Abstract
Objective
Many patients admitted to the intensive care unit (ICU) have pre-existing or acquired neurological disorders which significantly affect their short-term and long-term outcomes. The ESICM NeuroIntensive Care Section convened an expert panel to establish a pragmatic approach to neurological examination (NE) of the critically ill patient.
Methods
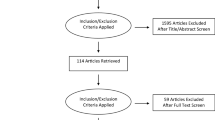
The group conducted a comprehensive review of published studies on the NE of patients with coma, delirium, seizures and neuromuscular weakness in critically ill patients. Quality of data was rated as high, moderate, low, or very low, and final recommendations as strong, weak, or best practice.
Summary and Conclusions
The group made the following recommendations: (1) NE should be performed in all patients admitted to ICUs; (2) NE should include an assessment of consciousness and cognition, brainstem function, and motor function; (3) sedation should be managed to maximize the clinical detection of neurological dysfunction, except in patients with reduced intracranial compliance in whom withdrawal of sedation may be deleterious; (4) the need for additional tests, including neurophysiological and neuroradiological investigations, should be guided by the NE; (5) selected features of the NE have prognostic value which should be considered in well-defined patient populations.
Similar content being viewed by others

Introduction
Clinical examination is the cornerstone of the assessment of patients with primary neurological conditions leading to intensive care unit (ICU) admission, and also for the detection of neurological disorders complicating critical illness. It is the basis for neuroanatomical localization of a disease process. It may help to identify a previously undiagnosed neurological disease, such as myasthenia gravis in a patient who is failing liberation from the ventilator, or pre-existing cognitive decline in a patient who develops delirium. The diagnosis of neurological disorders in the ICU may lead to therapeutic interventions, because a specific treatment is needed (e.g., the institution of anticonvulsant therapy) or contra-indicated (e.g., therapeutic anticoagulation in a patient with intracerebral hemorrhage), or to determine physiological goals (e.g., management of blood pressure in ischemic stroke). The identification of a neurological disorder will also orient prognosis and the need for and type of rehabilitation. Critical care providers need skills to (1) determine nature and severity of neurological dysfunction, (2) establish a neurological differential diagnosis, and (3) to determine a plan for further neurological testing and treatment. Currently, there are no recommendations for NE of critically ill patients. To address this gap, the ESICM NeuroIntensive Care Section (NIC) convened an expert panel of intensivists, neuro-intensivists, anesthesiologists, and neurologists to establish a pragmatic framework for the NE of critically ill adult patients.
Methods
Expert panel
The members of the expert panel were nominated at a meeting of the NIC in March 2010. Participants are senior academic intensivists with training in anesthesiology, critical care medicine, and neurology. The panel-members were asked to perform an evidence-based review and to write a concise summary with grading of the level of evidence and recommendations. These summaries were merged in a single manuscript which was then reviewed and edited by the entire panel.
Questions addressed by the panel
The group identified nine key domains relating to the clinical NE of critically ill patient and each panel member was tasked with responding in their summaries to one or two of the questions:
-
1.
What are the essential components of the clinical neurological assessment in the ICU?
-
2.
Which critically ill patients should be examined neurologically?
-
3.
How should sedation be managed to facilitate neurological assessment?
-
4.
How should coma be assessed in critically ill patients?
-
5.
How should delirium be assessed in critically ill patients?
-
6.
What are the clinical criteria which should prompt magnetic resonance imaging in patients who are admitted without primary neurological diagnosis?
-
7.
How should patients be evaluated for ICU-acquired muscle weakness?
-
8.
What are the clinical criteria which should prompt nerve conduction studies and electromyography?
-
9.
What is the prognostic value of neurological signs?
The place of EEG in the neurological assessment and monitoring of critically ill patients has been extensively addressed in a recent systematic review by Claassen et al. [1].
Search strategy
The PubMed database was searched (from 1996 to September 2012) for observational studies and clinical trials in adults using the following terms: “coma”, “delirium”, “confusion”, “agitation”, “consciousness”; “psychosis”, “encephalopathy”, “brain dysfunction”, “seizure”, “muscle weakness”; “paresis”, “critical illness polyneuropathy”, “critical illness myopathy”, “critical illness neuromyopathy”; with one of the following: “critical illness”, “critically ill patients”, “intensive care”, “sepsis”, “sedation”, “mechanical ventilation”. Only studies containing a description of the NE in critically ill populations were included. Review articles, animal studies, and studies conducted in pediatric populations were excluded.
Rating of evidence and recommendations
Quality of data and strength of final recommendations were rated high, moderate, low, or very low, and recommendations were rated as strong or weak. Some recommendations were based not on published evidence but on clinical standard of care acknowledged by all the experts. These were designated as “best practice recommendation”. All the recommendations were reviewed and approved by all members of the panel. In cases of disagreement, recommendations were modified, in order to be unanimously accepted. Therefore, all the members agreed with the content of the manuscript and the recommendations proposed here.
Question 1: what are the essential components of the clinical neurological assessment in the ICU?
Disturbances in neurological function are prevalent in the ICU, both as expressions of primary neurological injury and of systemic organ failure. Neurological signs indicate severity of illness and independently predict outcome [2–9]. Altered consciousness, delirium, agitation, anxiety, pain, sedation, neuromuscular blockade, hypothermia, intubation/mechanical ventilation, and surgical or traumatic lesions of the extremities may confound neurological assessment in the ICU [10]. Notwithstanding, NE is feasible in the ICU and has major diagnostic and prognostic significance [2, 11, 12].
