Abstract
Purpose
This study aims at extending current knowledge on consequences of informal caregiving by analyzing the influence of different caregiving types on mental, physical, and self-rated health longitudinally.
Methods
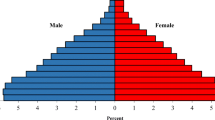
Data from wave 2008, 2011, and 2014 of the nationally representative German Ageing Survey were used, drawing on 16,412 observations aged 40–95 years in fixed effects (FE) regression analyses. Three informal caregiving types (helping around the house, looking after someone, nursing care services), which we used as explanatory variables and four health outcomes (depressive symptoms, self-rated health, pulmonary function, and morbidity), were assessed with structured interviews and written questionnaires. FE regression analysis was used for our calculations.
Results
Results revealed that none of the caregiving types was significantly associated with pulmonary function or morbidity. However, helping around the house and looking after someone were significantly associated with increased depressive symptoms. Additionally, all three types of informal caregiving were significantly associated with decreased self-rated health.
Conclusion
The results of this study indicate that the impact of care on health differs. First, it differs in dependence on the health outcome focused; only mental and self-rated health are negatively associated with care. Second, the impact depends on the caregiving type performed. This knowledge might help to develop support options which are specific to the caregiving type and the health aspects in order to reduce negative health consequences.
Similar content being viewed by others
References
Heuchert, M., König, H. H., & Lehnert, T. (2016). Die Rolle von Präferenzen für Langzeitpflege in der sozialen Pflegeversicherung - Ergebnisse von Experteninterviews [The role of preferences in the german long-term care insurance - results from expert interviews]. Das Gesundheitswesen. https://doi.org/10.1055/s-0041-111839.
Lehnert, T., Heuchert, M. A. X., Hussain, K., & König, H.-H. (2018). Stated preferences for long-term care: A literature review. Ageing and Society. https://doi.org/10.1017/S0144686X18000314.
Hajek, A., Lehnert, T., Wegener, A., Riedel-Heller, S. G., & Konig, H. H. (2017). Factors associated with preferences for long-term care settings in old age: Evidence from a population-based survey in Germany. BMC Health Services Research, 17(1), 156. https://doi.org/10.1186/s12913-017-2101-y.
Lavela, S. L., & Ather, N. (2010). Psychological health in older adult spousal caregivers of older adults. Chronic Illness, 6(1), 67–80. https://doi.org/10.1177/1742395309356943.
Pinquart, M., & Sörensen, S. (2003). Differences between caregivers and noncaregivers in psychological health and physical health: A meta-analysis. Psychology and Aging, 18(2), 250–267.
Schulz, R., O’Brien, A. T., Bookwala, J., & Fleissner, K. (1995). Psychiatric and physical morbidity effects of dementia caregiving: Prevalence, correlates, and causes. The Gerontologist, 35(6), 771–791. https://doi.org/10.1093/geront/35.6.771.
Berglund, E., Lytsy, P., & Westerling, R. (2015). Health and wellbeing in informal caregivers and non-caregivers: A comparative cross-sectional study of the Swedish general population. Health and Quality of Life Outcomes, 13, 109. https://doi.org/10.1186/s12955-015-0309-2.
Vitaliano, P. P., Zhang, J., & Scanlan, J. M. (2003). Is caregiving hazardous to one’s physical health? A meta-analysis. Psychological Bulletin, 129(6), 946–972. https://doi.org/10.1037/0033-2909.129.6.946.
Allen, A. P., Curran, E. A., Duggan, A., Cryan, J. F., Chorcorain, A. N., Dinan, T. G., et al. (2016). A systematic review of the psychobiological burden of informal caregiving for patients with dementia: Focus on cognitive and biological markers of chronic stress. Neuroscience and Biobehavioral Reviews, 73, 123–164. https://doi.org/10.1016/j.neubiorev.2016.12.006.
Wimo, A., & Nordberg, G. (2007). Validity and reliability of assessments of time: Comparisons of direct observations and estimates of time by the use of the resource utilization in dementia (RUD)-instrument. Archives of Gerontology and Geriatrics, 44(1), 71–81. https://doi.org/10.1016/j.archger.2006.03.001.
Garand, L., Dew, M. A., Eazor, L. R., DeKosky, S. T., & Reynolds, C. F., III (2005). Caregiving burden and psychiatric morbidity in spouses of persons with mild cognitive impairment. International Journal of Geriatric Psychiatry, 20(6), 512–522. https://doi.org/10.1002/gps.1318.
Hirst, M. A. (2005). Carer distress: A prospective, population-based study. Social Science & Medicine, 61(3), 697–708. https://doi.org/10.1016/j.socscimed.2005.01.001.
Coe, N. B., & van Houtven, C. H. (2009). Caring for mom and neglecting yourself? The health effects of caring for an elderly parent. Health Economics, 18(9), 991–1010. https://doi.org/10.1002/hec.1512.
