Abstract
Rising admissions from emergency departments (EDs) to hospitals are a primary concern for many healthcare systems. The issue of how to differentiate urgent admissions from non-urgent or even elective admissions is crucial. We aim to develop a model for classifying inpatient admissions based on a patient’s primary diagnosis as either emergency care or elective care and predicting urgency as a numerical value. We use supervised machine learning techniques and train the model with physician-expert judgments. Our model is accurate (96%) and has a high area under the ROC curve (>.99). We provide the first comprehensive classification and urgency categorization for inpatient emergency and elective care. This model assigns urgency values to every relevant diagnosis in the ICD catalog, and these values are easily applicable to existing hospital data. Our findings may provide a basis for policy makers to create incentives for hospitals to reduce the number of inappropriate ED admissions.





Similar content being viewed by others
Notes
For example, the NHS introduced the “marginal rate rule” in 2010 in response to growth in the volume of patients being admitted to the hospital as emergencies. The rule sets a baseline value for income from each provider’s emergency admissions. For emergency admissions above this baseline, the provider receives only 30% of the normal price [6, 7] regardless of urgency.
If a hospital treats more cases than negotiated with the SHI, it may receive reductions in the DRG payments for additional patients [23]. Therefore, it may be beneficial to code elective admissions as emergencies since every acute care hospital in Germany is required by law to admit all emergency cases unless it has reached capacity [24].
Urgency interpreted from greatest to least harm as a consequence of deferring treatment [29].
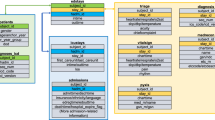
ICD and OPS codes were harmonized to the same version over the years using official mapping tables by DIMDI (German Institute of Medical Documentation and Information).
The operating definition of interaction is that variables m and k interact if a split on one variable, say m, in a tree makes a split on k either systematically less possible or more possible.
We have training data from all ICD chapters except for III (diseases of the blood and blood-forming organs and certain disorders involving the immune system), V (mental and behavioral disorders) and XX (external causes of morbidity and mortality), which together make up less than 5% of cases. We exclude chapter XV (pregnancy, childbirth and puerperium).
Additionally, superficial partial thickness (2nd degree a) has a lower urgency then deep partial thickness (2nd degree b).
Excluding maternity and birth.
For illustration purposes, we used logarithmic values for the hospital utilization in the lower part because of the steep age gradient.
The large increase of inpatient cases with a length of stay of <48 h in Germany is in line with this observation.
References
Morse A (2013) Emergency admissions to hospital: managing the demand. The Stationery Office, National Audit Office, London
Schuur JD, Venkatesh AK (2012) The growing role of emergency departments in hospital admissions. N Engl J Med 367(5):391–393. https://doi.org/10.1056/NEJMp1204431
Meacock R, Doran T, Sutton M (2015) What are the costs and benefits of providing comprehensive seven-day services for emergency hospital admissions? Health Econ 24(8):907–912. https://doi.org/10.1002/hec.3207
Roland M, Abel G (2012) Reducing emergency admissions: are we on the right track? BMJ 345:e6017. https://doi.org/10.1136/bmj.e6017
Wallace E, Smith SM, Fahey T, Roland M (2016) Reducing emergency admissions through community based interventions. BMJ 352:h6817. https://doi.org/10.1136/bmj.h6817
