Abstract
Purpose
To document and analyse the decision to withhold or withdraw life-sustaining treatment (LST) in a population of very old patients admitted to the ICU.
Methods
This prospective study included intensive care patients aged ≥ 80 years in 309 ICUs from 21 European countries with 30-day mortality follow-up.
Results
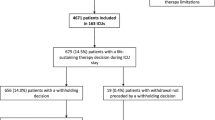
LST limitation was identified in 1356/5021 (27.2%) of patients: 15% had a withholding decision and 12.2% a withdrawal decision (including those with a previous withholding decision). Patients with LST limitation were older, more frail, more severely ill and less frequently electively admitted. Patients with withdrawal of LST were more frequently male and had a longer ICU length of stay. The ICU and 30-day mortality were, respectively, 29.1 and 53.1% in the withholding group and 82.2% and 93.1% in the withdrawal group. LST was less frequently limited in eastern and southern European countries than in northern Europe. The patient-independent factors associated with LST limitation were: acute ICU admission (OR 5.77, 95% CI 4.32–7.7), Clinical Frailty Scale (CFS) score (OR 2.08, 95% CI 1.78–2.42), increased age (each 5 years of increase in age had a OR of 1.22 (95% CI 1.12–1.34) and SOFA score [OR of 1.07 (95% CI 1.05–1.09 per point)]. The frequency of LST limitation was higher in countries with high GDP and was lower in religious countries.
Conclusions
The most important patient variables associated with the instigation of LST limitation were acute admission, frailty, age, admission SOFA score and country.
Trial registration
ClinicalTrials.gov (ID: NTC03134807).
Similar content being viewed by others
Among 5021 very old (≥ 80 years) patients admitted to 309 ICUs in 21 European countries, the most important patient variables associated with the instigation of life-sustaining treatment (LST) limitation were acute admission, frailty, age and SOFA score. The frequency of LST limitation was higher in countries with high GDP and lower where more inhabitants considered their religion’s deity very important. For patients with only a withholding decision, ICU and 30-day mortality were respectively 29.1 and 53.1%. |
Introduction
Life expectancy in many countries is steadily increasing. As a result, patients admitted to hospital and ultimately to the ICU will be older. At present, > 10% of the patients admitted to the ICU are ≥ 80 years old [1]. The proportion of older adults is estimated to increase to 30% by 2050, with a huge impact on total hospital expenditures [2]. As a consequence, many ICUs across the globe must adapt their policies to these increased demands. Some estimate that the need for ICU beds will increase by 50% owing to these developments [3]. However, once an older adult has been admitted to the ICU for an acute medical reason, his/her risk of dying within 30 days is high. For frail patients the 30-day mortality is 40.7% [4].
As a result, ICU physicians are increasingly faced with difficult decisions on continuation of life sustaining treatment (LST) in older adults. In these situations, decisions are being made to withhold LST if patients deteriorate or even to withdraw already instigated LST if the short-term prognosis is poor. Differences in ethics, religion, culture and predictive capacity add to the difficulty of formulating a consistent approach to treatment limitation in critical illness. Previous publications have highlighted the huge variation in admission policies for older adults in Europe [1, 5, 6]. At present, there is a strong consensus that age should not be considered as a sole decision-making criterion [7,8,9]. Older adults (like any other patients) should be admitted to the ICU only with a predefined, reasonable goal of care. Finally, considering their inherent frailty, all older adults should undergo systematic reassessment a few days after ICU admission to evaluate the appropriateness of their level of care. This concept of an “ICU trial” is attractive and has been proposed for cancer patients requiring mechanical ventilation [11]. However, this should be well organised, explicit, and shared with all ICU staff and the patients’ relatives. In most cases, important information is lacking when deciding to admit an older patient in ICU: no living will, incomplete information, and no clarity concerning life expectancy.
Differences in admission policies and health care systems, together with insufficient information from the patients or their relatives (i.e. advanced directives), result in huge variability in end-of-life (EOL) care in the ICU [12]. In addition, there is considerable variation in the proportion of deaths that occur after a decision to limit life support and this cannot be explained solely by patient characteristics [13, 14] or patients’ preferences [15]. In the present study we aim to examine the incidence and determinants of LST limitation decisions (withholding and withdrawal) in patients older than 80 years admitted to ICUs in European countries.
Methods
Study design and setting
The methods and patients have been described in a previous publication [4]. Briefly, VIP1 is a prospective European multicentre study. Each participating ICU could choose to include either consecutive patients throughout a 3-month period or the first 20 consecutive patients within this period. Individual ICUs started data collection between October 2016 and February 2017, depending on the speed of local ethics committee approval. A website was set up to facilitate sharing of information about the study and to allow data entry using an electronic case report form (CRF). The study was registered on ClinicalTrials.gov (ID: NTC03134807).
Participants
All patients aged 80 years or older admitted to the participating ICUs were eligible. Patients were followed until death or for 30 days after ICU admission.
Variables
The study collected a consistent set of data: age, gender, reason for ICU admission from a predefined list of 12 categories, length of stay (LOS) prior to ICU admission, Clinical Frailty Scale (CFS) score [16], admission SOFA score [17], any period of non-invasive or invasive ventilation with endotracheal intubation or tracheostomy during the ICU stay, use of vasoactive drugs, and renal replacement therapy. Severity scores such as SAPS2 were optional. ICU outcome (death or survival) and survival at day 30 after ICU discharge were collected for all included patients. All decisions to withhold and/or withdraw therapy were at the discretion of the treating physician(s) but were documented according to international recommendations [18]. However, we did not collect information on the timing of such a decision relative to ICU admission and/or commencement of organ support.
The CRF and database ran on a secure server at Aarhus University, Denmark.
Country’s characteristics
Gross domestic product (GDP) and health expenditure from individual countries were extracted from EUROSTAT (http://ec.europa.eu/eurostat/statistics-explained/index.php/Healthcare_expenditure_statistics). Proportions of elderly patients per country were extracted from Health at a Glance 2013: OECD Indicators. Numbers of ICU beds per inhabitants were extracted from data derived from Rhodes et al. [37].
Data on religious beliefs were extracted from the European Values Study (http://www.europeanvaluesstudy.eu/).
Bias and study size
The participating ICUs included consecutive patients, and decisions to withhold or withdraw LST were documented. The relationship with 30-day outcome was assessed retrospectively after closure of the database. No formal sample-size calculation was performed for this observational study.
Statistical analysis
Baseline patient characteristics, treatment and outcomes were compared among three LST groups: (1) no limitations, (2) withholding alone and (3) withdrawal, whether or not preceded by a withholding decision. Continuous variables were compared among the groups using the Mann–Whitney U test, categorical variables using the Chi squared test. Normally distributed continuous data were described as medians with 25th to 75th percentiles (interquartile range, IQR). Associations between variables and treatment limitation—i.e. withholding or withdrawal of LST—were estimated using a logistic regression model. To account for the clustering of patients within countries, a multilevel logistic regression model was used. Two models were built to estimate (a) the effect of patient characteristics on treatment limitation and (b) the effect of patient and country characteristics on treatment limitation. In order to quantify the country effect, we used intraclass coefficient correlation (ICC) and median odds ratio (MOR). The ICC represents the proportion of the total observed individual variation in the outcome (treatment limitation, i.e. withholding or withdrawal) that is attributable to between-country variation. The higher this proportion, the higher is the general contextual effect. If one were to repeatedly sample at random two subjects with the same covariates from different countries, then the MOR is the ratio between the subject at higher risk of the outcome and the subject at the lower risk of the outcome (differences in risk are entirely quantified by the country-specific random effects).