Heger, D. (2016). The mental health of children providing care to their elderly parent. Health Economics. https://doi.org/10.1002/hec.3457.
Kaschowitz, J., & Brandt, M. (2017). Health effects of informal caregiving across Europe: A longitudinal approach. Social Science & Medicine, 173, 72–80. https://doi.org/10.1016/j.socscimed.2016.11.036.
Hiel, L., Beenackers, M. A., Renders, C. M., Robroek, S. J., Burdorf, A., & Croezen, S. (2015). Providing personal informal care to older European adults: Should we care about the caregivers’ health? Preventive Medicine, 70, 64–68. https://doi.org/10.1016/j.ypmed.2014.10.028.
Kiecolt-Glaser, J. K., Dura, J. R., Speicher, C. E., Trask, O. J., & Glaser, R. (1991). Spousal caregivers of dementia victims: Longitudinal changes in immunity and health. Psychosomatic Medicine, 53(4), 345–362. https://doi.org/10.1097/00006842-199107000-00001.
Miyawaki, A., Tomio, J., Kobayashi, Y., Takahashi, H., Noguchi, H., & Tamiya, N. (2017). Impact of long-hours family caregiving on non-fatal coronary heart disease risk in middle-aged people: Results from a longitudinal nationwide survey in Japan. Geriatrics & Gerontology International, 17(11), 2109–2115. https://doi.org/10.1111/ggi.13061.
Ory, M. G., Hoffman, R. R., III, Yee, J. L., Tennstedt, S., & Schulz, R. (1999). Prevalence and impact of caregiving: A detailed comparison between dementia and nondementia caregivers. The Gerontologist, 39(2), 177–185. https://doi.org/10.1093/geront/39.2.177.
Salive, M. E. (2013). Multimorbidity in older adults. Epidemiologic Reviews, 35(1), 75–83. https://doi.org/10.1093/epirev/mxs009.
Klaus, D., Engstler, H., Mahne, K., Wolff, J. K., Simonson, J., Wurm, S., et al. (2017). Cohort profile: The German ageing survey (DEAS). International Journal of Epidemiology, 46(4), 1105–1105g. https://doi.org/10.1093/ije/dyw326.
Klaus, D., & Engstler, H. (2017). Daten und Methoden des Deutschen Alterssurveys [Data and methods of the German Ageing Survey]. In K. Mahne, J. K. Wolff, J. Simonson & C. Tesch-Römer (Eds.), Altern im Wandel: Zwei Jahrzehnte Deutscher Alterssurvey (DEAS) [Ageing in social change: Two decades of the German Ageing Survey (DEAS)] (pp. 29–45). Wiesbaden: Springer.
German Research Foundation. (2010–2017). Informationen für Geistes- und Sozialwissenschaftler/innen [Information for humanities and social scientists]. Accessed May 9, 2017, from http://www.dfg.de/foerderung/faq/geistes_sozialwissenschaften/.
Wurm, S., Tesch-Romer, C., & Tomasik, M. J. (2007). Longitudinal findings on aging-related cognitions, control beliefs, and health in later life. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 62(3), P156–P164.
Quail, J. M., Lix, L. M., Osman, B. A., & Teare, G. F. (2011). Comparing comorbidity measures for predicting mortality and hospitalization in three population-based cohorts. BMC Health Services Research, 11(1), 146. https://doi.org/10.1186/1472-6963-11-146.
Nunn, A. J., & Gregg, I. (1989). New regression equations for predicting peak expiratory flow in adults. The BMJ, 298(6680), 1068–1070. https://doi.org/10.1136/bmj.298.6680.1068.
Roberts, M. H., & Mapel, D. W. (2012). Limited lung function: Impact of reduced peak expiratory flow on health status, health-care utilization, and expected survival in older adults. American Journal of Epidemiology, 176(2), 127–134. https://doi.org/10.1093/aje/kwr503.
Hautzinger, M., & Bailer, M. (1993). ADS - Allgemeine Depressions Skala [ADS - General Depression Scale]. Weinheim: Beltz.
Fayers, P. M., & Sprangers, M. A. G. (2002). Understanding self-rated health. The Lancet, 359(9302), 187–188. https://doi.org/10.1016/S0140-6736(02)07466-4.
Zhu, C. W., Leibman, C., McLaughlin, T., Zbrozek, A. S., Scarmeas, N., Albert, M., et al. (2008). Patient dependence and longitudinal changes in costs of care in Alzheimer’s disease. Dementia and Geriatric Cognitive Disorders, 26(5), 416–423. https://doi.org/10.1159/000164797.
Bullinger, M., & Kirchberger, I. (1998). Der SF-36-Fragebogen zum Gesundheitszustand. Handanweisung [SF-36-Questionnaire on health status. Manual]. Göttingen: Hogrefe.
