Abstract
Objectives
Early broad-spectrum antimicrobial treatment reduces mortality in patients with septic shock. In a multicenter, prospective observational study, we explored whether delayed appropriate antimicrobial therapy (AAT) influences outcome in Staphylococcus aureus bloodstream infection (SAB).
Methods
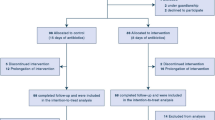
Two hundred and fifty-six patients with SAB from ten German study centers were enrolled and followed for 3 months. Predisposing factors, clinical features, diagnostic procedures, antimicrobial therapy, and outcome were recorded. The appropriateness of antimicrobial therapy was judged by a trained physician based on in vitro activity, dosage, and duration of therapy. Therapy was considered to be delayed when more than 24 h elapsed between the first positive blood culture and the start of appropriate therapy. The association of delayed therapy with overall mortality and SAB-related events (i.e., attributable mortality or late SAB-related complications) was assessed by crosstabulation and propensity score-based logistic regression.
Results
One hundred and sixty-eight patients received AAT during their hospital stay, of whom 42 (25 %) received delayed AAT. The overall mortality and the occurrence of severe sepsis or septic shock were lower in patients with delayed AAT, pointing towards confounding by indication. Adjusted 90-day mortality (adjusted odds ratio [OR] 0.91, 95 % confidence interval [CI] [0.39–2.13], p 0.82) and SAB-related events (adjusted OR 1.46, 95 % CI [0.47–4.51], p 0.52) also failed to show a significant impact of delayed AAT on outcome.
Conclusion
In patients with SAB, early AAT may not improve survival. However, confounding by indication is a major challenge when analyzing and interpreting observational studies on the impact of delayed AAT.


Similar content being viewed by others
References
Kumar A, Roberts D, Wood KE, Light B, Parrillo JE, Sharma S, et al. Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med. 2006;34:1589–96.
Lipman J, Boots R. A new paradigm for treating infections: “go hard and go home”. Crit Care Resusc. 2009;11:276–81.
Ammerlaan H, Seifert H, Harbarth S, Brun-Buisson C, Torres A, Antonelli M, et al. Adequacy of antimicrobial treatment and outcome of Staphylococcus aureus bacteremia in 9 Western European countries. Clin Infect Dis. 2009;49:997–1005.
European Antimicrobial Resistance Surveillance Network (EARS-Net) Database. RIVM, Bilthoven, the Netherlands. 2011. http://www.ecdc.europa.eu/en/activities/surveillance/EARS-Net/database/Pages/database.aspx. Accessed 15 Jan 2013.
Kreisel K, Boyd K, Langenberg P, Roghmann MC. Risk factors for recurrence in patients with Staphylococcus aureus infections complicated by bacteremia. Diagn Microbiol Infect Dis. 2006;55:179–84.
Lodise TP, McKinnon PS, Swiderski L, Rybak MJ. Outcomes analysis of delayed antibiotic treatment for hospital-acquired Staphylococcus aureus bacteremia. Clin Infect Dis. 2003;36:1418–23.
Gómez J, García-Vázquez E, Baños R, Canteras M, Ruiz J, Baños V, et al. Predictors of mortality in patients with methicillin-resistant Staphylococcus aureus (MRSA) bacteraemia: the role of empiric antibiotic therapy. Eur J Clin Microbiol Infect Dis. 2007;26:239–45.
Soriano A, Marco F, Martínez JA, Pisos E, Almela M, Dimova VP, et al. Influence of vancomycin minimum inhibitory concentration on the treatment of methicillin-resistant Staphylococcus aureus bacteremia. Clin Infect Dis. 2008;46:193–200.
Rodríguez-Baño J, Millán AB, Domínguez MA, Borraz C, González MP, Almirante B, et al. Impact of inappropriate empirical therapy for sepsis due to health care-associated methicillin-resistant Staphylococcus aureus. J Infect. 2009;58:131–7.
Paul M, Kariv G, Goldberg E, Raskin M, Shaked H, Hazzan R, et al. Importance of appropriate empirical antibiotic therapy for methicillin-resistant Staphylococcus aureus bacteraemia. J Antimicrob Chemother. 2010;65:2658–65.
Marchaim D, Kaye KS, Fowler VG, Anderson DJ, Chawla V, Golan Y, et al. Case–control study to identify factors associated with mortality among patients with methicillin-resistant Staphylococcus aureus bacteraemia. Clin Microbiol Infect. 2010;16:747–52.
Roghmann MC. Predicting methicillin resistance and the effect of inadequate empiric therapy on survival in patients with Staphylococcus aureus bacteremia. Arch Intern Med. 2000;160:1001–4.
Kim SH, Park WB, Lee KD, Kang CI, Bang JW, Kim HB, et al. Outcome of inappropriate initial antimicrobial treatment in patients with methicillin-resistant Staphylococcus aureus bacteraemia. J Antimicrob Chemother. 2004;54:489–97.
Kim SH, Park WB, Lee CS, Kang CI, Bang JW, Kim HB, et al. Outcome of inappropriate empirical antibiotic therapy in patients with Staphylococcus aureus bacteraemia: analytical strategy using propensity scores. Clin Microbiol Infect. 2006;12:13–21.
Schweizer ML, Furuno JP, Harris AD, Johnson JK, Shardell MD, McGregor JC, et al. Empiric antibiotic therapy for Staphylococcus aureus bacteremia may not reduce in-hospital mortality: a retrospective cohort study. PLoS One. 2010;5:e11432.
Asgeirsson H, Kristjansson M, Kristinsson KG, Gudlaugsson O. Staphylococcus aureus bacteraemia—nationwide assessment of treatment adequacy and outcome. J Infect. 2011;62:339–46.