Standardized treatment limitation ratios were estimated for each country, defined as the ratio of the observed number of treatment limitations in a country and the sum of the predicted individual probabilities of treatment limitation (estimated from model 1) in the same country. The 95% confidence intervals of the ratios were estimated using Byar’s approximation.
Associations between variables and survival at 30 days after ICU admission were estimated using a Cox proportional hazard regression model. All patients were censored at 30 days. Adjusted survival curves were produced using inverse probability weighting. The weights were estimated using frailty, age, gender, type of admission and SOFA score. Mid-point imputations were used for patients discharged from ICU and dead at day 30. A p value less than 0.05 was considered to show a statistically significant difference.
All analyses were performed with R software, version 3.2.2 (R Foundation for Statistical Computing).
Ethics
Institutional research ethics board approval was obtained from each study site. No specific funding was received, but the study was endorsed by ESICM.
Results
In total, 309 ICUs from 21 European countries participated and included 5132 patients. Follow-up at 30 days was completed in 98% (5021/5132) of the patients. The median recruited number of patients per country was 114 and the median number of patients per ICU was 16. The median age of all patients was 84 years (IQR 81–86); 52.1% were male. See Table 1 for more baseline characteristics.
Patients with no LST limitation accounted for 3656/5021 (72.8%) patients with only withholding comprised 15.0% and patients with withdrawal (including those with previous withholding) made up 12.2% of the total. Patients with LST limitation were older, more frail, more severely ill and less frequently electively admitted (Table 1). Patients with withdrawal of LST were more frequently male and had a longer ICU LOS. The proportion of LST limitations varied according to diagnostic category (ESM3), with a very low frequency for patients admitted after elective surgery. Among the non-survivors at day 30, 24.3% had a withholding and 34.6% had a withdrawing LST decision (ESM5). The ICU and 30-day mortality were respectively 29.1 and 53.1% in the withholding group and 82.2 and 93.1% in the withdrawal group. The unadjusted and adjusted survival curves are depicted in Fig. 1.
Provision of organ support also differed according to LST decision, with more instances of organ supports in the withdrawal group (Table 2).
LST limitation was less frequent in eastern and southern European countries than in other parts of Europe (ESM6). The ICUs located in northern Europe had higher rates of LST limitation (up to 45.2%).
Country was found to have a significant effect on the decision whether or not to limit LST. The multivariate analysis identified independent factors for LST limitation decision (Table 3). The most important patient factors associated with LST limitation were: acute ICU admission, CFS score, higher age and admission SOFA score. A sensitivity analysis focusing only on urgent admission, thus excluding scheduled surgery, found similar results. Among the different country characteristics (ESM1) and patient characteristics (ESM2), high GDP was associated with a higher rate of LST limitation, while religiosity, defined as the proportion of inhabitants agreeing with the statement “God is important”, was associated with low rates of LST limitation (Table 3) (Fig. 2). The number of ICU beds and the age distribution of the population had no impact on LST limitation.
The ICC was 0.14 (empty model), 0.23 (model with individual patient characteristics) and 0.08 (model with individual patient and country level characteristics). In this last model, 8% of the total variation in patients’ treatment limitation is due to country.
The MOR was 2.06 (empty model), 2.57 (model with individual patient characteristics) and 1.66 (model with individual patient and country level characteristics). When comparing two patients with the same frailty level, age, gender, SOFA score and type of admission from randomly selected countries, the MOR for the patient from the country with the higher risk of treatment limitation relative to the patient from the country with the lower risk of treatment limitation was 1.66. Thus, in half such comparisons, the odds of treatment limitation would be less than 1.66 for a patient in the country of higher risk relative to an “identical” patient in the country of lower risk.
Among patients with withdrawal, invasive mechanical ventilation was highly associated with LST limitation decisions (ESM6).
Discussion
Our prospective European study included 5021 patients aged 80 years or older. Limitation of LST was instigated in 27.2% of these patients. Such limitations were associated with 30-day mortality of 54.8% in the withholding group and 94.2% in the withdrawal group. In this very old patient population, several factors other than chronological age are associated with limitations in LST, such as country, urgent admission, frailty and severity of illness (SOFA score).
Our findings are potentially important for policy makers. There was considerable geographical variation in preparedness to instigate limitations in LST in older adult patients. Using the MOR, we have shown that country effects (i.e. ‘culture’) are as important as, or in some instances more important than, patient characteristics in terms of the association with decisions to withhold or withdraw treatment. An advantage to use of the MOR for quantifying the contextual effect is that the MOR is on the same scale as that used for estimating measures of association when quantifying the effect of subject-level (and country-level) covariates on the odds of the outcome. Thus, one can compare the magnitude of the MOR with that of the association between characteristics of the subject and the outcome. In examining the odds ratios for the model including patient and country characteristics, we observed that only two of the six patient characteristics had an odds ratio above 1.66. Thus, the magnitude of the effect of clustering (the contextual effect) was higher than that of four of the six patient characteristics.
High GDP was associated with higher standardized treatment limitation ratio, while religiosity had the opposite effect. This may seem paradoxical, with more resources used in countries with lower GDP. From an ethical point of view, countries with low GDP potentially jeopardize the allocation of resources by postponing (or not formalizing) EOL decision making.
Such differences have been noted previously. For example, there is lower prevalence of withdrawal of life support in Asia than in the USA or in Europe [15, 19]. Regional variations have also been reported in the UK [20]. These studies suggest that although some variability is driven by ICU bed availability, much of the variability is driven by the views of individual physicians (culture, religion, profile) [21]. This indirectly indicates potential violation of the patients’ autonomy (besides inappropriate allocation of resources) and suggests physician- or culture-centred care instead of patient-centred care. In northern European countries intensivists are apparently more willing to withhold or withdraw LST than in eastern and southern European countries. In our study, this difference was even more striking for decisions to withdraw treatment: 5.5% in eastern Europe vs 17.7% in northern Europe. Religion may play a part: the European ETHICUS study reported that withholding occurred more often than withdrawal if the physician was Jewish (81%), Greek Orthodox (78%) or Moslem (63%) [22].
The rate of LST limitation in our study is higher than previously reported in the general ICU population. For example, LST was limited in 11.0% of patients in France [23] and 9.8% in Europe [22]. Several factors may explain these differences: a much younger population (the median age was 57 and 66, respectively, in the French and European studies); less severely ill patients (lower SAPS II scores, lower overall mortality); or the time when the study was conducted, with changes in the perceptions of society in general and ICU physicians in particular as the population ages.
Several studies have documented higher rates of treatment limitation in aged patients compared with their younger counterparts [18, 24,25,26]. In the SUPPORT study, older age was associated with higher rates of withholding ventilator support and dialysis in adjusted analyses [24, 25]. In a study by Hakim et al. in the USA, the rate of do-not-resuscitate orders increased with age (from 21% in patients < 54 years to 55% in patients > 84 years) [26]. In a study by Hoel et al. in Norway, medical and unscheduled surgical patients with LST limitation were older [27]. Other factors besides age have been associated with increased odds of decisions to forgo LST in US ICUs: female sex, white race, poor baseline functional status [13] and the treatments given to such patients [24].
