Summary
Paget’s disease of bone (osteitis deformans) is a benign focal disorder of accelerated skeletal remodeling. Either a single bone (monostotic) or multiple bones (polyostotic) can be affected. In patients with suspected Paget’s disease plain radiographs of the suspicious regions of the skeleton are recommended. The initial biochemical evaluation of a patient should be done using serum total ALP (alkaline phosphatase) or with the use of a more specific marker of bone formation: PINP (intact N-terminal type 1 procollagen propeptide) or CTX (cross-linked C‑telopeptide). Treatment with a bisphosphonate is recommended for most patients with active Paget’s disease who are at risk for further skeletal and extraskeletal complications. A single dose of 5 mg i.v. zoledronate as the treatment of choice in patients without contraindications is suggested. Oral bisphosphonates are less potent when compared to zoledronate. Treatment with an antiresorptive agent induces a more rapid decrease in resorption markers compared to formation marker. Measurement of total ALP or other baseline disease activity markers (e. g. CTX) at 6 to 12 weeks, when bone turnover will have shown a substantial decline, is an acceptable and cost-effective option. Maximum suppression of high bone turnover may require measurement at 6 months after administration. In patients with increased bone turnover, biochemical follow-up is recommended to be used as a more objective indicator of relapse rather than symptoms. The prolonged response after zoledronate treatment should be assessed every 1–2 years after normal bone turnover. With less potent drugs, every 6 to 12 months is appropriate.
Zusammenfassung
Morbus Paget (Osteitis deformans) ist eine fokale benigne Erkrankung des Knochens mit beschleunigtem Knochenumsatz. Betroffen sind entweder einzelne (monostotische Form) oder mehrere Knochen (polyostotische Form). Diagnostisch werden Röntgenaufnahmen der suszipierten Skelettregionen empfohlen. Zur weiteren serologischen Untersuchung wird die alkalische Phosphatase (AP) empfohlen. Zusätzlich können spezifische Serummarker der Knochenformation (PINP Prokollagen Typ 1 N-terminales Propeptid) oder der Knochenresorption (CTX Cross-linked C‑Telopeptid) bestimmt werden. Zur Behandlung von Patienten mit einem aktiven M. Paget und einem erhöhten Risiko für weitere skeletale oder extraskeletale Manifestationen werden Bisphosphonate empfohlen. Eine einmalige i.v.-Dosis von 5 mg Zoledronat ist Mittel der Wahl bei Patienten ohne Kontraindikationen. Orale Bisphosphonate sind im Vergleich zu i.v.-Applikationen weniger potent. Die Behandlung mit einem antiresorptiven Medikament induziert eine schnellere Reduktion der Resorptionsmarker im Vergleich zu den Formationsmarkern. Die Bestimmung der AP oder anderer Marker (z. B. CTX) 6 bis 12 Wochen nach der Applikation eines Bisphosphonats ist eine kostengünstige Methode zur Überprüfung des therapeutischen Erfolgs. Die maximale Suppression wird erst nach 6 Monaten erreicht. Bei Patienten mit erhöhtem Knochenumsatz ist die Bestimmung der biochemischen Marker ein objektiverer Indikator im Vergleich zur Symptomkontrolle. Das Ansprechen auf eine Therapie mit Zoledronat sollte 1 bis 2 Jahre nach Applikation serologisch kontrolliert werden; mit weniger potenten antiresorptiven Medikamenten alle 6 bis 12 Monate.
Similar content being viewed by others
Introduction
Paget’s disease of bone (osteitis deformans) is a benign focal disorder of accelerated skeletal remodeling with an approximate prevalence of 1.1 % in pelvic bones in patients above the age of 40 [1, 2]. Either a single bone (monostotic) or multiple bones (polyostotic) can be affected which leads to bone hypertrophy, cortical expansion, and abnormal bone architecture. Clinical symptoms include bone pain, bone deformity, and skeletal fragility. Complications of Paget’s disease involve bones (deformity, fracture, and neoplastic degeneration), joints (osteoarthritis), the nervous and the vascular system [3].