The structure of the NE is determined by the level of consciousness:
-
(a)
In the conscious patient, the clinician assesses cognition (orientation, language, attention, memory), cranial nerves, motor and sensory function, reflexes, and coordination. The comprehensiveness and structure of this examination must be adapted to the underlying neurological process. Serial examinations are necessary to discern trends and evidence of deterioration. Once sedation is interrupted [13], delirium and coma should be scored using validated instruments [4, 14, 15], as detailed below. Muscular strength should be tested using the validated Medical Research Council (MRC) scale [6, 16] (Table 1).
Table 1 Medical Research Council (MRC) sumscore -
(b)
In the comatose patient, neurological assessment considers level of arousal, brainstem function, motor responses, and respiratory pattern [15]. Numerical scales generally used for this purpose are the Glasgow Coma Scale (GCS) [17] or The Full Outline of Unresponsiveness (FOUR) scale, as detailed in Table 2 and below [18] (see also Figs. 1, 2). In both traumatic and post-anoxic coma, brainstem semiology is critical: absence of pupillary reactivity and abnormal motor responses are prognostically significant [11, 19, 20], while loss of the corneal response signals poor outcome in post-anoxic coma [11].
Table 2 Glasgow Coma Scale and Full Outline of UnResponsiveness (FOUR) score Fig. 1
Recommendations
-
1.
Interpretation of neurological signs must consider confounding by sedation, neuromuscular blockade, pain, delirium, anxiety, metabolic and physiological disturbances, and the physical limitations caused by injuries and intubation—low evidence, best practice recommendation.
-
2.
Frequency of NE should be determined by the nature and severity of the underlying cause of neurological dysfunction. At a minimum, NE should be performed upon admission to the ICU and once daily—moderate evidence, best practice recommendation.
-
3.
Coma, delirium, and motor strength should be evaluated using validated scales (respectively GCS or FOUR; CAM-ICU or ICDSC; and MRC—moderate evidence, strong recommendation.
Question 2: which critically ill patients should be examined neurologically?
Neurological dysfunction including altered consciousness, delirium, seizures, and muscle weakness are exceedingly common in critically ill patients [21]. More than 80 % of mechanically ventilated patients may experience delirium in the ICU [22]. Depressed consciousness is the major contributor to prolonged ventilation in a third of those who need it and a significant factor in an additional 40 % [23, 24]. Neurological complications increase both the length of stay in hospital and the likelihood of death [23]. The mortality rate for patients with neurological complications is 55 % compared to 29 % for those without [25]. Critical illnesses have been associated with substantial long-term declines in neuropsychological function [26, 27, 28].
Recommendations
-
1.
All critically ill patients should undergo routine NE—moderate evidence, best practice recommendation.
Question 3: how should sedation be managed to facilitate neurological assessment?
In the ICU, routine interruption of continuous sedation (ICS) has been associated with reduced duration of mechanical ventilation and decreased overall ICU length of stay [29], and in the prevention and early treatment of evolving neurological deterioration [29, 30]. The strategy of ICS may allow a downward titration of sedative infusion rates over time, minimizing the tendency for accumulation [29, 31–34]. In one trial, paired sedation interruption and spontaneous breathing trials were linked to reduced 1-year mortality [33]. The strategy of daily ICS and neurological evaluation has been demonstrated as beneficial, but the role of more frequent evaluation needs further study [35]. Also, the relative benefits of ICS as opposed to protocolized sedation were not clearly demonstrated in one recent multicenter trial [30].
ICS may have adverse effects in patients with reduced intracranial compliance resulting in deleterious ICP and CPP changes [36, 37]. These patients, and also patients without ICP monitoring in whom low intracranial compliance is suspected, should be excluded from ICS and information should instead be gathered from other neuromonitoring methods in combination with neuroradiological evaluation. Recent evidence suggests that assessment of brainstem responses is feasible even when sedation is maintained, and that loss of selected responses is predictive of mortality and altered mental status [12].
Recommendations
-
1.
Daily interruption or reduction of sedation is recommended in mechanically ventilated patients to enhance NE and improve short- and long-term outcomes—moderate evidence, strong recommendation.
-
2.
Sedation interruption is not recommended in patients with intracranial hypertension—moderate evidence, strong recommendation.
Question 4: how should coma be assessed in critically ill patients?
Examination of the comatose patient should include assessment of the best responses to graded stimulus starting with verbal order and progressing to noxious stimulus, brainstem reflexes, motor responses, and respiratory pattern [15]. The noxious stimulus can evoke localizing movements, withdrawal, posturing reflexes, or no response. Brainstem examination includes an assessment of pupils and pupillary reactivity, spontaneous eye position and movements, vestibulo-oculocephalic reflex, corneal reflex, cough, and gag reflexes [12, 38].
There are various scales that assign a numerical value to the level of consciousness. The GCS remains the most widely used [17]. Its main limitations are that verbal responses are not assessable in mechanically ventilated patients and that brainstem examination is not directly considered. More recently, the FOUR score has been designed and validated for use in mechanically ventilated patients [18]. It assesses eye response, motor response, brainstem reflexes, and respiratory pattern and has been tested in a range of clinical settings and in different countries [39–42]. Patients with the lowest GCS score can be further differentiated using the FOUR score (Table 2); however, evidence that the FOUR has greater inter-rater reliability or prognostic value than the GCS is limited [18, 39].