In our study, the decision to limit LST was associated with increased 30-day mortality (54.8% in the withholding group and 94.2% in the withdrawal group). The same result was found in a recent multicentre observational study in France, in which withdrawing or withholding care accounted for half of all deaths [28]. In Italy, withdrawal or withholding preceded 62% of deaths [29]. In our study, among the elderly patients dead at day 30, 41.1% had no LST decision, 24.3% withholding and 34.6% withdrawal. However, it should be emphasised that a LST limitation decision is not equal to an EOL decision. In fact, among the elderly patients with a decision to withhold care, the ICU mortality and 30-day mortality were only 29.1 and 53.1%, respectively. For patients in whom LST was withdrawn, ICU mortality and 30-day mortality were 82 and 94.2%. Clearly, not all LST limitations are EOL decisions, since the mortality rate is low for patients with only withholding of treatment and not 100% at 30 days for patients with withdrawal of LST. Apparently, LST limitation is proposed when such LST is considered disproportionate to the patient’s chances of survival with a good quality of life [27, 30]. The impact of LST limitation on mortality is greatest in the first week of ICU treatment [31], depending on what kind of treatment is withdrawn and the number of organs failing at the time of LST limitation [31, 32]. We found that the impact of LST limitation on survival was discernible until 2 weeks after ICU admission (Fig. 1).
In our study, the ICU LOS of patients with LST withdrawal was a little longer than the other patients but was still below 3 days, suggesting an early decision to limit LST. In a study from Australia and New Zealand, the LOS of older adults was 3.9 days in non-survivors and 2.5 days in survivors, suggesting that EOL decisions were made later in patients older than 80 years [33]. On the other hand, data from Scandinavia show shorter LOS for non-survivors than survivors in the ICU, particularly for older patients [34].
Our study has several strengths: the focus on patients older than 80 years, the large number of participating ICUs from 21 European countries, the separate documentation of withholding and/or withdrawal of LST and the 30-day follow-up. However, it also has limitations. We have no documentation of the timing of the LST limitation decision, which could bias the results; patient inclusion was mostly during the winter, which may have contributed to the high rate of LST limitation; and the participating ICUs cannot necessarily be considered as representative of their countries. In order to combat these weaknesses, we grouped countries into five European regions; we did not document any possible influence of advance directives or patients’ and/or relatives’ preferences in the decision; and included no health economic data or bed access/pressure data that could help to develop a resource-based argument for deciding on LST limitation.
In the older adult population, LST limitation occurs frequently. The best criteria for the appropriateness of such decision include post-discharge functional capacity, mortality and quality of life [35]. A dialogue with family members (or care givers) about the possibilities and potential outcomes should take place within 72 h of a patient being admitted to the ICU [10, 21, 36].
Conclusion
Given the limited survival chances of very old patients and the cost and scarcity of ICU resources, an active policy for limiting life-sustaining therapy should be advocated for patients who are not responding to treatment or not willing to continue ICU treatment. This should be accompanied by a campaign encouraging patients to express their preferences and wishes before they become ill. Better definition of which elderly patients will benefit from ICU procedures, rather than drawing up exclusion criteria, is a challenge for future studies.
Change history
20 August 2018
In the original publication Dr Patrick Meybohm of the Department of Anaesthesiology, Intensive Care Medicine and Pain Therapy, Frankfurt University Hospital, Frankfurt, Germany was inadvertently omitted from the list of investigators.
References
Flaatten H, Artigas A, de Lange DW, Bin D, Moreno R, Christensen S, Joynt GM, Bagshaw SM, Sprung CL, Benoit D, Soares M, Guidet B (2017) The status of ICM research and a future agenda for very elderly patients in the ICU. Intensive Care Med 43:1319–1328
Angus D (2017) Admitting elderly patients to the intensive care unit—is it the right decision? JAMA 318:1443–1444
Laake JH, Dybwik K, Flaatten HK, Fonneland I-L, Kvåle R, Strand K (2010) Impact of the post-World War II generation on intensive care needs in Norway. Acta Anaesthesiol Scand 54:479–484
Flaatten H, De Lange D, Morandi A et al (2017) The impact of frailty on ICU and 30-day mortality and the level of care in very elderly patients (≥ 80 years). Intensive Care Med 43:4940–4948
Sprung CL, Danis M, Iapichino G, Artigas A, Kesecioglu J, Moreno R, Lippert A, Curtis JR, Meale P, Cohen SL, Levy MM, Truog RD (2013) Triage of intensive care patients: identifying agreement and controversy. Intensive Care Med 39:1916–1924
Boumendil A, Angus DC, Guitonneau AL, Menn AM, Ginsburg C, Takun K, Davido A, Masmoudi R, Doumenc B, Pateron D, Garrouste-Orgeas M, Somme D, Simon T, Aegerter Ph, Guidet B (2012) Variability of intensive care admission decisions for the very elderly. Plos One 7(1–11):e34387
Sprung CL, Woodcock T, Sjokvist P, Ricou B, Bulow HH, Lippert A, Maia P, Cohen S, Baras M, Hovilehto S, Ledoux D, Phelan D, Wennberg E, Schobersberger W (2008) Reasons, considerations, difficulties and documentation of end-of-life decisions in European intensive care units: the ETHICUS Study. Intensive Care Med 34:271–277
Guidet B, de Lange D, Flaatten H (2018) Should this elderly patient be admitted to the ICU. Intensive Care Medicine. https://doi.org/10.1007/s00134-018-5054-7 (Epub ahead of print)
Guidet B, De Lange DW, Christensen S, Moreno R, Fjølner J, Dumas G, Flaatten H (2018) Attitudes of physicians towards the care of critically ill elderly patients—a European survey. Acta Anaesthesiol Scand 62:207–219
Le Guen J, Boumendil A, Guidet B, Corvol A, Saint-Jean O, Somme D (2016) Are elderly patients’ opinions sought before admission to an intensive care unit? Results of the ICE-CUB study. Age Ageing 45:303–309
Lecuyer L, Chevret S, Thiery G, Darmon M, Schlemmer B, Azoulay E (2007) The ICU trial: a new admission policy for cancer patients requiring mechanical ventilation. Crit Care Med 35:808–814
Mark NM, Rayner SG, Lee NJ, Curtis JR (2015) Global variability in withholding and withdrawal of life-sustaining treatment in the intensive care unit: a systematic review. Intensive Care Med 41:1572–1585
