Abstract
Background
Competence in airway management and maintenance of oxygenation and ventilation represent fundamental skills in emergency medicine. The successful use of laryngeal tubes (LT, LT-D, LTS II) to secure the airway in the prehospital setting has been published in the past. However, some complications can be associated with the use of a laryngeal tube.
Methods
In a nonconsecutive case series, problems and complications associated with the use of the laryngeal tube in prehospital emergency medicine as seen by independent observers in the emergency room are presented.
Results
Various problems and possible complications associated with the use of a laryngeal tube in eight case reports are reported: incorrect placement of the laryngeal tube in the trachea, displacement and/or incorrect placement of the laryngeal tube in the pharynx, tongue and pharyngeal swelling with subsequently difficult laryngoscopy, and inadequate ventilation due to unrecognized airway obstruction and tension pneumothorax.
Conclusion
Although the laryngeal tube is considered to be an effective, safe, and rapidly appropriable supraglottic airway device, it is also associated with adverse effects. In order to prevent tongue swelling, after initial prehospital or in-hospital placement of laryngeal tube and cuff inflation, it is important to adjust and monitor the cuff pressure.
Article in English.
Zusammenfassung
Hintergrund
Die sichere Beherrschung des Atemwegsmanagements sowie die Aufrechterhaltung einer Oxygenierung und Ventilation sind fundamentale Fähigkeiten in der Notfallmedizin. Im prähospitalen Setting wurde die erfolgreiche Anwendung von Larynxtuben (LT, LT-D und LTS II) zur Atemwegssicherung wiederholt publiziert. Jedoch können auch Komplikationen bei der Anwendung des Larynxtubus auftreten.
Methode
In einer nichtkonsekutiven Fallserie werden die mit der Anwendung des Larynxtubus assoziierten Probleme und Komplikationen durch unabhängige Beobachter aus der Notaufnahme berichtet.
Ergebnisse
Es wird von folgenden Problemen und Komplikationen berichtet, die bei Anwendung des Larynxtubus in 8 Fällen auftraten: nichtkorrekte Platzierung des Larynxtubus in der Trachea, Verrutschen bzw. nichtkorrekte Platzierung des Larynxtubus im Pharynx, Zungen- und Pharynxschwellung mit nachfolgender schwieriger Laryngoskopie, inadäquate Ventilation durch unerkannte Atemwegsobstruktion und Spannungspneumothorax.
Schlussfolgerung
Obwohl der Larynxtubus als effektive, sicher und rasch anwendbare supraglottische Atemwegshilfe angesehen wird, können schwere Nebenwirkungen eintreten. Um eine Zungenschwellung nach prä- oder innerklinischer Einlage eines Larynxtubus zu verhindern, sollte der „Cuff“-Druck gemessen und angepasst werden.
Similar content being viewed by others
Securing the airway and maintaining oxygenation and ventilation represent essential life-saving strategies in emergency medicine [1, 2, 3, 40]. Depending on the experience of the person performing the procedure and on the individual intubation conditions, endotracheal intubation (ETI) is still considered to be the gold standard [4, 5, 40].
Failed prehospital ETI is a common occurrence and associated with increased mortality. Reliable airway devices such as supraglottic airways (SGA) are needed for rescuers who are less experienced in ETI [2, 3, 40]. The different types of laryngeal mask airway (LMA) and the laryngeal tube have been reported as acceptable alternative devices [6, 7, 8, 40].
The laryngeal tube was introduced as an alternative to the LMA for managing difficult airway situations, both in the hospital and in the prehospital setting. The laryngeal tube then became rapidly established in many emergency medical services (EMS) and its use was implemented in international guidelines [2]. The laryngeal tube has now been modified so that different versions of this device are used in the prehospital setting [laryngeal tube (LT), disposable version (LT-D), laryngeal tube suction mark II (LTS II), and disposable version (LTS D), all VBM, Sulz, Germany].
Studies describing the successful use of the laryngeal tube in the prehospital setting sound promising [9, 10, 22]. However, the results of these studies and of case reports were not reported by an independent observer and, therefore, reporting bias could be possible [11, 22]. Only one prospective, randomized study has confirmed that the LTS-D is comparable to ETI in the prehospital setting [41]. Indeed, the successful use of the laryngeal tube depends on individual performance in carrying out the airway maneuver (e.g., skill, experience, and qualification). The following case series presents the problems and complications upon arrival in the emergency department described by emergency physicians independently of the prehospital emergency personnel. These observations raise questions concerning the safety and usefulness of a laryngeal tube in the prehospital setting.