Method of development of evidence-based guidelines for clinical practice
This review article follows the approach recommendations by the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) group, an international group with expertise in the implementation of evidence-based guidelines.
In terms of the strength of the recommendation and the quality of evidence, strong recommendations use the phrase “recommended” and the number “1”, and weak recommendations use the phrase “suggest/suggested” and the number “2”.
Crosses indicate the quality of evidence, such that “+” denotes very low quality of evidence, “++” low quality, “+++” moderate quality, and “++++” high quality [4–6].
Clinical signs, symptoms, and complications
Many patients with Paget’s disease of bone are asymptomatic; therefore, the disease is discovered when a radiograph and/or a bone scan is performed for another clinical indication. Elevated levels of serum total alkaline phosphatase (ALP) on a multiphasic screening chemistry panel are often the first indicator. An accurate clinical examination and the medical history are two necessary steps of a diagnostic algorithm involving the musculoskeletal system and checking for endocrinological and metabolic disorders, neurological and cardiovascular complications. A detailed summary of symptoms and complications discovered in diverse clinical examinations are listed in Table 1 [7].
Diagnosis—imaging
In patients with suspected Paget’s disease, plain radiographs of the suspicious regions of the skeleton are recommended – 1/++++.
The evolution of the radiological changes with Paget’s disease mirrors the pathological changes that evolve over time and are adequately demonstrated by X‑ray evaluation. The earliest lesions are osteolytic and are best observed in the skull and long bones with a general progression of 8 mm/year until the increased osteoblastic activity transforms the previous osteolytic lesion into bone tissue with a mixed osteolytic–sclerotic appearance. In the final phase, sclerosis is the dominant feature, although secondary fronts of osteolytic lesions may be noted. After decades of untreated disease, affected bones may increase in size, and lateral and anterior bowing may be seen predominately in lower extremity long bones. Occasionally, complete transverse fractures may develop at these anatomical sites. In general—and according to the radiologist’s experience—lesions caused by Paget’s disease can be distinguished by radiological examinations. Very seldom it is necessary to perform a bone biopsy to make a definite diagnosis [8, 9].
Other radiological examinations, such as computed tomography (CT scan), magnetic resonance imaging (MRI), and positron emission tomography (PET) are useful in patients, particularly if a neoplasm at a pagetic site is suspected. All the above mentioned methods are not used routinely in the evaluation of patients with Paget’s disease [10].
In patients with diagnosed Paget’s disease, a radionuclide bone scan to determine the extent of the disease and identify possible asymptomatic sites is suggested – 2/+++.
Due to the majority of asymptomatic lesions, radionuclide imaging of the skeleton rather than general X‑ray survey has become the standard means to diagnose and document the extent of skeletal involvement of Paget’s disease. This is the most sensitive examination for the detection of localized increased bone cell activity, and lesions may be detected before they are clearly apparent on x‑ray images. It is not recommended to repeat radionuclide imaging, but if a treatment is administered, the radionuclide uptake of the lesion is usually reduced [11, 12].
Diagnosis—biochemistry
After the radiological diagnosis of Paget’s disease, the initial biochemical evaluation of a patient should be done using serum total ALP or with the use of a more specific marker of bone formation (when appropriate) – 1/++++.
In patients who have the radiological evidence of Paget’s disease, the least expensive biochemical test to determine the metabolic activity of the disorder is the measurement of total serum ALP. Although the increase of this bone formation marker is secondary to the change in bone resorption, it correlates well with the extent of skeletal involvement assessed by either radiographs or scintigraphy. Furthermore, ALP values reflect the efficacy of pharmacological intervention by, e. g., a potent bisphosphonate [13].
The recommendation to use total ALP to screen for the metabolic activity of Paget’s disease is based on the low cost and universal availability of this test in primary and secondary care. These economic advantages should be weighed against the greater specificity but somewhat higher cost, possibly restricted availability and reimbursement by health care providers of more bone specific formation markers.
