Abstract
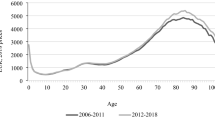
It is still an open question whether increasing life expectancy as such causes higher health care expenditures (HCE) in a population. According to the “red herring” hypothesis, the positive correlation between age and HCE is exclusively due to the fact that mortality rises with age and a large share of HCE is caused by proximity to death. As a consequence, rising longevity—through falling mortality rates—may even reduce HCE. However, a weakness of many previous empirical studies is that they use cross-sectional evidence to make inferences on a development over time. In this paper, we analyse the impact of rising longevity on the trend of HCE over time by using data from a pseudo-panel of German sickness fund members over the period 1997–2009. Using (dynamic) panel data models, we find that age, mortality and 5-year survival rates each have a positive impact on per-capita HCE. Our explanation for the last finding is that physicians treat patients more aggressively if the results of these treatments pay off over a longer time span, which we call “Eubie Blake effect”. A simulation on the basis of an official population forecast for Germany is used to isolate the effect of demographic ageing on real per-capita HCE over the coming decades. We find that, while falling mortality rates as such lower HCE, this effect is more than compensated by an increase in remaining life expectancy so that the net effect of ageing on HCE over time is clearly positive.



Similar content being viewed by others
Notes
A recent survey can be found in Karlsson and Klohn [22].
For instance, one criterion in organ allocation is expected organ functioning duration.
The empirical literature shows that some physicians use age as a prioritisation criterion in allocating scarce health care resources; for an overview, see Strech et al. [30].
Fang et al. [12] attribute the same quotation to the baseball star Mickey Mantle and speak of a “Mickey Mantle effect”. However, it is quite clear that Mantle did not invent the phrase, but quoted the football player Bobby Lane, who died in late 1986 and may well have known the statement by Blake, which had been made in February 1983.
See, e.g., the fact sheet on cancer edited by the National Institutes of Health, which is published online at http://report.nih.gov/nihfactsheets/Pdfs/Cancer(NCI).pdf.
This point is also made by van Baal and Wong [32].
The social health insurance system covers about 90 % of the population in Germany.
Expenditures for long-term care are not covered under Social Health Insurance.
We thank Dirk Göpffarth, the Head of the Risk Adjustment Unit at BVA, for making this dataset available to us.
Technically, we run a regression of \((SR5_{c-5,a,t-5}, \ldots, SR5_{c-1,a,t-1})'\) on a constant and a linear time trend, i.e.
$$ SR5_{c-\tau,a,t-\tau} = \mu_0 - \mu_1 \tau + \varepsilon \quad \hbox{ for } \quad \tau=1, \dots, 5, $$and determine the prediction as \(\widehat{SR5}_{c,a,t} = \hat{\mu}_0 - \hat{\mu}_1 \cdot 0 = \hat{\mu}_0\). For each prediction, a separate regression is performed. As these equations are estimated for every age, there is implicitly an interaction between age and year in this estimation. In contrast, there is no age-year interaction term in the equation for HCE; this difference is used for identification.
A possible concern might be that the mortality rate and SR5 are highly correlated and thus the effect of the two variables cannot be disentangled empirically. However, this is not the case; we return to this issue in the fifth section.
For the robustness checks, we also use the variables \(SR2_{c,a,t}, SR3_{c,a,t}, \dots SR10_{c,a,t}\), i.e., the predicted 2-year survival rate, 3-year survival rate, and so on.
Of course, dropping one of the variables means imposing the restriction that all coefficients of this variable are zero. However, since this is usually not made explicit, we mention it as a separate way to deal with the problem of linear dependence.
Because of the way the Intrinsic Estimator is implemented in Stata’s apc_ie command, in practice the estimates of the Intrinsic Estimator may differ slightly from the results of the partial least squares regression. In our data, we find the difference between the estimates using the Partial Least Squares Regression procedure of the software package R and Stata’s apc_ie command to be negligible. Since we perform the other regressions in Stata, we present the results for the Intrinsic Estimator.
Results are very similar when clustering at the age or year level.
We thank an anonymous referee for this suggestion.