Recommendations
-
1.
Examination of the comatose patient should include graded stimulus, brainstem evaluation, motor responses, and respiratory pattern—moderate evidence, best practice recommendation.
-
2.
Coma examination should include a validated objective scale such as the GCS or the FOUR score—moderate evidence, strong recommendation.
Question 5: how should delirium be assessed in critically ill patients?
Delirium is a pathological alteration in cerebral function associated with inattention, a fluctuating course, and an underlying illness or physiologic/metabolic imbalance [43]. Delirium is independently linked to hospital mortality and length of stay [7, 44, 45], posing a major public health burden [46, 47]. Delirium also increases the likelihood of post-discharge death [48], functional disability [49], cognitive impairment [26, 28], and dementia [50]. The risk of delirium is particularly high in the elderly, following major surgery [51] and in the ICU [14]. Up to 80 % of mechanically ventilated patients experience delirium, which is independently associated with a higher risk of death during and after hospitalization [14, 44, 48, 52].
Delirium is under-recognized and inadequately treated in ICU patients [53]. There is broad acceptance of the Diagnostic and Statistical Manual of mental disorders (DSM) criteria for delirium [43]; however, implementation of DSM in the ICU is hindered by sedation and endotracheal intubation. The Confusion Assessment Method for the Intensive care Unit (CAM-ICU) assesses four items (acute change of or fluctuating mental status, inattention, altered level of consciousness, and disorganized thinking), two of which require active patient participation [14]. The Intensive Care Delirium Screening Checklist (ICDSC) has eight items (level of consciousness, inattention, disorientation, hallucination/delusion/psychosis, psychomotor agitation or retardation, inappropriate speech or mood, sleep/wake disturbance, and fluctuation of symptoms), none of which require direct patient cooperation [4]. The feasibility of CAM-ICU and ICDSC screening has been demonstrated in different ICU settings and in many countries [52, 54–57]. The validity and reliability of the two instruments when compared to a diagnostic gold standard (DSM) is mixed [4, 14, 56], as is their comparative accuracy [13, 58, 59]. Delirium screening is not practicable in the unconscious patient, and the value of delirium screening in sedated patients needs further study.
Recommendations
-
1.
All critically ill patients who are not comatose should be screened routinely for the presence of delirium—high evidence, strong recommendation.
-
2.
Delirium should be assessed using a score validated in the ICU, such as the CAM-ICU or the ICDSC—moderate evidence, strong recommendation.
-
3.
Delirium screening should be repeated at scheduled intervals to increase diagnostic sensitivity and monitor response to interventions—low evidence, strong recommendation.
Question 6: what are the clinical criteria which should prompt neuroimaging in patients who are admitted without a primary neurological diagnosis?
Neuroimaging with computed tomography (CT) may reveal brain infarction, intracranial hemorrhage, or cerebral edema, and is generally the first neuroimaging study in patients where clinical instability or local resource limitation makes magnetic resonance imaging (MRI) inaccessible. In the same sitting, CT may be coupled with (1) CT angiography which may be useful in the diagnosis of intracranial aneurysms, vasospasm, arterial occlusion, stenosis or dissection, and cerebral venous thrombosis, and (2) CT perfusion to evaluate regional cerebral blood flow abnormalities.
Brain MRI has greater sensitivity to early infarction and is substantially superior to CT in identifying lesions in the posterior fossa. Brain MRI may have prognostic value in patients with hypoxic-ischemic [60] or septic [61] encephalopathy. Imaging findings are not diagnostic in isolation; consequently, the prescription of neuroimaging studies is recommended only once clinical history and NE define a reasonably high a priori probability of brain injury.
Recommendations
-
1.
Computed tomography (CT) is a reasonable initial imaging modality for the evaluation of patients with focal neurological deficits or unexplained depression of consciousness, particularly when the need for continuing organ support and/or local resource limitation makes MR logistically difficult—high evidence, best practice recommendation.
-
2.
Brain MRI is recommended in the following conditions:
-
(a)
In patients developing acute neurological deficits or an acute change in mental status not explained by CT-scan—high evidence, strong recommendation;
-
(b)
In patients with refractory status epilepticus, who cannot be evaluated clinically due to the concurrent use of major neurodepressants—high evidence, best practice recommendation;
-
(c)
In case of suspicion of cerebral fat embolism, osmotic myelinolysis, or posterior reversible encephalopathy syndrome—high evidence, best practice recommendation;
-
(d)
In patients not recovering after hypoxic-ischemic injury or prolonged hypoglycaemia—high evidence, best practice recommendation;
-
(e)
In patients with sepsis associated with altered mental status, focal neurological signs, and/or abnormal brainstem reflexes—low evidence, best practice recommendation.
-
(a)
Question 7: how should patients be evaluated for ICU-acquired muscle weakness?
