Abstract
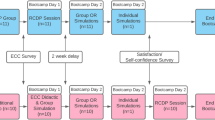
Simulation-based teaching (SBT) is increasingly used in medical education. As an alternative to other teaching methods there is a lack of evidence concerning its efficacy. The aim of this study was to evaluate the potency of SBT in anesthesia in comparison to problem-based discussion (PBD) with students in a randomized controlled setting. Thirty-three fourth-year medical students attending a curricular anesthesiology course were randomly allocated to either a session of SBT or a session of PBD on an emergency induction method. Ten days later all students underwent examination in a simulator. The performance of each student was evaluated by weighted tasks, established according to a modified Delphi process. Confidence and a multiple-choice questionnaire were additionally performed pre- and post-intervention. A total of 32 students completed the study. Participants in the SBT group presented with significantly higher self-assessment scores after the intervention than students in the PBD group. However, students in the SBT group achieved only slightly and statistically insignificantly higher scores in the theoretical and simulator examination (p > 0.05) with only a moderate effect size of d = 0.52. The current study demonstrates that both PBD and SBT lead to comparable short-term outcomes in theoretical knowledge and clinical skills. However, undesirably, SBT students overrated their anticipated clinical abilities and knowledge improvement.



Similar content being viewed by others
References
Bloom, B. S. (1984). The 2 sigma problem: The search for methods of group instruction as effective as one-to-one tutoring. Education Research, 4, 4–16.
Byrick, R., Cleave-Hogg, D., & McKnight, D. (1998). A crisis management program for residents in anesthesia. Academic Medicine: Journal of the Association of American Medical Colleges, 73(5), 592.
Chopra, V., Gesink, B. J., & DeJong, J. (1994). Does training on an anaesthesia simulator lead to improvement in performance? British Journal of Anaesthesia, 73(3), 293–297.
Cohen, J. (1988). Statistical power analysis for the behavioral sciences. Hillsdale, NJ: Lawrence Erlbaum.
Colliver, J. A. (2000). Effectiveness of problem-based learning curricula: Research and theory. Academic Medicine: Journal of the Association of American Medical Colleges, 75(3), 259–266.
Cooper, J. B., & Taqueti, V. R. (2004). A brief history of the development of mannequin simulators for clinical education and training. Quality & Safety in Health Care, 13(Suppl 1), i11–i18.
Cumin, D., & Merry, A. F. (2007). Simulators for use in anaesthesia. Anaesthesia, 62(2), 151–162.
DeVita, M. A., Schaefer, J., Lutz, J., Dongilli, T., & Wang, H. (2004). Improving medical crisis team performance. Critical Care Medicine, 32(Suppl 2), S61–S65.
Eva, K. W., Cunnington, J. P., Reiter, H. I., Keane, D. R., & Norman, G. R. (2004). How can I know what I don’t know? Poor self assessment in a well-defined domain. Advances in Health Sciences Education: Theory and Practice, 9(3), 211–224.
Eva, K. W., & Regehr, G. (2005). Self-assessment in the health professions: A reformulation and research agenda. Academic Medicine: Journal of the Association of American Medical Colleges, 80(Suppl 10), S46–S54.
Eva, K. W., & Regehr, G. (2007). Knowing when to look it up: A new conception of self-assessment ability. Academic Medicine: Journal of the Association of American Medical Colleges, 82(Suppl 10), S81–S84.
Flanagan, B., Nestel, D., & Joseph, M. (2004). Making patient safety the focus: Crisis resource management in the undergraduate curriculum. Medical Education, 38(1), 56–66.
Gaba, D. M., & DeAnda, A. (1988). A comprehensive anesthesia simulation environment: Re-creating the operating room for research and training. Anesthesiology, 69(3), 387–394.
Gardiner, J. (2006). Simulators in obstetric anaesthesia are a waste of time. International Journal of Obstetric Anesthesia, 15(1), 44–46.
Goldmann, K., & Ferson, D. Z. (2005). Education and training in airway management. Best Practice & Research. Clinical Anaesthesiology, 19(4), 717–732.
Hebert, R., & Bravo, G. (1996). Development and validation of an evaluation instrument for medical students in tutorials. Academic Medicine: Journal of the Association of American Medical Colleges, 71(5), 488–494.