Measuring a specific marker of bone formation or resorption is recommended in patients with Paget’s disease and abnormal liver or biliary tract function to assess response to treatment or follow evolution of the disease in untreated patients – 1/+++.
In general, available serum biomarkers show a good correlation with the disease activity assessed by scintigraphy [14].
Serum PINP (intact N-terminal type 1 procollagen propeptide) reflecting bone formation/osteoblast activity is considered the best option. If cost, reimbursement or availability prevents the use of this marker, resorption marker such as serum CTX (cross-linked C‑telopeptide) or urinary NTX provide accurate estimates of baseline bone metabolic activity and the response to treatment in patients with Paget’s disease.
The disadvantage of total ALP is its overlap with ALP from the liver. If liver tests are abnormal (e. g., elevated liver enzymes), measurement of PINP provides an accurate, but more expensive alternative, to test bone formation activity. Other markers of bone formation such as BSAP (bone-specific alkaline phosphatase) or osteocalcin are less useful than PINP. There may be an up to 20 % cross-reactivity of antibodies to liver ALP with bone ALP, and osteocalcin has been shown to be an insensitive marker of disease activity in Paget’s disease [15, 16].
In untreated Paget’s disease, αCTX (contains aspartyl-glycine) is raised proportionally more than βCTX (formed from spontaneous isoaspartyl formation as bone ages in response to treatment), but commercial assays on αCTX are not available. Therefore, βCTX may slightly underestimate to response to treatment of a very active disease due to a isomerization phenomenon. Urinary NTX also shows large reductions during treatment, but the variability of individual responses may result in less discrimination when directly compared to bone formation markers.
The advantage of telopeptide assays over bone formation assays is represented by a much faster demonstration of a maximal decrease in bone resorption than in bone formation after treatment. Specific markers of bone turnover are also useful in patients with limited radiographic or scintigraphic evidence of Paget’s disease in conjunction with normal ALP levels [17].
Treatment of Paget’s disease
Treatment with a bisphosphonate is recommended for most patients with active Paget’s disease who are at risk for further skeletal and extraskeletal complications – 1/+++.
The clinical potency of a bisphosphonate is determined by its affinity for hydroxyapatite (which determines skeletal uptake) and the potency of its inhibition of farnesyl pyrophosphate synthase (FPP). During bone resorption bisphosphonates are incorporated by osteoclasts, where they inhibit FPP, a critical step in the mevalonate pathway that leads to the synthesis of cholesterol as well as to the production of geranylgeraniol, which is critical to the prenylation of intracellular proteins. Disruption of this pathway adversely affects the osteoclast cytoskeleton and results in secondary apoptosis [18, 19].
There is consensus that pharmacological treatment should be offered to patients with active disease who are either symptomatic or at substantial risk of future complications. In addition, treatment of patients with active disease before surgery involving pagetic bone has been advised in the belief that the resultant reductions in bone vascularity decrease perioperative blood loss [20].
The increasing superiority of disease control observed with longer term follow-up of zoledronate-treated patients indicates that a re-evaluation of the indications for treatment is appropriate. Treatment regimens based on potent oral bisphosphonates or less potent intravenous (i.v.) such as pamidronate have typically produced biochemical remissions lasting 1–3 years. Therefore, the regular follow-up interval of patients who had received treatment is 6 months. Even in patients not receiving therapy but who had an active disease, regular monitoring of comparable frequency is required.
The pharmacological management of Paget’s disease is primarily based on the use of drugs that reduce bone turnover, particularly bone resorption by osteoclasts. Therefore a single dose of 5 mg i.v. zoledronate as the treatment of choice in patients without contraindications is suggested – 2/+++.