ICU-acquired muscle weakness (ICUAW) is a generalized symmetrical reduction of limb and respiratory muscle strength developing as a complication of critical illness [62]. Manual testing of muscle strength is done using the Medical Research Council [16] (Table 1), or handgrip dynamometry [2] in awake collaborative patients. Critical illness polyneuropathy (CIP) and myopathy (CIM) are the most frequent cause of ICUAW. ICUAW should be differentiated on the basis of clinical history and NE. Differential diagnosis includes concurrent complications, such as electrolyte abnormalities, rhabdomyolysis, nerve compression or entrapment, status epilepticus, surgery, or use of drugs, and pre-existing neuromuscular diseases, particularly in cases of acute onset diseases (Guillain–Barré syndrome, myasthenia gravis, botulin intoxication, hypokalemic periodic paralysis, and various intoxications) [62] (Tables 3, 4).
ICUAW is usually excluded in the presence of the following: clinical signs suggest a central nervous system disease (i.e. Babinski signs, increased deep tendon reflexes, spasticity, widespread muscle fasciculation, and focal neurological signs); facial muscles are involved (i.e. drooping of the eyelids, weakness of extraocular muscles with diplopia, facial nerve palsy with altered patient’s expression, and difficulty in speech, chewing or swallowing); distribution of muscle weakness is asymmetrical (i.e. monoparesis or hemiparesis); progression of muscle weakness suggests a specific diagnosis, for example, the pattern is ascending (Guillain–Barré syndrome) or descending (botulin intoxication); muscle weakness is fluctuating and worsens after brief exercise indicating muscle fatigability and neuromuscular transmission defect (myasthenia gravis) or improves after exercise indicating pre-synaptic neuromuscular defect (Lambert–Eaton syndrome); there are associated abnormalities such as skin rash or abdominal pain pointing to dermatomyositis, vasculitis, porphyria, or diabetes; there are dysautonomic signs (i.e. dilated pupils poorly reactive to light suggesting botulin intoxication, and cardiac arrhythmias or fluctuations in blood pressure as seen in GBS); pharmacological side effects are suspected (i.e. after prolonged administration of neuromuscular blocking agents, steroids, or cancer chemotherapy).
Recommendations
-
1.
We recommend that assessment of ICUAW be made using either the MRC or handgrip dynamometry—low evidence, moderate recommendation
-
2.
Critically ill patients with muscle weakness should be evaluated for plausible etiologies with a careful clinical history and NE—moderate evidence, best practice recommendation.
Question 8: what are the clinical criteria, which should prompt nerve conduction studies and electromyography?
Nerve conduction studies (NCS) include the measurement of conduction velocity and action potential amplitude in sensory (SNAP) and motor (CMAP) nerves [63]. SNAP and CMAP amplitudes are reduced while nerve conduction velocity is normal in sensory-motor axonal neuropathy such as CIP [64]. Conversely, velocity is reduced while amplitude is normal in demyelinating polyneuropathy. In repetitive muscle stimulation, a brief series of stimulations is applied to a motor nerve, and serial response amplitudes are recorded [63]; a decremented response is shown in disorders of the neuromuscular transmission such as myasthenia gravis or the use of neuromuscular blocking agents.
ICU-AW is established clinically. However, clinical evaluation has limitations particularly in cases of rapid progression of disease causing acute respiratory failure. Some diseases are amenable to specific treatments, for example, immunoglobulins or plasmapheresis in Guillain–Barré syndrome [65], steroids in post-surgical inflammatory neuropathy [66], antitoxin administration in botulism [67], or simply the prompt removal of ticks in tick paralysis [68]. Nerve conduction study, repetitive nerve stimulation, and electromyography can be of value in distinguishing acute axonal neuropathy from demyelinating neuropathy, altered neuromuscular transmission, or acute myopathy.
Recommendations
-
1.
We recommend that NCS and EMG are used whenever a differential diagnosis between ICUAW and other causes of neuromuscular weakness cannot be achieved based on history and clinical features—moderate evidence, best practice recommendation.
Question 9: what is the prognostic value of neurological signs?
Clinical examination is the cornerstone for prognostic assessment following neurological insults [69]. In traumatic brain injury (TBI), the GCS and pupillary light responses have prognostic significance [70, 71]. Following cardiac arrest (CA), absent pupillary light response, corneal reflexes, abnormal motor response, and the presence of myoclonus status epilepticus have been robustly associated with neurologic prognosis in patients who have not received therapeutic hypothermia [72, 73]. In CA patients who have received therapeutic hypothermia, clinically significant false positive rates have been noted in particular with absent or abnormal with motor responses [19, 74, 75]. The clinical NE also has prognostic significance in non-neurological critical illness, increased weighting of the GCS increases prognostic performance of APACHE II [76], and APACHE III [3]. The FOUR score has prognostic value in a range of illnesses [19, 40, 41, 74]. Impaired brainstem responses, absent verbal responses, or absent withdrawal to pain substantially increase the risk of non-survival or severe disability in comatose critically ill patients [12, 77]. Absent cough or oculocephalic reflexes, even when documented in sedated patients, remain predictive of mortality and post-sedation delirium [12]. Finally, delirium independently predicts mortality and long-term risk of neuropsychological impairment in critically ill patients [7, 26].
Recommendations
-
1.
NE is recommended to assess prognosis following TBI and CA—high evidence, strong recommendation.
-
2.
NE of comatose patients after CA should include: pupillary reflex, corneal reflex, and motor responses—high evidence, strong recommendation.