Macnabb J, Rowan L, Heneghan C, Onakpoya I (2014) How England's emergency departments are being penalised. BMJ 348:g1604. https://doi.org/10.1136/bmj.g1604
Monitor and NHS England (2013) Monitor and NHS England’s review of the marginal rate rules. Monitor and NHS England, London
Adan IJBF, Vissers JMH (2002) Patient mix optimisation in hospital admission planning: a case study. Int J Oper Prod Manag 22(4):445–461. https://doi.org/10.1108/01443570210420430
Mackway-Jones K, Marsden J, Windle J (2013) Emergency triages. Wiley, Chichester. https://doi.org/10.1002/9781118299029
Propper C, Sutton M, Whitnall C, Windmeijer F (2010) Incentives and targets in hospital care: evidence from a natural experiment. J Public Econ 94(3-4):318–335. https://doi.org/10.1016/j.jpubeco.2010.01.002
Wilper AP, Woolhandler S, Lasser KE, McCormick D, Cutrona SL, Bor DH, Himmelstein DU (2008) Waits to see an emergency department physician: U.S. trends and predictors, 1997-2004. Health Aff 27(2):w84–ww95. https://doi.org/10.1377/hlthaff.27.2.w84
Addison PD, Getgood A, Paterson-Brown S (2001) Separating elective and emergency surgical care (the emergency team). Scott Med J 46(2):48–50. https://doi.org/10.1177/003693300104600207
Blunt I, Bardsley M, Grove A, Clarke A (2015) Classifying emergency 30-days readmissions in England using routine hospital data 2004-2010: what is the scope for reduction? Emerg Med J 32(1):44–50. https://doi.org/10.1136/emermed-2013-202531
McCormack LA, Jones SG, Coulter SL (2016) Demographic factors influencing nonurgent emergency department utilization among a Medicaid population. Health Care Manag Sci 20(3):395–402. https://doi.org/10.1007/s10729-016-9360-8
Moskop JC, Sklar DP, Geiderman JM, Schears RM, Bookman KJ (2009) Emergency department crowding, part 2--barriers to reform and strategies to overcome them. Ann Emerg Med 53(5):612–617. https://doi.org/10.1016/j.annemergmed.2008.09.024
Pines JM, Hilton JA, Weber EJ, Alkemade AJ, Al Shabanah H, Anderson PD, Bernhard M, Bertini A, Gries A, Ferrandiz S, Kumar VA, Harjola VP, Hogan B, Madsen B, Mason S, Ohlén G, Rainer T, Rathlev N, Revue E, Richardson D, Sattarian M, Schull MJ (2011) International perspectives on emergency department crowding. Acad Emerg Med 18(12):1358–1370. https://doi.org/10.1111/j.1553-2712.2011.01235.x
Baker LC, Baker LS (1994) Excess cost of emergency department visits for nonurgent care. Health Aff 13(5):162–171. https://doi.org/10.1377/hlthaff.13.5.162
Cunningham PJ (2006) What accounts for differences in the use of hospital emergency departments across U.S. communities? Health Aff 25(5):w324–ww336. https://doi.org/10.1377/hlthaff.25.w324
Ballard DW, Price M, Fung V, Brand R, Reed ME, Fireman B, Newhouse JP, Selby JV, Hsu J (2010) Validation of an algorithm for categorizing the severity of hospital emergency department visits. Med Care 48(1):58–63. https://doi.org/10.1097/MLR.0b013e3181bd49ad
Weinick RM, Burns RM, Mehrotra A (2010) Many emergency department visits could be managed at urgent care centers and retail clinics. Health Aff 29(9):1630–1636. https://doi.org/10.1377/hlthaff.2009.0748
Young GP, Wagner MB, Kellermann AL, Ellis J, Bouley D (1996) Ambulatory visits to hospital emergency departments. Patterns and reasons for use. 24 hours in the ED study group. JAMA 276(6):460–465. https://doi.org/10.1001/jama.276.6.460
Johar M, Jones GS, Savage E (2013) Emergency admissions and elective surgery waiting times. Health Econ 22(6):749–756. https://doi.org/10.1002/hec.2849
Busse R, Geissler A, Quentin W (2011) Diagnosis-related groups in Europe: moving towards transparency, efficiency and quality in hospitals. McGraw-Hill Education, Maidenhead
Schwierz C, Augurzky B, Focke A, Wasem J (2012) Demand, selection and patient outcomes in German acute care hospitals. Health Econ 21(3):209–221. https://doi.org/10.1002/hec.1706