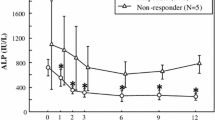
A single, 5 mg i.v. dose of zoledronate has been compared with risedronate 30 mg/day for 2 months in two clinical trials. The core study was of 6‑month duration, with 96 % of patients randomized to zoledronate showing a therapeutic response compared with 74 % of those randomized to risedronate (p < 0.001). ALP levels normalized in 89 % of patients in the zoledronate group and 58 % of those given risedronate (p < 0.001). Zoledronate showed a more rapid onset of action, and superior effects on quality of life, including bone pain relief. Patients with a therapeutic response in the core study entered a follow-up study that compared the duration of remissions with these two treatments. At 2 years after drug administration, therapeutic response was maintained in 98 % of those receiving zoledronate and 57 % of risedronate patients. At 5 to 6 years follow-up, these figures were 87 % and 38 %, respectively [18, 21, 22].
Although the mean PINP values remained within the normal range in the zoledronate group throughout the follow-up, gradual increases in the risedronate group were observed. Patients who had a PINP of <40 µg/l or a total ALP of <80 IU/l 6 months after treatment with zoledronate were found to have a likelihood >90 % of no relapse during follow-up [22].
Zoledronate has a satisfactory safety profile; the most common adverse event being flu-like symptoms, which occur in about 2.5 % of patients. The frequency and severity of these reactions is reduced by about one-half with nonsteroidal anti-inflammatory drugs, which can be used prophylactically. Very seldom (<1 %) uveitis and other inflammatory changes in the eye can be observed as part of the acute phase. Zoledronate is potentially nephrotoxic; an administration in patients with a glomerular filtration rate <35 ml/min is not recommended. Lower doses or longer infusion times in these patients can be considered, but are not approved by regulatory agencies. In the presence of severe vitamin D deficiency (25-OH vitamin D < 10 ng/ml or <25 nmol/l) symptomatic hypocalcemia can occur due to the administration of a potent bisphosphonate [23].
Risedronate tablets (30 mg/day for 2–3 months) were evaluated in open studies and in randomized controlled trials with etidronate. While there was a 73 % normalization of ALP levels and evidence of relief of pagetic pain, the comparatively high doses of oral bisphosphonates caused significant upper gastrointestinal side effects [24–26].
Ibandronate has been shown to provide effective short-term control of Paget’s disease, but it has not been actively promoted for this indication [27].
Alendronate was studied in two randomized trials, one comparing this bisphosphonate to placebo, and the other comparing it with etidronate. With a dosage of 40 mg/day alendronate for 6 months ALP normalized in 60–70 % of patients with healing of lytic radiological lesions. Bone biopsies confirmed the restoration of normal lamellar bone histology [28, 29].
Pamidronate was shown to normalize bone resorption with one week of oral dosing, although normalization of bone formation lasted 3–6 months. Similarly, i.v. pamidronate is reported to be efficacious in the treatment of Paget’s disease, but to a lesser extent when compared to zoledronate in terms of reduction of biochemical markers [30].
Less data are available about denosumab, the RANKL antibody that blocks the maturation and activation of osteoclasts. Case reports demonstrated normalization of ALP levels 4–8 months after (recurrent) administration, symptomatic and scintigraphic improvement after the subcutaneous application of 60 mg. Due to the pharmacological duration of denosumab repeated injections are needed to maintain normal serum values of bone turnover marker and clinical signs of remission [31–33].
A summary of dosing and application intervals of diverse drugs for the treatment of Paget’s disease is given in Table 2.
Although the specific therapy of Paget’s disease is the administration of bisphosphonates, disease complications may also require surgical interventions, such as joint replacement, osteotomy for deformity, or surgical management of fractures. The indications for surgical interventions in pagetic patients are similar to nonpagetic patients. Paraplegia associated with Paget’s disease appears to be better when managed with bisphosphonates rather than with surgery [18, 34, 35].
Monitoring treatment
Treatment with antiresorptive agents induces a more rapid decrease in resorption markers compared to formation marker. For most patients, measurement of total ALP or other baseline disease activity markers (e. g., CTX) at 6 to 12 weeks, when bone turnover will have shown a substantial decline, is an acceptable and cost-effective option. Maximum suppression of high bone turnover may require measurement at 6 months [6].