Concluding remarks
These deliberations of this panel provide pragmatic recommendations on the indications, content, and interpretation of NE, and on the indication for additional testing in order to improve the management of critically ill patients who have, or are at high risk for developing, neurological disorders. A major contribution of the present work is to underscore the need to conduct studies which will define and validate the neurological approach to critically ill patients. Despite technological advances, it is likely that the clinical NE will remain a foundation in the assessment of patients in the ICU.
Limitations of this work must be acknowledged. First, the evidence supporting some of these recommendations is weak or biased. Second, and largely because of the lack of robust studies, this group elected to not undertake a formal evidence-based consensus process. Finally, we have focused our investigation on two major neurological syndromes—alteration of consciousness (i.e. delirium and coma) and muscle weakness—as they are the most frequent neurological manifestations of critical illness. It will be interesting in the future to address other more subtle neurological symptoms such as impairments in attention, memory, and executive function.
References
Claassen J, Taccone FS, Horn P, Holtkamp M, Stocchetti N, Oddo M (2013) Recommendations on the use of EEG monitoring in critically ill patients: consensus statement from the neurointensive care section of the ESICM. Intensive Care Med. doi:10.1007/s00134-013-2938-4
Ali NA, O’Brien JM Jr, Hoffmann SP, Phillips G, Garland A, Finley JC, Almoosa K, Hejal R, Wolf KM, Lemeshow S, Connors AF Jr, Marsh CB (2008) Acquired weakness, handgrip strength, and mortality in critically ill patients. Am J Respir Crit Care Med 178:261–268
Bastos PG, Sun X, Wagner DP, Wu AW, Knaus WA (1993) Glasgow Coma Scale score in the evaluation of outcome in the intensive care unit: findings from the Acute Physiology and Chronic Health Evaluation III study. Crit Care Med 21:1459–1465
Bergeron N, Dubois MJ, Dumont M, Dial S, Skrobik Y (2001) Intensive care delirium screening checklist: evaluation of a new screening tool. Intensive Care Med 27:859–864
De Jonghe B, Bastuji-Garin S, Durand MC, Malissin I, Rodrigues P, Cerf C, Outin H, Sharshar T (2007) Respiratory weakness is associated with limb weakness and delayed weaning in critical illness. Crit Care Med 35:2007–2015
De Jonghe B, Sharshar T, Lefaucheur JP, Authier FJ, Durand-Zaleski I, Boussarsar M, Cerf C, Renaud E, Mesrati F, Carlet J, Raphael JC, Outin H, Bastuji-Garin S (2002) Paresis acquired in the intensive care unit: a prospective multicenter study. JAMA 288:2859–2867
Ely EW, Shintani A, Truman B, Speroff T, Gordon SM, Harrell FE Jr, Inouye SK, Bernard GR, Dittus RS (2004) Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA 291:1753–1762
Oddo M, Carrera E, Claassen J, Mayer SA, Hirsch LJ (2009) Continuous electroencephalography in the medical intensive care unit. Crit Care Med 37:2051–2056
Sharshar T, Bastuji-Garin S, Stevens RD, Durand MC, Malissin I, Rodriguez P, Cerf C, Outin H, De Jonghe B (2009) Presence and severity of intensive care unit-acquired paresis at time of awakening are associated with increased intensive care unit and hospital mortality. Crit Care Med 37:3047–3053
Samaniego EA, Mlynash M, Caulfield AF, Eyngorn I, Wijman CA (2011) Sedation confounds outcome prediction in cardiac arrest survivors treated with hypothermia. Neurocrit Care 15:113–119
Levy DE, Bates D, Caronna JJ, Cartlidge NE, Knill-Jones RP, Lapinski RH, Singer BH, Shaw DA, Plum F (1981) Prognosis in nontraumatic coma. Ann Intern Med 94:293–301
Sharshar T, Porcher R, Siami S, Rohaut B, Bailly-Salin J, Hopkinson NS, Clair B, Guidoux C, Iacobone E, Sonneville R, Polito A, Aboab J, Gaudry S, Morla O, Amouyal G, Azuar J, Allary J, Vieillard-Baron A, Wolff M, Cariou A, Annane D (2011) Brainstem responses can predict death and delirium in sedated patients in intensive care unit. Crit Care Med 39:1960–1967
Haenggi M, Blum S, Brechbuehl R, Brunello A, Jakob S, Takala J (2013) Effect of sedation level on the prevalence of delirium when assessed with CAM-ICU and ICDSC. Intensive Care Med 39:2171–2179
Ely EW, Inouye SK, Bernard GR, Gordon S, Francis J, May L, Truman B, Speroff T, Gautam S, Margolin R, Hart RP, Dittus R (2001) Delirium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU). JAMA 286:2703–2710
Plum F, Posner JB (1981) The diagnosis of stupor and coma. Oford University Press, New York, pp 394–447
Kleyweg RP, van der Meche FG, Schmitz PI (1991) Interobserver agreement in the assessment of muscle strength and functional abilities in Guillain–Barre syndrome. Muscle Nerve 14:1103–1109