Schreyögg J, Bäuml M, Krämer J, Dette T, Busse R, Geissler A (2014) Forschungsauftrag zur Mengenentwicklung nach.§ 17 b Abs. 9 KHG. Endbericht Juli 2014s, Hamburg
Alessandrini EA, Alpern ER, Chamberlain JM, Shea JA, Gorelick MH (2010) A new diagnosis grouping system for child emergency department visits. Acad Emerg Med 17(2):204–213. https://doi.org/10.1111/j.1553-2712.2009.00635.x
Gale SC, Shafi S, Dombrovskiy VY, Arumugam D, Crystal JS (2014) The public health burden of emergency general surgery in the United States: a 10-years analysis of the nationwide inpatient sample--2001 to 2010. J Trauma Acute Care Surg 77(2):202–208. https://doi.org/10.1097/TA.0000000000000362
Unger B, Afilalo M, Boivin JF, Bullard M, Grafstein E, Schull M, Lang E, Colacone A, Soucy N, Xue X, Segal E (2010) Development of the Canadian emergency department diagnosis shortlist. CJEM 12(04):311–319. https://doi.org/10.1017/S1481803500012392
Green SM, Roback MG, Miner JR, Burton JH, Krauss B (2007) Fasting and emergency department procedural sedation and analgesia: a consensus-based clinical practice advisory. Ann Emerg Med 49(4):454–461. https://doi.org/10.1016/j.annemergmed.2006.08.017
Herwartz H, Strumann C (2012) On the effect of prospective payment on local hospital competition in Germany. Health Care Manag Sci 15(1):48–62. https://doi.org/10.1007/s10729-011-9180-9
Huang XM (1995) A planning model for requirement of emergency beds. IMA J Math Appl Med Biol 12(3-4):345–353. https://doi.org/10.1093/imammb/12.3-4.345
Hughes D, McGuire A (2003) Stochastic demand, production responses and hospital costs. J Health Econ 22(6):999–1010. https://doi.org/10.1016/S0167-6296(03)00048-1
Hof S, Fügener A, Schoenfelder J, Brunner JO (2015) Case mix planning in hospitals: a review and future agenda. Health Care Manag Sci 20(2):1–14. https://doi.org/10.1007/s10729-015-9342-2
Clemens J, Gottlieb JD (2014) Do physicians' financial incentives affect medical treatment and patient health? Am Econ Rev 104(4):1320–1349. https://doi.org/10.1257/aer.104.4.1320
Dolton P, Pathania V (2016) Can increased primary care access reduce demand for emergency care? Evidence from England's 7-days GP opening. J Health Econ 49:193–208. https://doi.org/10.1016/j.jhealeco.2016.05.002
Obermeyer Z, Emanuel EJ (2016) Predicting the future - big data, machine learning, and clinical medicine. N Engl J Med 375(13):1216–1219. https://doi.org/10.1056/NEJMp1606181
Breiman L (2001) Random forests. Mach Learn 45(1):5–32. https://doi.org/10.1023/A:1010933404324
Dietterich TG (2000) An experimental comparison of three methods for constructing ensembles of decision trees: bagging, boosting, and randomization. Mach Learn 40(2):139–157. https://doi.org/10.1023/A:1007607513941
Liaw A, Wiener M (2002) Classification and regression by random forest. R News 2:18–22
Malley JD, Kruppa J, Dasgupta A, Malley KG, Ziegler A (2012) Probability machines: consistent probability estimation using nonparametric learning machines. Methods Inf Med 51(1):74–81. https://doi.org/10.3414/ME00-01-0052
Strobl C, Malley J, Tutz G (2009) An introduction to recursive partitioning: rationale, application, and characteristics of classification and regression trees, bagging, and random forests. Psychol Methods 14(4):323–348. https://doi.org/10.1037/a0016973
Fernandez-Delgado M, Cernadas E, Barro S, Amorim D (2014) Do we need hundreds of classifiers to solve real world classification problems? J Mach Learn Res 15:3133–3181
Díaz-Uriarte R, Alvarez de Andrés SA (2006) Gene selection and classification of microarray data using random forest. BMC Bioinformatics 7(1):3. https://doi.org/10.1186/1471-2105-7-3
