Abstract
Background
Drug-related problems are an important healthcare safety concern in the growing population of older people. Prescription of potentially inappropriate medication (PIM) is one aspect of this concern that is considered to increase the risk of adverse health outcomes.
Objective
The aim of the Health Economics of Potentially Inappropriate Medication (HEPIME) study was to analyze the association between the prescription of PIMs according to the German PRISCUS list and healthcare utilization, healthcare costs, and the occurrence of adverse events in old age.
Methods
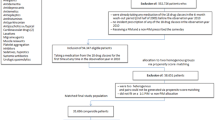
Insurants of a large German health insurance company aged 65+ years were included in a retrospective matched cohort study. A total of 3,953,423 individuals with no exposure to PIM in 2011 were matched to 521,644 exposed individuals and compared in terms of outpatient healthcare utilization, healthcare costs, and the occurrence of adverse events in outpatient, hospital, and rehabilitation sectors during a 12-month follow-up.
Results
On average, individuals in the exposed group had additional 143 [95% confidence interval (CI) 140–146] daily defined doses of pharmaceuticals and 4.5 (95% CI 4.4–4.6) days in hospital. Mean annual total healthcare costs per individual in the exposed group exceeded those in the non-exposed group by €2321 (95% CI 2269–2372), resulting mainly from differences in hospitalization costs of €1718 (95% CI 1678–1759). Odds ratios for the occurrence of adverse events in the exposed group were 1.32 (95% CI 1.32–1.34) in the outpatient sector, 1.76 (95% CI 1.73–1.79) in the hospital sector, and 1.82 (95% CI 1.76–1.89) in the rehabilitation sector.
Conclusions
Increased healthcare utilization and costs as well as an increased probability for adverse events in individuals exposed to PIM demonstrate the health economic relevance of PIM prescriptions. Whether avoiding PIM listed on the PRISCUS list may potentially improve the quality and efficiency of healthcare is currently unknown.

Similar content being viewed by others
References
Bundesamt Statistisches, editor. Bevökerung Deutschlands bis 2060: 12. Koordinierte Bevölkerungsvorausberechnung12. Wiesbaden: Statistisches Bundesamt; 2009.
van den Akker M, Buntinx F, Metsemakers JF, et al. Multimorbidity in general practice: prevalence, incidence, and determinants of co-occurring chronic and recurrent diseases. J Clin Epidemiol. 1998;51:367–75.
van den Bussche H, Koller D, Kolonko T, et al. Which chronic diseases and disease combinations are specific to multimorbidity in the elderly? Results of a claims data based cross-sectional study in Germany. BMC Public Health. 2011;11:101.
Schaufler J, Telschow C. Arzneimittelverordnungen nach Alter und Geschlecht. In: Schwab U, Paffrath D, editors. Arzneiverordnungsreport 2013. Heidelberg: Springer Medizin; 2013.
Corsonello A, Pedone C, Incalzi RA. Age-related pharmacokinetic and pharmacodynamic changes and related risk of adverse drug reactions. Curr Med Chem. 2010;17:571–84.
Schneeweiss S, Hasford J, Göttler M, et al. Admissions caused by adverse drug events to internal medicine and emergency departments in hospitals: a longitudinal population-based study. Eur J Clin Pharmacol. 2002;58:285–91.
Fick DM, Mion LC, Beers MH, et al. Health outcomes associated with potentially inappropriate medication use in older adults. Res Nurs Health. 2008;31:42–51.
Zint K, Haefeli WE, Glynn RJ, et al. Impact of drug interactions, dosage, and duration of therapy on the risk of hip fracture associated with benzodiazepine use in older adults. Pharmacoepidemiol Drug Saf. 2010;19:1248–55.
Cancelli I, Beltrame M, Gigli GL, et al. Drugs with anticholinergic properties: cognitive and neuropsychiatric side-effects in elderly patients. Neurol Sci. 2009;30:87–92.
Beers MH, Ouslander JG, Rollingher I, et al. Explicit criteria for determining inappropriate medication use in nursing home residents: UCLA Division of Geriatric Medicine. Arch Intern Med. 1991;151:1825–32.