Another way to deal with this would be to include proxy-variables; however, such variables will be difficult to find because they would have to be recorded in an age-specific way.
Regression (1) in first differences is referred to as regression (11), and in second differences as regression (21), and so on.
As we had to drop the age group 90+ in our estimations, in all the simulations we present, we use the predicted value of HCE for the 89 year olds as the predicted value of the age group 90+.
The columns are numbered as in Table 3 to indicate on which regressions the simulations are based. Table 9 refers only to the regressions in levels using the Intrinsic Estimator. Simulations based on the regressions in first and second differences and on the GMM regressions can be found in Tables 13 and 14 in the “Appendix”.
We emphasize again that these results do not at all depend on how the problem of linear dependence between age, period and cohort is solved.
References
Arellano, M., Bond, S.: Some tests of specification for panel data: Monte Carlo evidence and an application to employment equations. Rev. Econ. Stud. 58(2), 277–297 (1991)
Bech, M., Christiansen, T., Khoman, E., Lauridsen, J., Weale, M.: Ageing and health care expenditure in EU-15. Eur. J. Health Econ. 12(5), 469–478 (2011)
Blundell, R., Bond, S.: Initial conditions and moment restrictions in dynamic panel data models. J. Econom. 87(1), 115–143 (1998)
Breyer, F., Felder, S.: Life expectancy and health care expenditure: A new calculation for Germany using the costs of dying. Health Policy 75(2), 178–186 (2006)
Breyer, F., Hupfeld, S.: Fairness of public pensions and old-age poverty. FinanzArchiv 65, 358–380 (2009)
Callahan, D.: Setting Limits: Medical Goals in an Aging Society. New York (1987)
Colombier, C., Weber, W.: Projecting health-care expenditure for Switzerland: further evidence against the ‘red-herring’ hypothesis. Int. J. Health Plan. Manag. 26(3), 246–263 (2011)
Crimmins, E.M., Saito, Y., Ingegneri, D.: Trends in disability-free life expectancy in the United States, 1970–90. Popul. Dev. Rev. 23(3), 555–572 (1997)
Daniels, N.: Just Health Care. Cambridge University Press, Cambridge (1985)
Davidson, R., MacKinnon, J.G.: Estimation and Inference in Econometrics. New York (1993)
Deaton, A.: Panel data from time series of cross-sections. J. Econom. 30(1–2), 109–126 (1985)
Fang, H., Keane, M., Khwaja, A., Salm, M., Silverman, D.: Testing the mechanisms of structural models: The case of the Mickey mantle effect. Am. Econ. Rev. Papers Proc. 97(2), 53–59 (2007)
Felder, S., Werblow, A., Zweifel, P.: Do red herrings swim in circles? Controlling for the endogeneity of time to death. J. Health Econ. 29(2), 205–212 (2010)
Fuchs, V.: Though much is taken: Reflections on aging, health and medical care. Milbank Mem. Fund Q. Health Soc. 62(2), 143–166 (1984)
Hagist, C., Klusen, N., Plate, A., Raffelhüschen, B.: Social Health Insurance—the Major Driver of Unsustainable Fiscal Policy?, CESifo Working Paper; No. 1574 (2005)
Hagist, C., Kotlikoff, L.: Who’s Going Broke? Comparing Growth in Healthcare costs in ten OECD Countries, NBER Working Paper; w11833 (2005)
Harris, R., Tzavalis, E.: Inference for unit roots in dynamic panels where the time dimension is fixed. J. Econom. 91(2), 201–226 (1999)
Human Mortality Database: University of California, Berkeley (USA), and Max Planck Institute for Demographic Research (Germany). Available at http://www.mortality.org or http://www.humanmortality.de (data downloaded on May 31, 2011) (2011)
Hurst, S.A., Slowther, A.-M., Forde, R., Pegoraro, R., Reiter-Theil, S., Perrier, A., Garrett-Mayer, E., Danis, M.: Prevalence and determinants of physician bedside rationing. Data from Europe. J. Gen. Intern. Med. 21(11), 1138–1143 (2006)