Billings J, Parikh N, Mijanovich T (2000) Emergency department use in New York City: a survey of Bronx patients. Issue Brief 435:1–5
Smulowitz PB, Lipton R, Wharam JF, Adelman L, Weiner SG, Burke L, Baugh CW, Schuur JD, Liu SW, McGrath ME, Liu B, Sayah A, Burke MC, Pope JH, Landon BE (2011) Emergency department utilization after the implementation of Massachusetts health reform. Ann Emerg Med 58(3):225–234. https://doi.org/10.1016/j.annemergmed.2011.02.020
Taubman SL, Allen HL, Wright BJ, Baicker K, Finkelstein AN (2014) Medicaid increases emergency-department use: evidence from Oregon's health insurance experiment. Science 343(6168):263–268. https://doi.org/10.1126/science.1246183
Wharam JF, Landon BE, Galbraith AA, Kleinman KP, Soumerai SB, Ross-Degnan D (2007) Emergency department use and subsequent hospitalizations among members of a high-deductible health plan. JAMA 297(10):1093–1102. https://doi.org/10.1001/jama.297.10.1093
Alessandrini EA, Alpern ER, Chamberlain JM, Shea JA, Holubkov R, Gorelick MH, Pediatric Emergency Care Applied Research Network (2012) Developing a diagnosis-based severity classification system for use in emergency medical services for children. Acad Emerg Med 19(1):70–78. https://doi.org/10.1111/j.1553-2712.2011.01250.x
Australian Institute of Health and Welfare (2012) Australian hospital statistics, 2010–11s. Australian Institute of Health and Welfare, Canberra
Troyanskaya O, Cantor M, Sherlock G, Brown P, Hastie T, Tibshirani R, Botstein D, Altman RB (2001) Missing value estimation methods for DNA microarrays. Bioinformatics 17(6):520–525. https://doi.org/10.1093/bioinformatics/17.6.520
Hanley JA, McNeil BJ (1982) The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology 143(1):29–36. https://doi.org/10.1148/radiology.143.1.7063747
Clopper CJ, Pearson ES (1934) The use of confidence or fiducial limits illustrated in the case of the binomial. Biometrika 26(4):404–413. https://doi.org/10.1093/biomet/26.4.404
Bäuml M, Dette T (2014) Hospital responses to price changes: evidence from the German DRG system. Mimeo
Riessen R, Gries A, Seekamp A, Dodt C, Kumle B, Busch H-J (2015) Positionspapier für eine reform der medizinischen Notfallversorgung in Deutschen Notaufnahmen. Notfall Rettungsmed 18(3):174–185. https://doi.org/10.1007/s10049-015-0013-0
Wilson M, Cutler D (2014) Emergency department profits are likely to continue as the affordable care act expands coverage. Health Aff 33(5):792–799. https://doi.org/10.1377/hlthaff.2013.0754
Pitts SR, Pines JM, Handrigan MT, Kellermann AL (2012) National trends in emergency department occupancy, 2001 to 2008: effect of inpatient admissions versus emergency department practice intensity. Ann Emerg Med 60(6):679–686.e3. https://doi.org/10.1016/j.annemergmed.2012.05.014
OECD (2017) Hospital beds (indicator). https://doi.org/10.1787/0191328e-en
Corbella X, Ortiga B, Juan A, Ortega N, Gomez-Vaquero C, Capdevila C, Bardes I, Alonso G, Alonso G, Ferre C, Soler M, Mañez R, Jaurrieta E, Pujol R, Salazar A (2012) Alternatives to conventional hospitalization for improving lack of access to inpatient beds. A 12-years cross-sectional analysis. JHA 2(2):9–21. https://doi.org/10.5430/jha.v2n2p9
Athey S (2017) Beyond prediction: Using big data for policy problems. Science (New York, NY) 355(6324):483–485. https://doi.org/10.1126/science.aal4321
Kleinberg J, Ludwig J, Mullainathan S, Obermeyer Z (2015) Prediction policy problems. Am Econ Rev 105(5):491–495. https://doi.org/10.1257/aer.p20151023
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Krämer, J., Schreyögg, J. & Busse, R. Classification of hospital admissions into emergency and elective care: a machine learning approach. Health Care Manag Sci 22, 85–105 (2019). https://doi.org/10.1007/s10729-017-9423-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10729-017-9423-5