Quill CM, Ratcliffe SJ, Harhay MO, Halpern SD (2014) Variation in decisions to forgo life-sustaining therapies in US ICUs. Chest 146(573–582):5
Hart JL, Harhay MO, Gabler NB, Ratcliffe SJ, Quill CM, Halpern SD (2015) Variability among US intensive care units in managing the care of patients admitted with preexisting limits on life-sustaining therapies. JAMA Intern Med 175:1019–1026
Barnato AE, Herndon MB, Anthony DL, Gallagher PM, Skinner JS, Bynum JP, Fisher ES (2007) Are regional variations in end-of-life care intensity explained by patient preferences?: a study of the US Medicare population. Med Care 45:386–393
Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I et al (2005) A global clinical measure of fitness and frailty in elderly people. CMAJ 173:489–495
Vincent JL, Moreno R, Takala J, Willatts S, de Mendonça A, Bruining H et al (1996) The SOFA (sepsis-related organ failure assessment) score to describe organ dysfunction/failure. On behalf of the working group on sepsis-related problems of the European Society of Intensive Care Medicine. Intensive Care Med 22:707–710
Guidet B, Hodgson E, Feldman C, Paruk F, Lipman J, Koh Y, Vincent JL, Azoulay E, Sprung C (2014) The Durban World Congress Ethics Round Table conference report: II. Withholding or withdrawing of treatment in elderly patients admitted to the Intensive Care Unit. J Crit Care 29:896–901
Sprung CL, Cohen SL, Sjokvist P, Baras M, Bulow HH, Hovilehto S, Ledoux D, Lippert A, Maia P, Phelan D, Schobersberger W, Wennberg E, Woodcock T; Ethicus Study Group (2003) End-of-life practices in European intensive care units: the Ethicus Study. JAMA 290:790–797
Wunsch H, Harrison DA, Harvey S, Rowan K (2005) End-of-life decisions: a cohort study of the withdrawal of all active treatment in intensive care units in the United Kingdom. Intensive Care Med 31(6):823–831
Curtis JR, Engelberg RA, Teno JM (2017) Understanding variability of end-of-life care in the ICU for the elderly. Intensive Care Med 43:194–196
Sprung CL, Maia P, Bulow HH, Ricou B, Armaganidis A, Baras M, Wennberg E, Reinhart K, Cohen SL, Fries DR, Nakos G, Thijs LG; Ethicus Study Group (2007) The importance of religious affiliation and culture on end-of-life decisions in European intensive care units. Intensive Care Med 33:1732–1739
Ferrand E, Robert R, Ingrand P, Lemaire F; French LATAREA Group (2001) Withholding and withdrawal of life support in intensive-care units in France: a prospective survey. French LATAREA Group. Lancet 357(9249):9–14
Hamel MB, Davis RB, Teno JM et al (1999) Older age, aggressiveness of care, and survival for seriously ill, hospitalized adults. SUPPORT Investigators. Study to understand prognoses and preferences for outcomes and risks of treatments. Ann Intern Med 131:721–728
Hamel MB, Teno JM, Goldman L et al (1999) Patient age and decisions to withhold life-sustaining treatments from seriously ill, hospitalized adults. SUPPORT Investigators. Study to understand prognoses and preferences for outcomes and risks of treatment. Ann Intern Med 130:116–125
Hakim RB, Teno JM, Harrell FE Jr et al (1996) Factors associated with do-not-resuscitate orders: patients’ preferences, prognoses, and physicians’ judgments. SUPPORT Investigators. Study to understand prognoses and preferences for outcomes and risks of treatment. Ann Intern Med 125:284–293
Hoel H, Skjaker SA, Haagensen R, Stavem K (2014) Decisions to withhold or withdraw life-sustaining treatment in a Norwegian intensive care unit. Acta Anaesthesiol Scand 58:329–336
Orban JC, Walrave Y, Mongardon N, Allaouchiche B, Argaud L, Aubrun F, Barjon G, Constantin JM, Dhonneur G, Durand-Gasselin J, Dupont H, Genestal M, Goguey C, Goutorbe P, Guidet B, Hyvernat H, Jaber S, Lefrant JY, Mallédant Y, Morel J, Ouattara A, Pichon N, Guérin Robardey AM, Sirodot M, Theissen A, Wiramus S, Zieleskiewicz L, Leone M, Ichai C, Network AzuRéa (2017) Causes and characteristics of death in intensive care units: a prospective multicenter study. Anesthesiology 126:882–889
Bertolini G, Boffelli S, Malacarne P, Peta M, Marchesi M, Barbisan C, Tomelleri S, Spada S, Satolli R, Gridelli B, Lizzola I, Mazzon D (2010) End-of-life decision-making and quality of ICU performance: an observational study in 84 Italian units. Intensive Care Med 36:1495–1504
Weimer JM, Nowacki AS, Frontera JA (2016) Withdrawal of life-sustaining therapy in patients with intracranial hemorrhage: self-fulfilling prophecy or accurate prediction of outcome? Crit Care Med 44:1161–1172
Lautrette A, Garrouste-Orgeas M, Bertrand PM, Goldgran-Toledano D, Jamali S, Laurent V, Argaud L, Schwebel C, Mourvillier B, Darmon M, Ruckly S, Dumenil AS, Lemiale V, Souweine B, Timsit JF; Outcomerea Study Group (2015) Respective impact of no escalation of treatment, withholding and withdrawal of life-sustaining treatment on ICU patients’ prognosis: a multicenter study of the Outcomerea Research Group. Intensive Care Med 41:1763–1772
Cooke CR, Hotchkin DL, Engelberg RA, Rubinson L, Curtis JR (2010) Predictors of time to death after terminal withdrawal of mechanical ventilation in the ICU. Chest 138(2):289–297
Bagshaw SM, Webb SA, Delaney A, George C, Pilcher D, Hart GK, Bellomo R (2009) Very old patients admitted to intensive care in Australia and New Zealand: a multi-centre cohort analysis. Crit Care 13:R45
Strand K, Walther SM, Reinikainen M, Ala-Kokko TI, Nolin T, Martner J et al (2010) Variations in the length of stay of intensive care unit nonsurvivors in three Scandinavian countries. Crit Care 14:R175
Guidet B, Leblanc G, Simon T, Woimant M, Quenot JP, Ganansia O, Maignan M, Yordanov Y, Delerme S, Doumenc B, Fartoukh M, Charestan P, Trognon P, Galichon B, Javaud N, Patzak A, Garrouste-Orgeas M, Thomas C, Azerad S, Pateron D, Boumendil A; ICE-CUB 2 Study Network (2017) Effect of systematic intensive care unit triage on long-term mortality among critically ill elderly patients in france: a randomized clinical trial. JAMA 318:1450–1459
Truog RD, Campbell ML, Curtis JR, Haas CE, Luce JM, Rubenfeld GD, Rushton CH, Kaufman DC (2008) Recommendations for end-of-life care in the intensive care unit: a consensus statement by the American College of Critical Care Medicine. Crit Care Med 36:953–963
Rhodes A, Ferdinande P, Flaatten H, Guidet B, Metnitz PG, Moreno RP (2012) The variability of critical care beds numbers in Europe. Intensive Care Med 38:1647–1653. https://doi.org/10.1007/s00134-018-5196-7
Acknowledgements