Teasdale G, Jennett B (1974) Assessment of coma and impaired consciousness. A practical scale. Lancet 2:81–84
Wijdicks EF, Bamlet WR, Maramattom BV, Manno EM, McClelland RL (2005) Validation of a new coma scale: the FOUR score. Ann Neurol 58:585–593
Bouwes A, Binnekade JM, Kuiper MA, Bosch FH, Zandstra DF, Toornvliet AC, Biemond HS, Kors BM, Koelman JH, Verbeek MM, Weinstein HC, Hijdra A, Horn J (2012) Prognosis of coma after therapeutic hypothermia: a prospective cohort study. Ann Neurol 71:206–212
Kamps MJ, Horn J, Oddo M, Fugate JE, Storm C, Cronberg T, Wijman CA, Wu O, Binnekade JM, Hoedemaekers CW (2013) Prognostication of neurologic outcome in cardiac arrest patients after mild therapeutic hypothermia: a meta-analysis of the current literature. Intensive Care Med 39:1671–1682
Bleck TP, Smith MC, Pierre-Louis SJ, Jares JJ, Murray J, Hansen CA (1993) Neurologic complications of critical medical illnesses. Crit Care Med 21:98–103
Razvi SS, Bone I (2003) Neurological consultations in the medical intensive care unit. J Neurol Neurosurg Psychiatry 74(Suppl 3):iii16–iii23
Vosylius S, Sipylaite J, Ivaskevicius J (2005) Determinants of outcome in elderly patients admitted to the intensive care unit. Age Ageing 34:157–162
Shehabi Y, Chan L, Kadiman S, Alias A, Ismail WN, Tan MA, Khoo TM, Ali SB, Saman MA, Shaltut A, Tan CC, Yong CY, Bailey M, Sedation Practice in Intensive Care (SPICE) E, Study Group investigators (2013) Sedation depth and long-term mortality in mechanically ventilated critically ill adults: a prospective longitudinal multicentre cohort study. Intensive Care Med 39:910–918
Leijten FS, Harinck-de Weerd JE, Poortvliet DC, de Weerd AW (1995) The role of polyneuropathy in motor convalescence after prolonged mechanical ventilation. JAMA 274:1221–1225
Girard TD, Jackson JC, Pandharipande PP, Pun BT, Thompson JL, Shintani AK, Gordon SM, Canonico AE, Dittus RS, Bernard GR, Ely EW (2010) Delirium as a predictor of long-term cognitive impairment in survivors of critical illness. Crit Care Med 38:1513–1520
Iwashyna TJ, Ely EW, Smith DM, Langa KM (2010) Long-term cognitive impairment and functional disability among survivors of severe sepsis. JAMA 304:1787–1794
Pandharipande PP, Girard TD, Jackson JC, Morandi A, Thompson JL, Pun BT, Brummel NE, Hughes CG, Vasilevskis EE, Shintani AK, Moons KG, Geevarghese S, Canonico A, Hopkins RO, Bernard GR, Dittus RS, Ely EW, BRAIN-ICU Study Investigators (2013) Long-term cognitive impairment after critical illness. N Engl J Med 369:1306–1316
Kress JP, Pohlman AS, O’Connor MF, Hall JB (2000) Daily interruption of sedative infusions in critically ill patients undergoing mechanical ventilation. N Engl J Med 342:1471–1477
Mehta S, Burry L, Cook D, Fergusson D, Steinberg M, Granton J, Herridge M, Ferguson N, Devlin J, Tanios M, Dodek P, Fowler R, Burns K, Jacka M, Olafson K, Skrobik Y, Hebert P, Sabri E, Meade M, Investigators S, Canadian Critical Care Trials G (2012) Daily sedation interruption in mechanically ventilated critically ill patients cared for with a sedation protocol: a randomized controlled trial. JAMA 308:1985–1992
Barr J, Fraser GL, Puntillo K, Ely EW, Gelinas C, Dasta JF, Davidson JE, Devlin JW, Kress JP, Joffe AM, Coursin DB, Herr DL, Tung A, Robinson BR, Fontaine DK, Ramsay MA, Riker RR, Sessler CN, Pun B, Skrobik Y, Jaeschke R (2013) Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med 41:263–306
Ely EW, Baker AM, Dunagan DP, Burke HL, Smith AC, Kelly PT, Johnson MM, Browder RW, Bowton DL, Haponik EF (1996) Effect on the duration of mechanical ventilation of identifying patients capable of breathing spontaneously. N Engl J Med 335:1864–1869
Girard TD, Kress JP, Fuchs BD, Thomason JW, Schweickert WD, Pun BT, Taichman DB, Dunn JG, Pohlman AS, Kinniry PA, Jackson JC, Canonico AE, Light RW, Shintani AK, Thompson JL, Gordon SM, Hall JB, Dittus RS, Bernard GR, Ely EW (2008) Efficacy and safety of a paired sedation and ventilator weaning protocol for mechanically ventilated patients in intensive care (Awakening and Breathing Controlled trial): a randomised controlled trial. Lancet 371:126–134
Strom T, Martinussen T, Toft P (2010) A protocol of no sedation for critically ill patients receiving mechanical ventilation: a randomised trial. Lancet 375:475–480
Citerio G, Cormio M (2003) Sedation in neurointensive care: advances in understanding and practice. Curr Opin Crit Care 9:120–126
Skoglund K, Enblad P, Marklund N (2009) Effects of the neurological wake-up test on intracranial pressure and cerebral perfusion pressure in brain-injured patients. Neurocrit Care 11:135–142