Issenberg, S. B., McGaghie, W. C., Petrusa, E. R., Lee Gordon, D., & Scalese, R. J. (2005). Features and uses of high-fidelity medical simulations that lead to effective learning: A BEME systematic review. Medical Teacher, 27(1), 10–28.
Jude, D. C., Gilbert, G. G., & Magrane, D. (2006). Simulation training in the obstetrics and gynecology clerkship. American Journal of Obstetrics Gynecology, 195(5), 1489–1492.
Knudson, M. M., & Sisley, A. C. (2000). Training residents using simulation technology: Experience with ultrasound for trauma. The Journal of Trauma, 48(4), 659–665.
Lighthall, G. K. (2006). The value of simulation training during anesthesia residency. Anesthesiology, 105(2), 433.
Lippert, A., Nielsen, M. S., & Ostergaard, D. (2004). Medical simulation in anesthesiology. The Danish Society of Anesthesiology and Intensive Medicine. Ugeskr Laeger, 166(12), 1102.
Marshall, R. L., Smith, J. S., Gorman, P. J., Krummel, T. M., Haluck, R. S., & Cooney, R. N. (2001). Use of a human patient simulator in the development of resident trauma management skills. The Journal of Trauma, 51(1), 17–21.
Matsumoto, E. D., Hamstra, S. J., Radomski, S. B., & Cusimano, M. D. (2002). The effect of bench model fidelity on endourological skills: A randomized controlled study. The Journal of Urology, 167(3), 1243–1247.
McFetrich, J. (2006). A structured literature review on the use of high fidelity patient simulators for teaching in emergency medicine. Emergency Medicine Journal, 23(7), 509–511.
Morgan, P. J., & Cleave-Hogg, D. (2002a). Comparison between medical students’ experience, confidence and competence. Medical Education, 36(6), 534–539.
Morgan, P. J., & Cleave-Hogg, D. (2002b). A worldwide survey of the use of simulation in anesthesia. Canadian Journal of Anaesthesia, 49(7), 659–662.
Morgan, P. J., & Cleave-Hogg, D. M. (2001). Cost and resource implications of undergraduate simulator-based education. Canadian Journal of Anaesthesia, 48(8), 827–828.
Morgan, P. J., Cleave-Hogg, D., McIlroy, J., & Devitt, J. H. (2002). Simulation technology: A comparison of experiential and visual learning for undergraduate medical students. Anesthesiology, 96(1), 10–16.
Murray, D. (2005). Clinical simulation: Measuring the efficacy of training. Current Opinion in Anaesthesiology, 18(6), 645–648.
Ostergaard, D. (2004). National medical simulation training program in Denmark. Critical Care Medicine, 32(Suppl 2), S58–S60.
Scavone, B. M., Sproviero, M. T., McCarthy, R. J., Wong, C. A., Sullivan, J. T., Siddall, V. J., & Wade, L. D. (2006). Development of an objective scoring system for measurement of resident performance on the human patient simulator. Anesthesiology, 105(2), 260–266.
Steadman, R. H., Coates, W. C., Huang, Y. M., Matevosian, R., Larmon, B. R., McCullough, L., & Ariel, D. (2006). Simulation-based training is superior to problem-based learning for the acquisition of critical assessment and management skills. Critical Care Medicine, 34(1), 151–157.
Weller, J. M. (2004). Simulation in undergraduate medical education: Bridging the gap between theory and practice. Medical Education, 38(1), 32–38.
Weller, J., Wilson, L., & Robinson, B. (2003). Survey of change in practice following simulation-based training in crisis management. Anaesthesia, 58(5), 471–473.
Yee, B., Naik, V. N., Joo, H. S., Savoldelli, G. L., Chung, D. Y., Houston, P. L., Karatzoglou, B. J., & Hamstra, S. J. (2005). Nontechnical skills in anesthesia crisis management with repeated exposure to simulation-based education. Anesthesiology, 103(2), 241–248.
Acknowledgements
We thank Dr. Trevor G. Cooper, Ph.D., for carefully revising the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wenk, M., Waurick, R., Schotes, D. et al. Simulation-based medical education is no better than problem-based discussions and induces misjudgment in self-assessment. Adv in Health Sci Educ 14, 159–171 (2009). https://doi.org/10.1007/s10459-008-9098-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10459-008-9098-2