VIP1 study group members: René Schmutz, B5, Hospital of St. John of God Vienna , Austria; Franz Wimmer, Interne Intensiv, Kardinal Schwarzenberg´sches Krankenhaus, Austria; Philipp Eller, Intensivstation der Univ.-Klinik für Innere Medizin, Medical University Graz, Austria; Klemens Zotter, MICU, University Hospital Innsbruck, Austria; Pieter De Buysscher, Department of Intensive Care, AZ Sint-Lucas Ghent, Belgium; Nikolaas De Neve, Department of Intensive Care, O.L.Vrouwhospital Aalst , Belgium; Sandra Oeyen, Department of Intensive Care, Ghent University Hospital, Belgium; Walter Swinnen, Department of Intensive Care Medicine, AZ Sint-Blasius Dendermonde , Belgium; Bernardo Bollen Pinto, Peri-interventional Intermidate Care (SINPI), Geneva University Hospitals, Belgium; Paul Abraham, Adult Intensive Care (SIA), Geneva University Hospitals, Belgium; Leila Hergafi, Service des Soins intensifs, Hôpital fribourgeois, Fribourg, Belgium; Joerg C. Schefold, Universitätsklinik für Intensivmedizin, Inselspital, Bern University Hospital, University of Bern, Belgium; Ewelina Biskup, Medical ICU, University Hospital Basel, Belgium; Petr Piza, KARIP, IKEM, Checkoslovakia; Ioannis Taliadoros, CY001, Nicosia General Hospital, Cyprus; Jesper Fjølner, ITA, Randers Regional Hospital, Denmark; Nilanjan Dey, Intensiv Herning, Regions Hospital Herning, Denmark; Christoffer Sølling, I-25, Regionshospital Viborg, Denmark; Bodil Steen Rasmussen, ICU, Aalborg University Hospital, Denmark; Steffen Christensen, OPI Ost, Aarhus University Hospital Skejby, Denmark; Xavier Forceville, Réanimation médico chirurgical, Centre Hospitalier de Meaux, France; Guillaume Besch, Département d´Anesthésie Réanimation Chirurgicale, Centre Hospitalier Régional Universtaire de Besançon, France; Herve Mentec, Service de Réanimation Polyvalente, Centre Hospitalier Victor Dupouy Argenteuil, France; Philippe Michel, Réanimation médico-chirurgicale, CH Carnelle - Portes de l’Oise, France; Philippe Mateu, Réanimation Polyvalente, CH de Charleville-Mézières, France; Philippe Michel, Réanimation médico-chirurgicale, CH René Dubos, France; Lucie Vettoretti, Réanimation Médicale, CHRU de Besançon, France; Jeremy Bourenne, Reanimation des Urgences et Médicale, CHU Marseille - Timone, France; Nathalie MARIN, reanimation médicale, hopital cochin, France; Max Guillot, Réanimation médicale, Hôpital de Hautepierre, France; Naida Aissaoui , Réanimation médicale, hopital européen georges pompidou, France; Cyril Goulenok , Réanimation Médicale, Hopital Privé Jacques CARTIER, France; Nathalie Thieulot-Rolin , Intensive care medicine department, Hospital Marc Jacquet 77000 Melun, France; Jonathan Messika, Réanimation Médico-Chirurgicale, Louis Mourier, France; Lionel Lamhaut, Polyvalente adult ICU, Necker (APHP), France; Bertrand Guidet, Réanimation médicale, Saint Antoine, France; Cyril Charron, Medical-surgical ICU, University Hospital Ambroise Paré, de Paris Boulogne-Billancourt, France, France; Alexander Lauten, 1) Department of Cardiology, 2) DZHK Berlin partner side, Charité Universitaetsmedizin Berlin, Germany; Anna Lena Sacher, Department of Anesthesiology , Charité Universitaetsmedizin Berlin, Germany; Thorsten Brenner, Department of Anesthesiology, Heidelberg University Hospital, Germany; Marcus Franz, Department of Internal Medicine, Jena University Hospital, Friedrich-Schiller University, Germany; Frank Bloos, Department of Anesthesiology, Jena University Hospital, Friedrich-Schiller University, Germany; Henning Ebelt, Department for Medicine II, Catholic Hospital “St. Johann Nepomuk”, Germany; Stefan J Schaller, Department of Anesthesiology, Klinikum rechts der Isar, Technical University of Munich, Munich, Germany; Kristina Fuest, Department of Anesthesiology, Klinikum rechts der Isar, Technical University of Munich, Munich, Germany, Germany; Christian Rabe, Department Of Clinical Toxicology, Klinikum rechts der Isar, Technical University of Munich, Munich, Germany, Germany; Thorben Dieck, Department of Anaesthesiology and Intensive Care, Medical School Hospital Hannover, Germany; Stephan Steiner, Department of Cardiology, Pneumology and Intensive Care, St. Vincenz Krankenhaus Limburg, Germany; Tobias Graf, Department of Cardiology, University Heart Center Luebeck, Germany; Amir M Nia, Division of Cardiology and Intensive Care, University Hospital Düsseldorf, Heinrich-Heine University, Germany; Christian Jung, Division of Cardiology and Intensive Care, University Hospital Düsseldorf, Heinrich-Heine University, Germany; Rolf Alexander Janosi, Department of Cardiology and Vascular Diseases, University Hospital Essen, Germany; Philipp Simon, Department of Anaesthesiology and ICM, University Hospital of Leipzig, Germany; Stefan Utzolino, Department of General and Visceral Surgery , Universitätsklinikum Freiburg, Germany; Tim Rahmel, Department of Anaesthesiology, Intensive Care Medicine, University Hospital Knappschaftskrankenhaus Bochum, Germany; Eberhard Barth, Department of Anaesthesiology, University of Ulm, Germany; Christian Jung, University Hospital Düsseldorf, Heinrich-Heine-University Düsseldorf, Medical Faculty, Division of Cardiology, Pulmonology and Vascular Medicine, Düsseldorf, Germany, Germany; Michael Schuster, Department of Anaesthesiology, University Hospital Mainz, Germany; Zoi Aidoni , ICU, UGHT AHEPA, Greece; Stavros Aloizos , ICU , Army Share Fund Hospital, Athens, Greece; Polychronis Tasioudis , ICU, G. Gennimatas hospital of Thessaloniki, Greece; Kleri Lampiri , ICU, General Hospital Of Kavala, Greece; Vasiliki Zisopoulou, ICU1, General Hospital Of Larissa, Greece; Ifigenia Ravani , ICU, General hospital of Patras, Greece; Eumorfia Pagaki , ICU, General hospital of Trikala, Greece; Angela Antoniou , ICU, Volos General Hospital, Greece; Theodoros A. Katsoulas, ICU, “Ag Anargyroi” General Hospital, Greece; Aikaterini Kounougeri , ICU , Konstantopouleion General Hospital, Athens, Greece; George Marinakis, ICU, “Korgialenio-Benakio” G. Hospital of Athens, Greece; Fotios Tsimpoukas, ICU, Lamia General Hospital, Greece; Anastasia Spyropoulou, ICU, Panarkadian General Hospital of Tripolis, Greece; Paris Zygoulis, General ICU, University hospital of Larisa, Greece; Aikaterini Kyparissi , ICU, “HIPPOCRATEIO” General Hospital of Athens , Greece; Manish Gupta , MICU, MAX SUPER SPECIALTY HOSPITAL , Vaishali , India; Mohan Gurjar, Department of Critical Care Medicine, Sanjay Gandhi Postgraduate Institute of Medical Sciences , India; Ismail M Maji , MICU, St Johns Medical Colleg Hospital, Bangaluri, India; Ivan Hayes, CUH GICU, Cork University Hospital, Ireland; Brian Marsh, Department of Critical Care Medicine, Mater Misericordiae University Hospital, Ireland; Yvelynne Kelly, General ICU, St. Jamess Hospital, Ireland; Andrew Westbrook, ICU, St. Vincents University Hospital, Ireland; Gerry Fitzpatrick, Tallaght intensive Care, Tallaght Hospital, Ireland; Darshana Maheshwari, UHG ICU, University hospital