Helbok R, Kurtz P, Schmidt MJ, Fernandez L, Connolly SE, Lee K, Schmutzhard E, Mayer SA, Claassen J, Badjatia N (2012) Effects of the neurological wake-up test on clinical examination, intracranial pressure, brain metabolism and brain tissue oxygenation in severely brain-injured patients. Crit Care 16:R226
Stevens RD, Bhardwaj A (2006) Approach to the comatose patient. Crit Care Med 34:31–41
Fischer M, Ruegg S, Czaplinski A, Strohmeier M, Lehmann A, Tschan F, Hunziker PR, Marsch SC (2010) Inter-rater reliability of the Full Outline of UnResponsiveness score and the Glasgow Coma Scale in critically ill patients: a prospective observational study. Crit Care 14:R64
Iyer VN, Mandrekar JN, Danielson RD, Zubkov AY, Elmer JL, Wijdicks EF (2009) Validity of the FOUR score coma scale in the medical intensive care unit. Mayo Clin Proc 84:694–701
Stead LG, Wijdicks EF, Bhagra A, Kashyap R, Bellolio MF, Nash DL, Enduri S, Schears R, William B (2009) Validation of a new coma scale, the FOUR score, in the emergency department. Neurocrit Care 10:50–54
Weiss N, Mutlu G, Essardy F, Nacabal C, Sauves C, Bally C, Houbert M, Lecorre C, Germack V, Demeret S, Pierrot-Deseilligny C, Bolgert F (2009) The French version of the FOUR score: a new coma score. Rev Neurol (Paris) 165:796–802
American Psychiatric Association (2000) Task Force on DSM-IV. Diagnostic and statistical manual of mental disorders: DSM-IV-TR. American Psychiatry Association, Washington, DC
Lin SM, Liu CY, Wang CH, Lin HC, Huang CD, Huang PY, Fang YF, Shieh MH, Kuo HP (2004) The impact of delirium on the survival of mechanically ventilated patients. Crit Care Med 32:2254–2259
Pompei P, Foreman M, Rudberg MA, Inouye SK, Braund V, Cassel CK (1994) Delirium in hospitalized older persons: outcomes and predictors. J Am Geriatr Soc 42:809–815
Lemyze M, Mallat J, Nigeon O, Barrailler S, Pepy F, Gasan G, Vangrunderbeeck N, Grosset P, Tronchon L, Thevenin D (2013) Rescue therapy by switching to total face mask after failure of face mask-delivered noninvasive ventilation in do-not-intubate patients in acute respiratory failure. Crit Care Med 41:481–488
Milbrandt EB, Deppen S, Harrison PL, Shintani AK, Speroff T, Stiles RA, Truman B, Bernard GR, Dittus RS, Ely EW (2004) Costs associated with delirium in mechanically ventilated patients. Crit Care Med 32:955–962
Pisani MA, Kong SY, Kasl SV, Murphy TE, Araujo KL, Van Ness PH (2009) Days of delirium are associated with 1-year mortality in an older intensive care unit population. Am J Respir Crit Care Med 180:1092–1097
O’Keeffe S, Lavan J (1997) The prognostic significance of delirium in older hospital patients. J Am Geriatr Soc 45:174–178
Witlox J, Eurelings LS, de Jonghe JF, Kalisvaart KJ, Eikelenboom P, van Gool WA (2010) Delirium in elderly patients and the risk of postdischarge mortality, institutionalization, and dementia: a meta-analysis. JAMA 304:443–451
Balas MC, Happ MB, Yang W, Chelluri L, Richmond T (2009) Outcomes associated with delirium in older patients in surgical ICUs. Chest 135:18–25
Salluh JI, Soares M, Teles JM, Ceraso D, Raimondi N, Nava VS, Blasquez P, Ugarte S, Ibanez-Guzman C, Centeno JV, Laca M, Grecco G, Jimenez E, Arias-Rivera S, Duenas C, Rocha MG (2010) Delirium epidemiology in critical care (DECCA): an international study. Crit Care 14:R210
Spronk PE, Riekerk B, Hofhuis J, Rommes JH (2009) Occurrence of delirium is severely underestimated in the ICU during daily care. Intensive Care Med 35:1276–1280
Devlin JW, Fong JJ, Schumaker G, O’Connor H, Ruthazer R, Garpestad E (2007) Use of a validated delirium assessment tool improves the ability of physicians to identify delirium in medical intensive care unit patients. Crit Care Med 35:2721–2724 (quiz 2725)
George C, Nair JS, Ebenezer JA, Gangadharan A, Christudas A, Gnanaseelan LK, Jacob KS (2011) Validation of the Intensive Care Delirium Screening Checklist in nonintubated intensive care unit patients in a resource-poor medical intensive care setting in South India. J Crit Care 26:138–143
van Eijk MM, van den Boogaard M, van Marum RJ, Benner P, Eikelenboom P, Honing ML, van der Hoven B, Horn J, Izaks GJ, Kalf A, Karakus A, Klijn IA, Kuiper MA, de Leeuw FE, de Man T, van der Mast RC, Osse RJ, de Rooij SE, Spronk PE, van der Voort PH, van Gool WA, Slooter AJ (2011) Routine use of the confusion assessment method for the intensive care unit: a multicenter study. Am J Respir Crit Care Med 184:340–344
Radtke FM, Heymann A, Franck M, Maechler F, Drews T, Luetz A, Nachtigall I, Wernecke KD, Spies CD (2012) How to implement monitoring tools for sedation, pain and delirium in the intensive care unit: an experimental cohort study. Intensive Care Med 38:1974–1981
