times daily assistance in basic care + household assistance multiple times/week |
Level 2 (with dementia a) | 1,250 | ||
Level 3 | 1,550 | 5 h/day → to assume that 4 h/day for basic care | Five times a day support + household assistance multiple times/week |
Level 3+ | 1,918 | Additional support at night (usually only in nursing homes) |
Rights and permissions
About this article
Cite this article
Lahmann, N.A., Suhr, R., Kuntz, S. et al. Over- and undersupply in home care: a representative multicenter correlational study. Aging Clin Exp Res 27, 209–219 (2015). https://doi.org/10.1007/s40520-014-0267-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-014-0267-2