galway, Ireland; Catherine Motherway, ICU, University Hospital limerick, Ireland; Giovanni Negri, Rianimazione, A.S.S.T. Ovest Milanese - Presidio Di Magenta - Ospedale G. Fornaroli (Magenta), Italy; Savino Spadaro, Unità di Terapia Intensiva del Servizio di Anestesia , Azienda Ospedaliera Universitaria Sant Anna (Ferrara), Italy; Giuseppe Nattino, Rianimazione generale, ASST Lecco - Ospedale A.Manzoni (Lecco), Italy; Matteo Pedeferri, Rianimazione, AO della Provincia di Lecco - Presidio Ospedaliero S.Leopoldo Mandic, Merate , Italy; Annalisa Boscolo, Giustiniani I e II (Istar), Azienda Ospedaliera di Padova (Padova), Italy; Simona Rossi, Servizio Anestesia Rianimazione, Azienda Ospedaliera G.Salvini - Presidio Ospedaliero di Rho , Italy; Giuseppe Calicchio, Centro di Rianimazione, Azienda Ospedaliera Universitaria San Giovanni di Dio e Ruggi d’Aragona , Italy; Lucia Cubattoli, Rianimazione Generale , Azienda Ospedaliera Universitaria Senese (Siena), Italy; Gabriella Di Lascio, Terapia Intensiva di Emergenza, Azienda Ospedaliero Universitaria Careggi (Firenze), Italy; Maria Barbagallo, UO 2 Anestesia Rianimazione Terapia Intensiva, Azienda Ospedaliero-Universitaria di Parma (Parma), Italy; Francesco Berruto, rianimazione, Ospedale E. Agnelli (Pinerolo), Italy; Daniela Codazzi, Unità Terapia Intensiva, Fondazione IRCCS Istituto Nazionale dei Tumori (Milano), Italy; Andrea Bottazzi, Rianimazione 2, Fondazione IRCCS Policlinico S.Matteo (Pavia), Italy; Paolo Fumagalli, Rianimazione 1, Fondazione Policlinico San Matteo (Pavia), Italy; Giancarlo Negro, Anestesia e Rianimazione 1, Ospedale Francesco Ferrari (Casarano), Italy; Giuseppe Lupi, Servizio Anestesia e Rianimazione, Ospedale Maggiore (Cremona), Italy; Flavia Savelli, Anestesia e Rianimazione - TI 2, Ospedale Maurizio Bufalini (Cesena), Italy; Giuseppe A. Vulcano, Terapia Intensiva, Ospedale Civile Nicola Giannettasio (Rossano), Italy; Roberto Fumagalli, Anestesia e Rianimazione 1, Ospedale Niguarda Ca’ Granda (Milano), Italy; Andrea Marudi, Rianimazione Neurorianimazione, Nuovo Ospedale Civile Sant Agostino Estense (Modena), Italy; Ugo Lefons, Terapia intensiva, Ospedale Alta Val d’Elsa (Poggibonsi), Italy; Rita Lembo, Rianimazione generale, Ospedale Castelli di Verbania (Verbania), Italy; Maria Babini, Servizio Anestesia e Rianimazione, Ospedale Civile Lugo (Lugo), Italy; Alessandra Paggioro, Struttura Semplice di Rianimazione e Terapia Intensiva, Ospedale degli Infermi di Biella - ASL BI (Biella), Italy; Vieri Parrini, Anestesia e Rianimazione, Ospedale del Mugello (Borgo San Lorenzo), Italy; Maria Zaccaria, Rianimazione e Terapia Intensiva, Ospedale di Ciriè (Torino), Italy; Stefano Clementi, terapia intensiva polivalente, Ospedale di Sesto San Giovanni (Sesto San Giovanni), Italy; Carmelo Gigliuto, Rianimazione, Ospedale di Vigevano - Azienda Ospedaliera della Provincia di Pavia (Vigevano), Italy; Francesca Facondini, Reparto di Rianimazione e Terapia Intensiva, Ospedale Infermi (Rimini), Italy; Simonetta Pastorini, Servizio Anestesia-Rianimazione , Ospedale P. Cosma-AUSL 15 Alta padovana (Camposampiero), Italy; Susanna Munaron, Unità di Terapia Intensiva, Ospedale San Giacomo (Castelfranco Veneto), Italy; Italo Calamai, Rianimazione, Ospedale San Giuseppe (Empoli), Italy; Anna Bocchi, Terapia Intensiva, Ospedale San Luca (Trecenta), Italy; Adele Adorni, Unità di Terapia Intensiva Rianimatoria, Ospedale Valduce (Como), Italy; Maria Grazia Bocci, Centro di Rianimazione, Policlinico Agostino Gemelli (Roma), Italy; Andrea Cortegiani, Unità di Terapia Intensiva Polivalente, Policlinico P. Giaccone. University of Palermo, Italy; Tiziana Casalicchio, Terapia Intensiva, Ospedale San Giovanni Bosco (Torino), Italy; Serena Mellea, Unità di Terapia Intensiva, Ospedale Santa Maria della Misericordia (Perugia), Italy; Elia Graziani, Unità Operativa Anestesia e Rianimazione, Santa Maria delle Croci (Ravenna), Italy; Massimo Barattini, Rianimazione, Ospedale Santa Maria Nuova (Firenze), Italy; Elisabetta Brizio, Servizio di Rianimazione, Ospedale SS Annunziata, Italy; Maurizio Rossi, UO Anestesia e Rianimazione, Azienda Ospedaliera Sant’Anna Como – Presidio di Menaggio, Italy; Michael Hahn, ICU, Haugesund hospital, Norway; Hans Flaatten, General ICU, Haukeland University Hospital, Norway; Nicolai Kemmerer, ICU, Kongsberg hospital, Norway; Hans Frank Strietzel, ICU, Kristiansund Hospital, Norway; Knut Dybwik, ICU, Nordlandssykehuset Bodo, Norway; Terje Legernaes, ICU , Hamar hospital, Norway; Pål Klepstad, Dept Intensive Care Medicine, St Olavs University Hospital, Norway; Even Braut Olaussen, ICU, Stavanger University Hospital, Norway; Knut Inge Olsen, ICU, Namsos Hospital, Norway; Ole Marius Brresen, ICU, Telemark Hospital, Skien, Norway; Geir Bjorsvik, ICU , University Hospital Tromso, Norway; Finn H. Andersen, ICU, Ålesund hospital, Norway; Sameer Maini, Medical ICU, Aalesund Hospital, Norway; Lutz Fehrle, ICU, Molde hospital, Norway; Miroslaw Czuczwar, ICU, First Public Teaching Hospital in Lublin, Poland; Pawel Krawczyk, ICU, University Hospital in Krakow, Poland; Mirosław Ziętkiewicz, Respiratory and Thoracic Surgical ICU, John Paul II Hospital in Krakow, Poland; Łukasz R. Nowak, Department of Anaesthesiology and Intensive Care, Maria Sklodowska-Curie Memorial Institute of Oncology Krakow Branch, Poland; Katarzyna Kotfis, Department of Anaesthesia, Intensive Care and Acute Poisonings, Pomeranian Medical University, Teaching Hospital No.2, Poland; Katarzyna Cwyl, ICU, RCZ in Lublin, Poland; Ryszard Gajdosz, Department of Anaesthesiology and Intensive Care, Scanmed St. Raphael Hospital in Kraków, Poland; Jowita Biernawska, Department of Anaesthesiology and Intensive Care, Pomeranian Medical University, Teaching Hospital No. 1, Poland; Romuald Bohatyrewicz, Department of Anaesthesiology and Intensive Care, Pomeranian Medical University, Teaching Hospital No. 1, Poland; Ryszard Gawda, Department of Anaesthesiology and Intensive Care, University Hospital in Opole, Poland; Paweł Grudzień, ICU, Edward Szczeklik Specialist Hospital in Tarnów, Poland; Paweł Nasiłowski, Department of Anaesthesiology and Intensive Care, Gabriel Narutowicz Specialist Hospital in Kraków, Poland; Natalia Popek, Department of Anaesthesiology and Intensive Care, Stefan Żeromski Specialist Hospital in Kraków, Poland; Waldemar Cyrankiewicz, Department of Anaesthesiology and Intensive Care, Antoni Jurasz University Hospital No. 1 in Bydgoszcz, Poland; Katarzyna Wawrzyniak, Department of Anaesthesiology and Intensive Care, Antoni Jurasz University Hospital No. 1 in Bydgoszcz, Poland; Marek Wnuk, Department of Anaesthesiology and Intensive Care, John Paul II Memorial Hospital in Bełchatów, Poland; Dariusz