Fick D, Cooper J, Wade W, et al. Updating the Beers criteria for potentially inappropriate medication use in older adults: results of a US consensus panel of experts. Arch Intern Med. 2003;163:2716–24.
Laroche M-L, Charmes J-P, Merle L. Potentially inappropriate medications in the elderly: a French consensus panel list. Eur J Clin Pharmacol. 2007;63:725–31.
Rognstad S, Brekke M, Fetveit A, et al. The Norwegian General Practice (NORGEP) criteria for assessing potentially inappropriate prescriptions to elderly patients: a modified Delphi study. Scand J Prim Health Care. 2009;27:153–9.
Holt S, Schmiedl S, Thürmann PA. Potentially inappropriate medications in the elderly: the PRISCUS list. Dtsch Arztebl Int. 2010;107:543–51.
Amann U, Schmedt N, Garbe E. Prescribing of potentially inappropriate medications for the elderly. Dtsch Arztebl Int. 2012;109:69–75.
Fu AZ, Liu GG, Christensen DB. Inappropriate medication use and health outcomes in the elderly. J Am Geriatr Soc. 2004;52:1934–9.
Fu AZ, Jiang JZ, Reeves JH, et al. Potentially inappropriate medication use and healthcare expenditures in the US community-dwelling elderly. Med Care. 2007;45:472–6.
Stockl KM, Le L, Zhang S, et al. Clinical and economic outcomes associated with potentially inappropriate prescribing in the elderly. Am J Manag Care. 2010;16:e1–10.
Hyttinen V, Jyrkkä J, Valtonen H. A systematic review of the impact of potentially inappropriate medication on health care utilization and costs among older adults. Med Care. 2016;54:950–64.
Hefner G, Stieffenhofer V, Gabriel S, et al. Side effects related to potentially inappropriate medications in elderly psychiatric patients under everyday pharmacotherapy. Eur J Clin Pharmacol. 2015;71:165–72.
Montastruc F, Duguet C, Rousseau V, et al. Potentially inappropriate medications and adverse drug reactions in the elderly: a study in a PharmacoVigilance database. Eur J Clin Pharmacol. 2014;70:1123–7.
Onda M, Imai H, Takada Y, et al. Identification and prevalence of adverse drug events caused by potentially inappropriate medication in homebound elderly patients: a retrospective study using a nationwide survey in Japan. BMJ Open. 2015;5:e007581.
Endres HG, Kaufmann-Kolle P, Steeb V, et al. Association between potentially inappropriate medication (PIM) use and risk of hospitalization in older adults: an observational study based on routine data comparing PIM use with use of PIM alternatives. PLoS One. 2016;11:e0146811.
Wehling M, Burkhardt H, Kuhn-Thiel A, et al. VALFORTA: a randomised trial to validate the FORTA (Fit fOR The Aged) classification. Age Ageing. 2016;45:262–7.
Hainmueller J. Entropy balancing for causal effects: a multivariate reweighting method to produce balanced samples in observational studies. Polit Anal. 2012;20:25–46.
World Health Organization. Guidelines for ATC classification and DDD assignment 2016. Oslo: World Health Organization; 2016.
Quinzler R, Schmitt SPW, Szecsenyi J, et al. Optimizing information on drug exposure by collection of package code information in questionnaire surveys. Pharmacoepidemiol Drug Saf. 2007;16:1024–30.
Aronson JK. Meyler’s side effects of drugs: the international encyclopedia of adverse drug reactions and interactions. 15th edn. Amsterdam, Boston: Elsevier; 2006.
World Health Organization. International statistical classification of diseases and related health problems. Tenth Revision, German Modification. Geneva: World Health Organization; 1992.
Elixhauser A, Steiner C, Harris DR, et al. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27.
Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130–9.
van Walraven C, Austin PC, Jennings A, et al. A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Med Care. 2009;47:626–33.
Roy AD. Some thoughts on the distribution of earnings. Oxf Econ Pap. 1951;3:135–46.
Rubin DB. Estimating causal effects of treatments in randomized and nonrandomized studies. J Educ Psychol. 1974;66:688–701.
Eggers AC, Fowler A, Hainmueller J, et al. On the validity of the regression discontinuity design for estimating electoral effects: new evidence from over 40,000 close races. Am J Polit Sci. 2015;59:259–74.