Fagundes JA, Tomasi CD, Giombelli VR, Alves SC, de Macedo RC, Topanotti MF, de Lourdes Ugioni Bristot M, do Brasil PE, Soares M, Salluh J, Dal-Pizzol F, Ritter C (2012) CAM-ICU and ICDSC agreement in medical and surgical ICU patients is influenced by disease severity. PLoS ONE 7: e51010
Plaschke K, von Haken R, Scholz M, Engelhardt R, Brobeil A, Martin E, Weigand MA (2008) Comparison of the confusion assessment method for the intensive care unit (CAM-ICU) with the Intensive Care Delirium Screening Checklist (ICDSC) for delirium in critical care patients gives high agreement rate(s). Intensive Care Med 34:431–436
Wijman CA, Mlynash M, Caulfield AF, Hsia AW, Eyngorn I, Bammer R, Fischbein N, Albers GW, Moseley M (2009) Prognostic value of brain diffusion-weighted imaging after cardiac arrest. Ann Neurol 65:394–402
Sharshar T, Carlier R, Bernard F, Guidoux C, Brouland JP, Nardi O, de la Grandmaison GL, Aboab J, Gray F, Menon D, Annane D (2007) Brain lesions in septic shock: a magnetic resonance imaging study. Intensive Care Med 33:798–806
Latronico N, Bolton CF (2011) Critical illness polyneuropathy and myopathy: a major cause of muscle weakness and paralysis. Lancet Neurol 10:931–941
Daube JR (1991) AAEM minimonograph #11: needle examination in clinical electromyography. Muscle Nerve 14:685–700
Latronico N, Shehu I, Guarneri B (2009) Use of electrophysiologic testing. Crit Care Med 37:S316–S320
Winer JB (2008) Guillain–Barre syndrome. BMJ 337:a671
Staff NP, Engelstad J, Klein CJ, Amrami KK, Spinner RJ, Dyck PJ, Warner MA, Warner ME (2010) Post-surgical inflammatory neuropathy. Brain 133:2866–2880
Sheridana EA, Cepeda J, De Palma R, Brett MM, Nagendran K (2004) A drug user with a sore throat. Lancet 364:1286
Felz MW, Smith CD, Swift TR (2000) A six-year-old girl with tick paralysis. N Engl J Med 342:90–94
Stevens RD, Sutter R (2013) Prognosis in severe brain injury. Crit Care Med 41:1104–1123
Perel P, Arango M, Clayton T, Edwards P, Komolafe E, Poccock S, Roberts I, Shakur H, Steyerberg E, Yutthakasemsunt S (2008) Predicting outcome after traumatic brain injury: practical prognostic models based on large cohort of international patients. BMJ 336:425–429
Steyerberg EW, Mushkudiani N, Perel P, Butcher I, Lu J, McHugh GS, Murray GD, Marmarou A, Roberts I, Habbema JD, Maas AI (2008) Predicting outcome after traumatic brain injury: development and international validation of prognostic scores based on admission characteristics. PLoS Med 5:e165 (discussion e165)
Wijdicks EF, Hijdra A, Young GB, Bassetti CL, Wiebe S, Quality Standards Subcommittee of the American Academy of N (2006) Practice parameter: prediction of outcome in comatose survivors after cardiopulmonary resuscitation (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 67:203–210
Sandroni C, Cavallaro F, Callaway CW, Sanna T, D’Arrigo S, Kuiper M, Della Marca G, Nolan JP (2013) Predictors of poor neurological outcome in adult comatose survivors of cardiac arrest: a systematic review and meta-analysis. Part 1: patients not treated with therapeutic hypothermia. Resuscitation 84:1310–1323
Rossetti AO, Oddo M, Logroscino G, Kaplan PW (2010) Prognostication after cardiac arrest and hypothermia: a prospective study. Ann Neurol 67:301–307
Sandroni C, Cavallaro F, Callaway CW, Sanna T, D’Arrigo S, Kuiper M, Della Marca G, Nolan JP (2013) Predictors of poor neurological outcome in adult comatose survivors of cardiac arrest: a systematic review and meta-analysis. Part 2: patients treated with therapeutic hypothermia. Resuscitation 84:1324–1338
Knaus WA, Draper EA, Wagner DP, Zimmerman JE (1985) APACHE II: a severity of disease classification system. Crit Care Med 13:818–829
Hamel MB, Phillips R, Teno J, Davis RB, Goldman L, Lynn J, Desbiens N, Connors AF Jr, Tsevat J (2002) Cost effectiveness of aggressive care for patients with nontraumatic coma. Crit Care Med 30:1191–1196
Stevens RD et al (2009) A framework for diagnosing and classifying intensive care unit-acquired weakness. Crit Care Med 37(Suppl 10):S299–S308
Conflicts of interest
The authors have no conflict of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Additional information
This document has been endorsed by the European Society of Intensive Care Medicine.
Rights and permissions
About this article
Cite this article
Sharshar, T., Citerio, G., Andrews, P.J.D. et al. Neurological examination of critically ill patients: a pragmatic approach. Report of an ESICM expert panel. Intensive Care Med 40, 484–495 (2014). https://doi.org/10.1007/s00134-014-3214-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-014-3214-y