Maciejewski, Department of Anaesthesiology and Intensive Care, Provincial hospital in Bielsko-Biała, Poland; Dorota Studzińska, Department of Anaesthesiology and Intensive Care, St. John Grande Hospital, Poland; Maciej Żukowski, Department of Anaesthesiology, Intensive Care and Acute Poisoning, Pomeranian Medical University, Teaching Hospital No. 2 in Szczecin, Poland; Szymon Bernas, Department of Anaesthesiology and Intensive Therapy Centre for Artificial Extracorporeal Kidney and Liver Support, Dr Władysław Biegański Regional Specialist Hospital in Łódź, Poland; Mariusz Piechota, Department of Anaesthesiology and Intensive Therapy Centre for Artificial Extracorporeal Kidney and Liver Support, Dr Władysław Biegański Regional Specialist Hospital in Łódź, Poland; Centre for Artificial Extracorporeal Kidney and Liver Support, Poland; Wojciech Szczeklik, Department of Intensive Care and Perioperative Medicine, University Hospital in Kraków, Poland; Ilona Nowak, Department of Intensive Care and Perioperative Medicine, University Hospital in Kraków, Poland; Jakub Fronczek, Department of Intensive Care and Perioperative Medicine, University Hospital in Kraków, Poland; Marta Serwa, Department of Anaesthesiology and Intensive Care, University Hospital and Educational Centre of the Medical University of Łódź, Poland; Waldemar Machała, Department of Anaesthesiology and Intensive Care, University Hospital and Educational Centre of the Medical University of Łódź, Poland; Jan Stefaniak, Department of Anaesthesiology and Intensive Care, University Clinical Centre in Gdańsk, Poland; Maria Wujtewicz, Department of Anaesthesiology and Intensive Care, University Clinical Centre in Gdańsk, Poland; Paweł Maciejewski, Department of Anaesthesiology and Intensive Care, Orthopedic-Rehabilitation University Hospital in Zakopane, Poland; Małgorzata Szymkowiak, Department of Anaesthesiology and Intensive Care, Józef Struś Hospital in Poznan, Poland; Barbara Adamik, Department of Anaesthesiology and Intensive Care, Wrocław University Hospital, Poland; Nuno Catorze, UCIP, C. H. Médio TEJO, Portugal; Miguel Castelo Branco, Unidade de Cuidados Intensivos, Centro Hospitalar Cova da Beira, EPE, Portugal; Inês Barros, Unidade de Cuidados Intensivos Polivalente, Centro Hospitalar Tondela-Viseu, Portugal; Nelson Barros, Serviço Medicina Intensiva, Centro Hospitalar Trás-os-Montes e Alto Douro, Portugal; Andriy Krystopchuk, Intensive Care and Emergency Department, Centro Hospitalar do Algarve-Hospital de Faro, Portugal; Teresa Honrado, Unidade Cuidados INtensivos Polivalente, Hospital de São João, Portugal; Cristina Sousa, UCI, Hospital da Luz, Portugal; Francisco Munoz, UMI, Hospital do SAMS, Portugal; Marta Rebelo, UCIP, Hospital de Egas Moniz, Portugal; Rui Gomes, UCI, Hospital Garcia de Orta, Portugal; Jorge Nunes, Unidade de Cuidados Intensivos, Hospital Lusiadas Lisboa, Portugal; celeste dias, Neurocritical ICU, Hospital de São João, Portugal; Ana Margarida Fernandes, UCI Neurocríticos, Hospital S. José - CHLC EPE, Portugal; Cristina Petrisor, Anaesthesia and Intensive Care 1, Clinical Emergency County Hospital Cluj, Portugal; Bodolea Constantin, ATI, Municipal Hospital, Portugal; Vladislav Belskiy, Department of Anesthesiology and Intensive Care, Privolzhskiy District Medical Center, Russia; Boris Boskholov, Dept of intensive care, Zhadkevich Clinical Hospital, Russia; Enver Rodriguez, UCI , General Universitario de Castellón, Spain; Sergio Rebollo, ICU, HGU Santa Lucia,Cartagena, Murcia, Spain; Gerardo Aguilar, Unidad de Reanimación - Surgical ICU, Hospital Clínico Universitario de Valencia, Spain; Gaspar Masdeu, Servei Medicina Intensiva, Hospital de Tortosa Verge de la Cinta, Spain; Marián Irazábal Jaimes, Critical Care Unit, Hospital General de Catalunya, Spain; Ángela Prado Mira, Medicina Intensiva, Hospital General Universitario de Albacete, Spain; Maria A. Bodi, General ICU, Hospital Universitari de Tarragona Joan XXIII, Spain; Jesus A. Barea Mendoza, Servicio de Medicina Intensiva, Hospital Universitario 12 de Octubre, Spain; Sonia López-Cuenca, Servicio de Medicina Intensiva y Grandes Quemados, Hospital Universitario de Getafe, Spain; Marcela Homez Guzman, ICU, Hospital Universitario del Henares, Spain; Jesús Rico-Feijoo, Postoperative Critical Care Unit and Reanimation, Hospital Universitario Río Hortega de Valladolid, Spain; Mercedes Ibarz , ICU Hospital Universitario Sagrado Corazon, Hospital Universitario Sagrado Corazon. Barcelona, Spain; Josep Trenado Alvarez , Intensive Care Department. UCI-Semicritics, Hospital Universitario Mutua Terassa, Spain; Rafael Kawati, central ICU, Akademiska sjukhuset, Sweeden; Joakim Sivik, IVA Alingsås Lasarett, Alingsås Lasarett, Sweeden; Jessica Nauska, Intensivvårdsavdelning 31, Blekingesjukhuset Karlskrona, Sweeden; Daniel Smole, IVA, Centralsjukhuset i Karlstad, Sweeden; Fredric Parenmark, IVA, Gävle sjukhus, Sweeden; Johanna Lyrén, Intensivvårdsavdelning, Hudiksvalls sjukhus, Gävleborg, Hudiksvalls sjukhus, Sweeden; Katalin Rockstroh, IVA, Kalmar Länssjukhus, Sweeden; Sara Rydén, Karolinska ICU Huddinge, Karolinska University Hospital Huddinge, Sweeden; Martin Spångfors, Intensiven, Kristianstad, Sweeden; Morten Strinnholm, ICU Kungälvs Hospital, Kungälvs hospital, Sweeden; Sten Walther, Cardiothoracic ICU, Linköping University Hospital, Sweeden; Lina De Geer, ICU, Linköping University Hospital, Sweeden; Peter Nordlund, OP/IVA Kliniken, Länssjukhuset Ryhov, Sweeden; Staffan Pålsson, Intensivvårdsavdelningen, Norrtälje, Sweeden; Harald Zetterquist, IVA, Nykopings lasarett, Sweeden; Annika Nilsson, IVA, Ornskoldsvik, Ornskoldsviks hospital, Sweeden; Karin Thiringer, avdelning 227, IVA, Sahlgrenska University Hospital Mölndal, Sweeden; Mårten Jungner, ICU SUS Malmö, Skane University Hospital, Sweeden; Björn Bark, IVA Lund, Skåne University Hospital, Sweeden; Berit Nordling, IVA Sundsvall, Sundsvall, Sweeden; Hans Sköld, ICU, Torsby Sjukhus, Sweeden; Camilla Brorsson, CIP, University Hospital Northern Sweden, Sweeden; Stefan Persson, Intensivvårsdavdelningen USÖ, University hospital Örebro, Sweeden; Anna Bergström, IVA Vrinnevisjukhuset, Vrinnevi hospital, Sweeden; Johan Berkius, IVA Västervikssjukhus, Västervikssjukhus, Sweeden; Johanna Holmström, Intensivvårdsavdelningen Västerås, Västmanlands sjukhus, Västerås, Sweeden; I. van Dijk, Intensive Care , Alrijne Ziekenhuis, The Netherlands; L.E.M. van Lelyveld-Haas, Intensive Care, Diakonessenhuis Utrecht, The Netherlands; D.Ramnarain, Intensive Care, Elisabeth Tweesteden Hospital Tilburg, The Netherlands; Tim Jansen, Intensive Care , HagaZiekenhuis, The Netherlands; Fleur Nooteboom, IC LZR, Laurentius Ziekenhuis, The Netherlands; Peter HJ van