Patients who have osteolytic lesions caused by Paget’s disease have a repeated x‑ray examination approximately 1 year after radiological diagnosis to determine whether there has been an improvement with therapy or worsening in the absence of therapy. Subsequent x‑rays are suggested in the event of persistent elevations of biochemical markers of bone turnover or the presence of bone pain and to determine when there is a resolution of the lesion – 2/++.
To maximize the duration of remission, bone turnover marker should be reduced below the midpoint of the reference range for the chosen monitoring bone turnover marker – 2/++.
The normal level of prepagetic bone turnover is unknown for most patients, the usual aim is to reduce turnover values into the lower half of the reference range because this increases the probability that individual patient normal values will have been achieved.
After treatment with zoledronate, achieving ALP levels in the lower half of the normal range was associated with a 6-year risk of losing therapeutic response <10 % [7, 22].
Because the duration of biochemical remission is strongly determined by the nadir value achieved by treatment, long-term complications such as fracture, deformity, and degenerative joint disease might be prevented or reduced by long-term normalization of bone turnover [6, 36].
Measurement of PINP or AP/BSAP (bone-specific AP) and CTX or NTX is suggested for the assessment of the activity of untreated monostotic Paget’s disease, although these values may be normal when evidence of disease activity is still clearly demonstrated – 2/++.
Relapse and retreatment
In patients with increased bone turnover, biochemical follow-up is recommended to be used as a more objective indicator of relapse rather than symptoms – 1/+++.
The frequency of biochemical monitoring depends on the applied therapeutic agent. The prolonged response after zoledronate treatment should be assessed every 1–2 years after normal bone turnover. With less potent drugs, every 6 to 12 months is appropriate [15, 22, 36].
Recurrence of bone pain in the absence of an increase in bone turnover is uncommon. Because it may be due to other causes such as degenerative joint disease, it is therefore an insensitive indicator of relapse [6].
Management of complications
Hearing loss
Hearing loss can be associated with Paget’s disease; treatment with bisphosphonates is suggested – 2/++.
To date no randomized, placebo-controlled clinical trial focused on the effect of antipagetic therapy on hearing loss in patients with Paget’s disease of the temporal bone. Generally, patients who have been treated do not appear to have further rapid deterioration of hearing, but for the most part the hearing loss is not reversible. Less and no frequent data exist on the efficacy of cochlear implants in this patient population [37].
Osteoarthritis
The use of analgesics as adjunctive therapy for mild-to-moderate joint pain due to joint cartilage deterioration in patients with Paget’s disease adjacent to the painful joint is suggested – 2/++.
For patients with severe osteoarthritis adjacent to Paget’s disease of bone bisphosphonate therapy before undergoing elective total joint replacement is suggested to prevent intraoperative hemorrhaging and postoperative loosening of the prosthesis – 2/++.
Osteoarthritis is a relatively common complication in weight-bearing joints such as the hip or knee, when adjacent bones are affected by Paget’s disease. Due to increased blood flow to areas of active disease, preoperative therapy should reduce blood flow and lessen the possibility of hemorrhage. Reduction of osteoclast activity should also reduce the chance of loosening of the prosthesis and prevent a more rapid progression of the disease. Heterotropic bone formation is a rare complication after surgery that may require specific intervention. If surgery is required in the near future, an i.v. bisphosphonate should be administered 1 to 2 months before an operation. An oral bisphosphonate could be considered if surgery can be delayed for 3 to 4 months. High doses of etidronate should never be used in such cases since it may cause an increase of fracture risk and impaired healing due to disturbances of bone mineralization [38, 39].
Bowing of lower extremity
Treatment with a potent bisphosphonate before elective surgery is suggested for patients who require an osteotomy to correct severe bowing of the lower extremity associated with impaired ambulation and/or severe joint pain – 2/++.
Although there are no controlled clinical trials, it is likely that reducing the blood flow to a tibia/femur that requires straightening will improve surgical outcome. This will consecutively decrease the possibility of nonunion and prevent acceleration of the pagetic activity in untreated patients [40].