Im, K., Pesaran, M., Shin, Y.: Testing for unit roots in heterogeneous panels. J. Econom. 115, 53–74 (2003)
Inkmann, J., Klotz, S., Pohlmeier, W.: Permanente Narben oder temporäre Blessuren? Eine Studie über die langfristigen Folgen eines missglückten Einstiegs in das Berufsleben auf der Grundlage von Pseudo-Panel-Daten. In: Pfeiffer, F., Pohlmeier, W. (eds) Qualifikation Weiterbildung und Arbeitsmarkterfolg, pp. 223–255. Nomos, Baden-Baden (1998)
Karlsson, M., Klohn, F.: Testing the red herring hypothesis on an aggregated level: ageing, time-to-death and care costs for older people in Sweden. Eur. J. Health Econ. (forthcoming)
Miller, T.: Increasing longevity and medicare expenditures. Demography 38(2), 215–226 (2001)
Riley, G.F., Lubitz, J.D.: Long-term trends in medicare payments in the last year of life. Health Serv. Res. 45(2), 565–576 (2010)
Roodman, D.: “How to Do xtabond2: An Introduction to “Difference” and “System” GMM in Stata,” Center for Global Development Working Paper 103 (2006)
Seshamani, M., Gray, A.: Ageing and health-care expenditure: The red herring argument revisited. Health Econ. 13, 303–314 (2004)
Shang, B., Goldman, D.: Does age or life expectancy better predict health care expenditures?. Health Econ. 17(4), 487–501 (2008)
Statistisches Bundesamt: 12. koordinierte Bevölkerungsvorausberechnung. Wiesbaden (2009)
Stearns, S., Norton, E.: Time to include time to death? The future of health care expenditure predictions. Health Econ. 13(4), 315–327 (2004)
Strech, D., Synofzik, M., Marckmann, G.: How physicians allocate scarce resources at the bedside: A systematic review of qualitative studies. J. Med. Philos. 33(1), 80–99 (2008)
Tu, Y.-K., Krämer, N., Lee, W.-C.: Addressing the identification problem in age-period-cohort analysis. Epidemiology 23(4), 583–593 (2012)
van Baal, P.H., Wong, A.: Time to death and the forecasting of macro-level health care expenditures: Some further considerations. J. Health Econ. 31(6), 876–887 (2012)
von Gaudecker, H.-M., Scholz, R.: Differential mortality by lifetime earnings in Germany. Demographic Research. 17(4), 83–108 (2007)
Werblow, A., Felder, S., Zweifel, P.: Population ageing and health care expenditure: A school of red herrings?. Health Econ. 146(10), 1109–1126 (2007)
Yang, Y., Schulhofer-Wohl, S., Fu, W., Land, K.: The intrinsic estimator for age-period-cohort analysis: What it is and how to use it. Am. J. Sociol. 113(6), 1697–1736 (2008)
Zweifel, P., Felder, S., Meier, M.: Ageing of population and health care expenditure: a red herring?. Health Econ. 8(6), 485–496 (1999)
Zweifel, P., Felder, S., Werblow, A.: Population ageing and health care expenditure: New evidence on the red herring. Geneva Papers Risk Insur. Issues Pract. Spec. Issue Health Insur. 29(4), 652–666 (2004)
Zweifel, P., Steinmann, L., Eugster, P.: The Sisyphus syndrome in health revisited. Int. J. Health Care Financ. Econ. 5(2), 127–145 (2005)
Acknowledgments
We are grateful to the Bundesversicherungsamt, Bonn, for the provision of the health care expenditure dataset, to the Statistische Bundesamt, Wiesbaden, for the provision of the demographic data, and to an anonymous referee for helpful suggestions. Valuable comments by James Binfield, Ralf Brüggemann, Terkel Christiansen, Victor R. Fuchs, Martin Karlsson, Florian Klohn, Winfried Pohlmeier, Niklas Potrafke, Esther Schuch and Volker Ulrich are gratefully acknowledged.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Breyer, F., Lorenz, N. & Niebel, T. Health care expenditures and longevity: is there a Eubie Blake effect?. Eur J Health Econ 16, 95–112 (2015). https://doi.org/10.1007/s10198-014-0564-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10198-014-0564-x