der Voort, ICU OLVG, OLVG, The Netherlands; Dylan de Lange, Department of Intensive Care Medicine, UMC Utrecht, The Netherlands; Willem Dieperink, Department of Critical Care, University Medical Center Groningen, The Netherlands; Monique C. de Waard, Intensive Care Adults, VU University Medical Center Amsterdam, The Netherlands; Annemarie GE de Smet, Intensive Care Unit, University Medical Centre, University of Groningen, The Netherlands; Laura Bormans, Intensive Care, Zuyderland Medical Centrer, Heerlen, The Netherlands; Tom Dormans, Intensive Care, Zuyderland Medical Center, Heerlen, The Netherlands; Ged Dempsey, Critical Care Unit, Aintree University Hospital NHS Foundation Trust, UK; Shiju J Mathew, ICU, Alexandra Hospital, UK; Ashok S Raj, ICU, Barts Health NHS Trust, Whipps Cross Hospital, UK; Irina Grecu, ITU/HDU, Basingstoke and North Hampshire Hospital, UK; Jason Cupitt, Critical Care Unit, Blackpool Teaching Hospitals NHS Foundation Trust, UK; Tom Lawton, Critical Care Unit, Bradford Royal Infirmary, UK; Richard Clark, ICU, Central Manchester Foundation Trust, UK; Monica Popescu, ICU, Chelsea and Westminster Foundation Trust, West Middlesex University Hospital, UK; Nick Spittle, ICU, Chesterfield Royal Hospital, UK; Maria Faulkner, ICU, Countess of Chester Hospital NHS Foundation Trust, UK; Amanda Cowton, ICU, Darlington memorial Hospital (CDDFT), UK; Esme Elloway, ICU, Derriford Hospital, UK; Patricia Williams, Critical Care Unit, Dorset County Hospital, UK; Michael Reay, Critical Care Unit , Dudley Group of Hospitals NHSFT, Russells Hall Hospital, UK; Srikanth Chukkambotla, Critical Care Unit, East Lancashire Hospitals NHS Trust, UK; Ravi Kumar , CCU, East Surrey Hospital , UK; Nawaf Al-Subaie, ICU, Espsom and St Helier University Hospitals, UK; Linda Kent, Critical Care Unit, Fairfield General Hospital, UK; Tiina Tamm, ICU, Frimley Health, Wexham Park Hospital, UK; Istvan Kajtor, ICU, Frimley Park Hospital, UK; Karen Burns, ICU, Furness General, UK; Richard Pugh, Critical Care Unit, Glan Clwyd Hospital, UK; Marlies Ostermann, ICU, Guys and St Thomas Hospital, UK; Elisa Kam, ICU, Hillingdon Hospital, UK; Helen Bowyer, Critical Care Centre, Hinchingbrooke Healthcare NHS Trust, UK; Neil Smith, HICU 1&2, Hull Royal Infirmary, UK; Maie Templeton, Critical Care UNIT, Imperial College Healthcare NHS Trust, UK; Jeremy Henning, ICU2&3, James Cook Univeristy Hospital, UK; Kelly Goffin, ICU, James Paget University Hospital, UK; Ritoo Kapoor, K&C ITU, Kent and Canterbury Hospital, UK; Shondipon Laha, CrCU, Lancashire Teaching Hospitals NHS Foundation Trust, UK; Phil Chilton, Critical Care Unit, Leighton Hospital, UK; Waqas Khaliq, ITU/HDU, Lewisham and Greenwich NHS Trust, UK; Alison Crayford, ITU/HDU, Maidstone, UK; Samantha Coetzee, ICU, Medway NHS Foundation Trust, UK; Moira Tait, Adult ICU, Musgrove Park, UK; Wendy Stoker, ICU, Northumbria Specialist Emergency Care Hospital, UK; Marc Gimenez, ICU, Papworth Hospital NHS Foundation Trust, UK; Alan Pope, Critical Care Unit, Peterborough City Hospital, UK; Julie Camsooksai, Critical Care Unit , Poole Hospital NHS Trust, UK; David Pogson, Department of Critical Care, Queen Alexandra Hospital Portsmouth, UK; Kate Quigley, ICU, Queen Elizabeth Hospital, UK; Jenny Ritzema, Critical Care Department, Queen Elizabeth Hospital, Gateshead, UK; Anil Hormis, Critical Care Unit, Rotherham NHS Foundation Trust, UK; Carole Boulanger , ICU, Royal Devon and Exeter NHS Foundation Trust, UK; M. Balasubramaniam , ICU and HCU, Royal Bolton NHS hospital trust, UK; Luke Vamplew, Critical Care Unit, Royal Bournemouth Hospital, UK; Karen Burt, Critical Care Unit, Royal Cornwall Hospital NHS Trust, UK; Daniel Martin, ICU, Royal Free London NHS Foundation Trust, UK; Irina Grecu, ICU, Royal Hampshire County Hospital, UK; Jayne Craig, ICU, Royal Lancaster Infirmary, UK; John Prowle, Adult Critical Care Unit, Royal London Hospital, UK; Nanci Doyle, ICU, Royal Surrey County Hospital, UK; Jonathon Shelton , Ward 38 ICU, Royal Victoria Infirmary, UK; Carmen Scott, Ward 18 ICU, Royal Victoria Infirmary, UK; Phil Donnison, ICU, Salisbury District Hospital, UK; Sarah Shelton , ICU, Sherwood Forest Hospitals NHS Foundation Trust, UK; Christian Frey, ITU/HDU, South Tyneside District Hospital, UK; Christine Ryan, GICU, St Georges Hospital, UK; Dominic Spray, Cardiothoracic ICU, St Georges Hospital, UK; Christine Ryan, Acute Dependency Unit, St Georges Hospital NHS Trust London, UK; Veronica Barnes, Neuro ICU, St Georges University Hospital NHS Foundation Trust, UK; Kerry Barnes, ITU, st helier hospital, UK; Stephanie Ridgway, Critical Care Unit, NHS Foundation Trust, Tameside General Hospital, UK; Rajnish Saha, Critical Care Unit, The Princess Alexandra NHS Hospital, UK; Linda Kent, ICU, The Royal Oldham Hospital, UK; Thomas Clark, ICU, Torbay Hospital, UK; James Wood, ICU, Tunbridge Wells Hospital, UK; Clare Bolger, General Intensive Care, Univeristy Hospital Southampton NHS Foundation Trust, UK; Christopher Bassford, General Critical Care, University Hospital Coventry, UK; Amanda Cowton, ICU, University hospital of North Durham, UK; john lewandowski, Critical Care Unit, University Hospital of North Tees, UK; Xiaobei Zhao, ICU (Level 6), Watford General Hospital / West Hertfortshire NHS trust, UK; Sally Humphreys, Critical Care, West Suffolk NHS Foundation Trust, UK; Susan Dowling, Ward 4E Critical Care unit, Whiston, UK; Neil Richardson, ICU, William Harvey Hospital, Ashford, UK; Andrew Burtenshaw, Critical Care Unit, Worcestershire Royal Hospital, UK; Carl Stevenson, ICU, Wye Valley NHS Trust, UK; Danielle Wilcock, Critical Care Unit, York Teaching Hospital NHS Foundation Trust, UK; Yuiry Nalapko, Anaesthesia and Intensive Care, Lugansk State Medical University, Ukraine.
Author information
Authors and Affiliations
Consortia
Contributions
All listed authors have (1) made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; (2) drafted the article or revised it critically for important intellectual content; and (3) given final approval of the version submitted for publication.
Corresponding authors
Ethics declarations
Conflicts of interest
None of the authors have any conflict of interest related to this article.
Additional information
The VIP-LST collaborators are listed in the Acknowledgements and in the Electronic Supplementary Material.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Guidet, B., Flaatten, H., Boumendil, A. et al. Withholding or withdrawing of life-sustaining therapy in older adults (≥ 80 years) admitted to the intensive care unit. Intensive Care Med 44, 1027–1038 (2018). https://doi.org/10.1007/s00134-018-5196-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-018-5196-7