Paralysis
In case of paraplegia associated with Paget’s disease of the spine, immediate treatment with a potent i.v. bisphosphonate associated with neurosurgical consultation is suggested – 2/++.
Most patients with spinal paralysis recover well after medical treatment only, presumably due to the correction of ischemia caused by vascular steal. In case of severe structural damage, surgery will also be necessary [41].
Neoplasms
Patients with osteosarcoma or a giant cell tumor should be evaluated by an orthopedic surgeon. If surgery is planned, pretreatment with a potent bisphosphonate is suggested to reduce bleeding from the adjacent pagetic bone – 2/++.
Osteosarcoma is a rare complication that may arise in pagetic bone because of the proliferation of osteoblasts.
Giant cell tumors, usually benign, are described in a small number of patients with Paget’s disease of bone. Despite good response to radiation therapy, they are usually treated surgically. Denosumab is capable to shrink giant cell tumors in patients without Paget’s disease. Patients who have unresectable tumors or in whom surgical procedures are likely to result in severe morbidity can be treated with 120 mg of denosumab subcutaneously every four weeks [42].
References
Ringe JD, Jend HH, Becker H. Epidemiologie der Osteitis deformans Paget. Munch Med Wschr. 1984;126:683–6.
Mikosch P, Trifina E, Roschger P, Haller J, Klaushofer K. Klinik und Diagnose des Morbus Paget. J Mineralstoffwechsel Muskuloskelet Erkrank. 2012;19:68–73.
Lyles KW, Siris ES, Singer FR, Meunier PJ. A clinical approach to diagnosis and management of Paget’s disease of bone. J Bone Miner Res. 2001;16:1379–87.
Atkins D, Best D, Briss PA, Eccles M, Falck-Ytter Y, Flottorp S, et al. Grading quality of evidence and strength of recommendations. BMJ. 2004;328:1490.
Swiglo BA, Murad MH, Schünemann HJ, Kunz R, Vigersky RA, Guyatt GH, et al. A case for clarity, consistency, and helpfulness: state-of-the-art clinical practice guidelines in endocrinology using the grading of recommendations, assessment, development, and evaluation system. J Clin Endocrinol Metab. 2008;93:666–73.
Singer FR, Bone HG, Hosking DJ, Lyles KW, Murad MH, Reid IR, et al. Paget‘s disease of bone: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2014;99:4408–22.
Ralston SH, Langston AL, Reid IR. Pathogenesis and management of Paget’s disease of bone. Lancet. 2008;372:155–63.
Smith SE, Murphey MD, Motamedi K, Mulligan ME, Resnik CS, Gannon FH. From the archives of the AFIP. Radiologic spectrum of Paget disease of bone and its complications with pathologic correlation. Radiographics. 2002;22:1191–216.
Maldague B, Malghem J. Dynamic radiologic patterns of Paget’s disease of bone. Clin Orthop Relat Res. 1987;(217):126–51. doi:10.1097/00003086-198704000-00012.
López C, Thomas DV, Davies AM. Neoplastic transformation and tumour-like lesions in Paget’s disease of bone: a pictorial review. Eur Radiol. 2003;13(Suppl 4):L151–63.
Shirazi PH, Ryan WG, Fordham EW. Bone scanning in evaluation of Paget’s disease of bone. CRC Crit Rev Clin Radiol Nucl Med. 1974;5:523–58.
Fogelman I, Carr D. A comparison of bone scanning and radiology in the assessment of patients with symptomatic Paget’s disease. Eur J Nucl Med. 1980;5:417–21.
Eekhoff MEMW, Zwinderman AH, Haverkort DMAD, Cremers SCLM, Hamdy NAT, Papapoulos SE. Determinants of induction and duration of remission of Paget’s disease of bone after bisphosphonate (olpadronate) therapy. Bone. 2003;33:831–8.