Hainmueller J, Xu J. ebalance: a STATA package for entropy balancing. J Stat Softw. 2013;54:1–18.
StataCorp. Stata statistical software: Release 14. College Station, TX: StataCorp; 2015.
Greene WH. Econometric analysis. International ed. ed. Edinburgh Gate, Harlow: Pearson Education Limited; 2012.
Wooldridge J. Econometric analysis of cross section and panel data, vol. 2. Cambridge: The MIT Press; 2010.
Schrijvers G. Disease management: a proposal for a new definition. Int J Integr Care. 2009;9:e06.
Bradley MC, Fahey T, Cahir C, et al. Potentially inappropriate prescribing and cost outcomes for older people: a cross-sectional study using the Northern Ireland Enhanced Prescribing Database. Eur J Clin Pharmacol. 2012;68:1425–33.
Dedhiya SD, Hancock E, Craig BA, et al. Incident use and outcomes associated with potentially inappropriate medication use in older adults. Am J Geriatr Pharmacother. 2010;8:562–70.
Akazawa M, Imai H, Igarashi A, et al. Potentially inappropriate medication use in elderly Japanese patients. Am J Geriatr Pharmacother. 2010;8:146–60.
Lund BC, Schroeder MC, Middendorff G, et al. Effect of hospitalization on inappropriate prescribing in elderly Medicare beneficiaries. J Am Geriatr Soc. 2015;63:699–707.
Schnee M. Sozioökonomische Strukturen und Morbidität in den gesetzlichen Krankenkassen. In: Böcken J, Braun B, Amhof R, editors. Gesundheitsmonitor 2008. Gesundheitsversorgung und Gestaltungsoptionen aus der Perspektive der Bevölkerung. Gütersloh: Verlag Bertelsmann-Stiftung; 2008. p. 88–104.
Vega CP. PIMs: the real senior drug problem. Medscape. http://www.medscape.com/viewarticle/802898. Accessed 8 Feb 2016.
Hanlon JT, Weinberger M, Samsa GP, et al. A randomized, controlled trial of a clinical pharmacist intervention to improve inappropriate prescribing in elderly outpatients with polypharmacy. Am J Med. 1996;100:428–37.
Lang PO, Vogt-Ferrier N, Hasso Y, et al. Interdisciplinary geriatric and psychiatric care reduces potentially inappropriate prescribing in the hospital: interventional study in 150 acutely ill elderly patients with mental and somatic comorbid conditions. J Am Med Dir Assoc. 2012;13(406):e1–7.
Acknowledgements
We thank Florian Bleibler (Department of Health Economics and Health Services Research, University Medical Center Hamburg-Eppendorf) for suggesting the application of the entropy balancing procedure.
Author Contributions
All authors made substantial contributions to the conception and design of the work, and the acquisition and interpretation of data for the work. DH and J-BA prepared the data. DH and HM conducted the data analysis. DH and H-HK drafted the work and all authors revised it critically for important intellectual content and approved the final version for submission. All authors agreed to be accountable for all aspects of the work and ensuring that questions related to the accuracy or integrity of any part of the work were appropriately investigated and resolved. DH and HM had full access to the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. DH is the study guarantor.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The HEPIME study was funded by the Federal Ministry of Education and Research (BMBF) under Project No. 01GY1329A.
Conflict of interest
Walter E. Haefeli is a member of the scientific advisory board and a shareholder of Dosing GmbH, the company distributing the clinical decision support software used in this study. His wife is an employee of Dosing GmbH. Dirk Heider, Herbert Matschinger, Andreas Meid, Renate Quinzler, Jürgen-Bernhard Adler, Christian Günster, and Hans-Helmut König declare that they have no conflicts of interest relevant to this study.
Transparency
The lead author affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been disclosed.
Ethics approval
For this type of study, formal consent is not required.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Heider, D., Matschinger, H., Meid, A.D. et al. Health Service Use, Costs, and Adverse Events Associated with Potentially Inappropriate Medication in Old Age in Germany: Retrospective Matched Cohort Study. Drugs Aging 34, 289–301 (2017). https://doi.org/10.1007/s40266-017-0441-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-017-0441-2