Morfeld, M., Kirchberger, I., & Bullinger, M. (2011). SF-36 Fragebogen zum Gesundheitszustand: Deutsche Version des Short Form-36 Health Survey [SF-36-Questionnaire on health status: German version of the Short Form-36 Health Survey]. Göttingen: Hogrefe.
Cameron, A. C., & Trivedi, P. K. (2009). Microeconometrics using stata (Vol. 5). College Station: Stata Press.
Brüderl, J., & Ludwig, V. (2015). Fixed-effects panel regression. In H. Best & C. Wolf (Eds.), The Sage handbook of regression analysis and causal inference (pp. 327–357). London: Sage.
Schaffer, M., & Stillman, S. (2016). XTOVERID: Stata module to calculate tests of overidentifying restrictions after xtreg, xtivreg, xtivreg2, xthtaylor.
Gangl, M. (2010). Causal inference in sociological research. Annual Review of Sociology, 36, 21–47.
Cossette, S., & Lévesque, L. (1993). Caregiving tasks as predictors of mental health of wife caregivers of men with chronic obstructive pulmonary disease. Research in Nursing & Health, 16(4), 251–263. https://doi.org/10.1002/nur.4770160404.
Schüz, B., Wurm, S., Schöllgen, I., & Tesch-Römer, C. (2011). What do people include when they self-rate their health? Differential associations according to health status in community-dwelling older adults. Quality of Life Research, 20(10), 1573–1580. https://doi.org/10.1007/s11136-011-9909-4.
Ekwall, A. K., Sivberg, B., & Hallberg, I. R. (2005). Loneliness as a predictor of quality of life among older caregivers. Journal of Advanced Nursing, 49(1), 23–32. https://doi.org/10.1111/j.1365-2648.2004.03260.x.
van Campen, C., de Boer, A. H., & Iedema, J. (2013). Are informal caregivers less happy than noncaregivers? Happiness and the intensity of caregiving in combination with paid and voluntary work. Scandinavian Journal of Caring Sciences, 27(1), 44–50. https://doi.org/10.1111/j.1471-6712.2012.00998.x.
Neller, K. (2005). Kooperation und Verweigerung: Eine Non-Response-Studie [Cooperation and refusal: A non-response study]. ZUMA Nachrichten, 29(57), 9–36.
Brüderl, J. (2010). Kausalanalyse mit Paneldaten [Causal analysis with panel data]. In C. Wolf & H. Best (Eds.), Handbuch der sozialwissenschaftlichen Datenanalyse [Social science data analysis handbook] (pp. 963–994). Wiesbaden: VS Verlag für Sozialwissenschaften.
Charlson, M. E., Pompei, P., Ales, K. L., & MacKenzie, C. R. (1987). A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. Journal of Chronic Diseases. https://doi.org/10.1016/0021-9681(87)90171-8.
Reichert, M. (2016). Vereinbarkeit von Erwerbstätigkeit und Pflege – (k)ein Thema für Unternehmen? In G. Naegele, E. Olbermann & A. Kuhlmann (Eds.), Teilhabe im Alter gestalten: Aktuelle Themen der Sozialen Gerontologie (pp. 251–264). Wiesbaden: Springer.
Höfner, R., & Meißner, T. (2008). Pflegerische Betreuungsformen [Types of nursing care]. In R. Höfner & T. Meißner (Eds.), Von Fall zu Fall — Ambulante Pflege im Recht: Rechtsfragen in der ambulanten Pflege von A-Z [As the case arises - Laws on Ambulatory Care: Legal questions about ambulatory care from A-Z] (pp. 195–199). Heidelberg: Springer.
Chien, L. Y., Chu, H., Guo, J. L., Liao, Y. M., Chang, L. I., Chen, C. H., et al. (2011). Caregiver support groups in patients with dementia: A meta-analysis. International Journal of Geriatric Psychiatry, 26(10), 1089–1098. https://doi.org/10.1002/gps.2660.
Ashworth, M., & Baker, A. H. (2000). ‘Time and space’: carers’ views about respite care. Health & Social Care in the Community, 8(1), 50–56. https://doi.org/10.1046/j.1365-2524.2000.00221.x.
van Exel, N. J. A., de Graaf, G., & Brouwer, W. B. F. (2007). Care for a break? An investigation of informal caregivers’ attitudes toward respite care using Q-methodology. Health Policy, 83(2–3), 332–342. https://doi.org/10.1016/j.healthpol.2007.02.002.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in this study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zwar, L., König, HH. & Hajek, A. Consequences of different types of informal caregiving for mental, self-rated, and physical health: longitudinal findings from the German Ageing Survey. Qual Life Res 27, 2667–2679 (2018). https://doi.org/10.1007/s11136-018-1926-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-018-1926-0