Alvarez L, Peris P, Pons F, Guañabens N, Herranz R, Monegal A, et al. Relationship between biochemical markers of bone turnover and bone scintigraphic indices in assessment of Paget’s disease activity. Arthritis Rheum. 1997;40:461–8.
Blumsohn A, Naylor KE, Assiri AM, Eastell R. Different responses of biochemical markers of bone resorption to bisphosphonate therapy in Paget disease. Clin Chem. 1995;41:1592–8.
Withold W, Schulte U, Reinauer H. Method for determination of bone alkaline phosphatase activity: analytical performance and clinical usefulness in patients with metabolic and malignant bone diseases. Clin Chem. 1996;42:210–7.
Alvarez L, Guañabens N, Peris P, Monegal A, Bedini JL, Deulofeu R, et al. Discriminative value of biochemical markers of bone turnover in assessing the activity of Paget’s disease. J Bone Miner Res. 1995;10:458–65.
Reid IR, Miller P, Lyles K, Fraser W, Brown JP, Saidi Y, et al. Comparison of a single infusion of zoledronic acid with risedronate for Paget‘s disease. N Engl J Med. 2005;353:898–908.
Dunford JE, Thompson K, Coxon FP, Luckman SP, Hahn FM, Poulter CD, et al. Structure-activity relationships for inhibition of farnesyl diphosphate synthase in vitro and inhibition of bone resorption in vivo by nitrogen-containing bisphosphonates. J Pharmacol Exp Ther. 2001;296:235–42.
Lyles KW, Colón-Emeric CS, Magaziner JS, Adachi JD, Pieper CF, Mautalen C, et al. Zoledronic acid and clinical fractures and mortality after hip fracture. N Engl J Med. 2007;357:1799–809.
Hosking D, Lyles K, Brown JP, Fraser WD, Miller P, Curiel MD, et al. Long-term control of bone turnover in Paget’s disease with zoledronic acid and risedronate. J Bone Miner Res. 2007;22:142–8.
Reid IR, Lyles K, Su G, Brown JP, Walsh JP, del Pino-Montes J, et al. A single infusion of zoledronic acid produces sustained remissions in Paget disease: data to 6.5 years. J Bone Miner Res. 2011;26:2261–70.
Reid IR, Gamble GD, Mesenbrink P, Lakatos P, Black DM. Characterization of and risk factors for the acute-phase response after zoledronic acid. J Clin Endocrinol Metab. 2010;95:4380–7.
Siris ES, Chines AA, Altman RD, Brown JP, Johnston CC, Lang R, et al. Risedronate in the treatment of Paget’s disease of bone: an open label, multicenter study. J Bone Miner Res. 1998;13:1032–8.
Hosking DJ, Eusebio RA, Chines AA. Paget’s disease of bone: reduction of disease activity with oral risedronate. Bone. 1998;22:51–5.
Singer FR, Clemens TL, Eusebio RA, Bekker Risedronate PJ. A highly effective oral agent in the treatment of patients with severe Paget’s disease. J Clin Endocrinol Metab. 1998;83:1906–10.
Reid IR, Davidson JS, Wattie D, Wu F, Lucas J, Gamble GD, et al. Comparative responses of bone turnover markers to bisphosphonate therapy in Paget’s disease of bone. Bone. 2004;35:224–30.
Dodd GW, Ibbertson HK, Fraser TR, Holdaway IM, Wattie D. Radiological assessment of Paget’s disease of bone after treatment with the bisphosphonates EHDP and APD. Br J Radiol. 1987;60:849–60.
Siris E, Weinstein RS, Altman R, Conte JM, Favus M, Lombardi A, et al. Comparative study of alendronate versus etidronate for the treatment of Paget’s disease of bone. J Clin Endocrinol Metab. 1996;81:961–7.
Frijlink WB, Bijvoet OL, te Velde J, Heynen G. Treatment of Paget’s disease with (3-amino-1-hydroxypropylidene)-1, 1‑bisphosphonate (A.P.D.). Lancet. 1979;1:799–803.