Friedman ND, Kaye KS, Stout JE, McGarry SA, Trivette SL, Briggs JP, et al. Health care-associated bloodstream infections in adults: a reason to change the accepted definition of community-acquired infections. Ann Intern Med. 2002;137:791–7.
[No authors listed]. American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference: definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Crit Care Med. 1992;20:864–74.
Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R, et al. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2008. Crit Care Med. 2008;36:296–327.
Fraser A, Paul M, Almanasreh N, Tacconelli E, Frank U, Cauda R, et al. Benefit of appropriate empirical antibiotic treatment: thirty-day mortality and duration of hospital stay. Am J Med. 2006;119:970–6.
Garnacho-Montero J, Garcia-Garmendia JL, Barrero-Almodovar A, Jimenez-Jimenez FJ, Perez-Paredes C, Ortiz-Leyba C. Impact of adequate empirical antibiotic therapy on the outcome of patients admitted to the intensive care unit with sepsis. Crit Care Med. 2003;31:2742–51.
Lodise TP Jr, Patel N, Kwa A, Graves J, Furuno JP, Graffunder E, et al. Predictors of 30-day mortality among patients with Pseudomonas aeruginosa bloodstream infections: impact of delayed appropriate antibiotic selection. Antimicrob Agents Chemother. 2007;51:3510–5.
Vallés J, Rello J, Ochagavía A, Garnacho J, Alcalá MA. Community-acquired bloodstream infection in critically ill adult patients: impact of shock and inappropriate antibiotic therapy on survival. Chest. 2003;123:1615–24.
Fang CT, Shau WY, Hsueh PR, Chen YC, Wang JT, Hung CC, et al. Early empirical glycopeptide therapy for patients with methicillin-resistant Staphylococcus aureus bacteraemia: impact on the outcome. J Antimicrob Chemother. 2006;57:511–9.
Khatib R, Saeed S, Sharma M, Riederer K, Fakih MG, Johnson LB. Impact of initial antibiotic choice and delayed appropriate treatment on the outcome of Staphylococcus aureus bacteremia. Eur J Clin Microbiol Infect Dis. 2006;25:181–5.
Park SY, Son JS, Oh IH, Choi JM, Lee MS. Clinical impact of methicillin-resistant Staphylococcus aureus bacteremia based on propensity scores. Infection. 2011;39:141–7.
Kaasch AJ, Rieg S, Neumann S, Seifert H, Kern WV. Measuring mortality in Staphylococcus aureus bloodstream infections: are 3 months of follow-up enough? Infection. 2011;39:281–2.
Yzerman EP, Boelens HA, Tjhie JH, Kluytmans JA, Mouton JW, Verbrugh HA. Delta APACHE II for predicting course and outcome of nosocomial Staphylococcus aureus bacteremia and its relation to host defense. J Infect Dis. 1996;173:914–9.
Enoch DA, Cargill JS, Laing R, Herbert S, Corrah TW, Brown NM. Value of CT-guided biopsy in the diagnosis of septic discitis. J Clin Pathol. 2008;61:750–3.
Itani KM, Akhras KS, Stellhorn R, Quintana A, Budd D, Merchant S. Outcomes associated with initial versus later vancomycin use in patients with complicated skin and skin-structure infections. Pharmacoeconomics. 2009;27:421–30.
Bauer KA, West JE, Balada-Llasat JM, Pancholi P, Stevenson KB, Goff DA. An antimicrobial stewardship program’s impact with rapid polymerase chain reaction methicillin-resistant Staphylococcus aureus/S. aureus blood culture test in patients with S. aureus bacteremia. Clin Infect Dis. 2010;51:1074–80.
Acknowledgments
Data acquisition was supported by H. Birkholz (University of Cologne), M. Gensler (Saarland University Hospital, Homburg), M. Holl (University Hospital Ulm), G. Peyerl-Hofmann (University Hospital Freiburg), and C. Feind (University Hospital Düsseldorf). This study was mainly funded by the Deutsche Forschungsgemeinschaft (DFG, grant number KA 3104/1-1 to A.J.K.). The following individuals received support from the German Federal Ministry of Education and Research: A.J.K, S.R., P.K., F.M.B.; grant number BMBF 01KI1017, 01EO0803, 01KI0772, and 01EO1002, respectively. F.M.B. was supported by the Thuringian Ministry of Education, Science and Culture (PE 108-2), the Thuringian Foundation for Technology, Innovation and Research (STIFT), and the German Sepsis Society (GSS). B.S. was supported by the DFG (IRTG1522, SFB-TR34). The funding agencies did not have any role in the study design, collection, analysis, and interpretation of data, in the writing of the manuscript, or in the decision to submit the manuscript for publication.
Conflict of interest
All authors none to declare.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
* This article was written by members of the preSABATO study group. Other members of this study group, who collaborated to this research, are: C. MacKenzie (University Hospital Düsseldorf, Düsseldorf, Germany), C. Bogdan (University Hospital Erlangen, Erlangen, Germany), G. Häcker, C. Schneider (University Hospital of Freiburg, Freiburg, Germany), T. Wichelhaus, J. Kessel (J. W. Goethe University Hospital, Frankfurt, Frankfurt, Germany), S. Ziesing (Hannover Medical School, Hannover, Germany), L. von Müller (Saarland University Hospital, Homburg, Homburg Germany), and S. Stenger (University Hospital Ulm, Ulm, Germany).
Rights and permissions
About this article
Cite this article
Kaasch, A.J., Rieg, S., Kuetscher, J. et al. Delay in the administration of appropriate antimicrobial therapy in Staphylococcus aureus bloodstream infection: a prospective multicenter hospital-based cohort study. Infection 41, 979–985 (2013). https://doi.org/10.1007/s15010-013-0428-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-013-0428-9