Reid IR, Sharma S, Kalluru R, Eagleton C. Treatment of Paget’s disease of bone with denosumab: case report and literature review. Calcif Tissue Int. 2016; doi:10.1007/s00223-016-0150-6.
Polyzos SA, Singhellakis PN, Naot D, Adamidou F, Malandrinou FC, Anastasilakis AD, et al. Denosumab treatment for juvenile Paget’s disease: results from two adult patients with osteoprotegerin deficiency (“Balkan” mutation in the TNFRSF11B gene). J Clin Endocrinol Metab. 2014;99:703–7.
Grasemann C, Schündeln MM, Hövel M, Schweiger B, Bergmann C, Herrmann R, et al. Effects of RANK-ligand antibody (denosumab) treatment on bone turnover markers in a girl with juvenile Paget’s disease. J Clin Endocrinol Metab. 2013;98:3121–6.
Nancollas GH, Tang R, Phipps RJ, Henneman Z, Gulde S, Wu W, et al. Novel insights into actions of bisphosphonates on bone: differences in interactions with hydroxyapatite. Bone. 2006;38:617–27.
Wallace E, Wong J, Reid IR. Pamidronate treatment of the neurologic sequelae of pagetic spinal stenosis. Arch Intern Med. 1995;155:1813–5.
Patel S, Stone MD, Coupland C, Hosking DJ. Determinants of remission of Paget’s disease of bone. J Bone Miner Res. 1993;8:1467–73.
el Sammaa M, Linthicum FH, House HP, House JW. Calcitonin as treatment for hearing loss in Paget’s disease. Am J Otol. 1986;7:241–3.
Iorio R, Healy WL. Heterotopic ossification after hip and knee arthroplasty: risk factors, prevention, and treatment. J Am Acad Orthop Surg. 2002;10:409–16.
Finerman GA, Gonick HC, Smith RK, Mayfield JM. Diphosphonate treatment of Paget’s disease. Clin Orthop Relat Res. 1976;:115–24. doi:10.1097/00003086-197610000-00018.
Meyers MH, Singer FR. Osteotomy for tibia vara in Paget’s disease under cover of calcitonin. J Bone Joint Surg Am. 1978;60:810–4.
Chen JR, Rhee RS, Wallach S, Avramides A, Flores A. Neurologic disturbances in Paget disease of bone: response to calcitonin. Neurology. 1979;29:448–57.
Chawla S, Henshaw R, Seeger L, Choy E, Blay J‑Y, Ferrari S, et al. Safety and efficacy of denosumab for adults and skeletally mature adolescents with giant cell tumour of bone: interim analysis of an open-label, parallel-group, phase 2 study. Lancet Oncol. 2013;14:901–8.
van Staa TP, Selby P, Leufkens HGM, Lyles K, Sprafka JM, Cooper C. Incidence and natural history of Paget’s disease of bone in England and Wales. J Bone Miner Res. 2002;17:465–71.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
C. Muschitz has received speaker and/or consultancy honoraria from Amgen, Novartis, Servier, Eli Lilly, Nycomed Pharma/Takeda, Kwizda Pharma, Boehringer Ingelheim, Actavis, Alexion, and Daiichi-Sankyo. C. Muschitz has received educational grants/research support from the Austrian Society for Bone and Mineral Research, Roche Austria, Eli Lilly Austria, Eli Lilly International, and Amgen Austria. He has nothing to disclose concerning this manuscript. R. Kocijan has received speaker honoraria from Eli Lilly. He has nothing to disclose concerning this manuscript. X. Feichtinger and J. Haschka declare that they have no competing interests.
Funding source
This review article was not supported by any grant or pharmaceutical company.
Rights and permissions
About this article
Cite this article
Muschitz, C., Feichtinger, X., Haschka, J. et al. Diagnosis and treatment of Paget’s disease of bone. Wien Med Wochenschr 167, 18–24 (2017). https://doi.org/10.1007/s10354-016-0502-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10354-016-0502-x