Methods
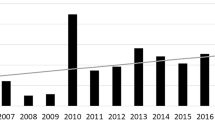
Clinical observations were made in a nonconsecutive series of patients between 2007 and 2012. All patients were admitted to the resuscitation rooms of emergency departments (ED) at tertiary care hospitals (University Hospital of Heidelberg, Hospital of Fulda, University Hospital of Leipzig). Reporting data in the present form was approved by the ethics committee of the Medical Faculty of Leipzig, Germany. Single cases were documented initially after ED admission. The case series was evaluated retrospectively, was not preregistered, and written informed content could not be obtained.
Results
Patient characteristics and the clinical problems associated with the use of the LT are described in detail in the following section.
Case report 1
A 50-year-old patient fell down the stairs. He was initially in stable cardiopulmonary condition but unconscious according to the Glasgow Coma Scale (GCS), with a GCS of 3. An EMS physician inserted a LTS II without attempting ETI first. Capnography was not used at the scene or during transport. Upon arrival in the ED, the patient was severely cyanotic. Upon hospital admission, the patient developed asystole. Cardiopulmonary resuscitation (CPR) was initiated immediately. End-expiratory carbon dioxide (etCO2) could not be detected using capnography after handing the patient over in the ED. Considering misplacement and expecting an endotracheal position, the LT was removed immediately, and endotracheal intubation was performed without any difficulty. Return of spontaneous circulation (ROSC) was achieved within the following 3 min of CPR. Immediately after endotracheal intubation, blood gas analysis showed combined severe respiratory and metabolic acidosis (pH 6.7, paCO2 164 mmHg, paO2 62 mmHg, base excess − 21 mmol/l). CT scan demonstrated extensive brain edema, a massively swollen stomach, abnormally large amounts of air in the small and large intestines, and massive aspiration. The only injury found was a fracture of the spinous process of the seventh cervical vertebra that did not compromise the spinal cord. The patient died 6 days after being admitted to the intensive care unit (ICU).
Case report 2
A 55-year-old patient suffered from an out-of-hospital cardiac arrest and associated fall. A LT was inserted by a paramedic without attempting ETI first. The arriving EMS physician refrained from switching over to a tracheal tube in the field. However, as a result of using LT during the prehospital interval of 45 min, the patient’s tongue had swollen considerably (Fig. 1). After ED admission, the LT was removed and subsequent laryngoscopy proved to be very difficult (Cormack–Lehane grade IV), most probably as a consequence of the swollen tongue. ETI was performed successfully by using a McCoy blade. The patient survived without any neurological sequelae.
Case report 3
A 65-year-old patient (body mass index 57 kg/m2) suffered from out-of-hospital cardiac arrest. A LTS II was inserted initially by an EMS physician without attempting ETI first. ROSC was achieved in the prehospital setting after CPR. However, capnography was not used in the prehospital setting. Upon arrival in the ED, peripheral oxygen saturation could not be detected although blood pressure and heart frequency were normal. A clearly audible ventilation synchronous leak was perceived alongside the inserted LT in the ED. The end-expiratory minute volume was low (3.5 l/min). After introduction of emergency anesthesia, the LT was removed and laryngoscopy showed a severely cyanotic and thickened tongue; the posterior pharyngeal wall was swollen, and blood had covered the entire oropharynx. Conventional laryngoscopy demonstrated a Cormack–Lehane grade IV. ETI was performed successfully with a McCoy blade. Thereafter, a CT scan was performed and confirmed a pulmonary embolism. The patient died of right ventricular failure in the course of the next few days on the ICU.
Case report 4
A 55-year-old patient suffered from out-of-hospital cardiac arrest. After CPR was initiated by bystanders, a paramedic inserted a LTS II without attempting ETI first. After 20 min of CPR and after arrival of an EMS physician, the patient achieved ROSC. During the prehospital course, a clearly audible ventilation synchronous leak was perceived alongside the inserted LT; however, no attempts were made to manage this problem. After arrival in the ED, this sound was remarkable, the abdomen was obviously swollen, and mechanical ventilation was inadequate [low etCO2, low end-expiratory minute volume (2.4 l/min)]. The LT was removed immediately, and subsequent ETI proved to be very easy (Cormack–Lehane grade I). Due to hypoventilation during the prehospital course, the initial blood gas analysis demonstrated a combined severe respiratory and metabolic acidosis (pH 6.6, paCO2 169 mmHg, paO2 89 mmHg, base excess − 22 mmol/l). The patient was transferred to the cardiac catheter laboratory for immediate PCI but died of multi-organ failure on hospital day 7 on the ICU.
Case report 5
A 25-year-old patient suffered a high-speed motorcycle accident and was found with a GCS 5. After failed ETI within two attempts and aspiration of a considerable amount of blood from the oropharynx, a LT was placed by the EMS physician. The patient was then handed over to an air rescue team. Due to the information reported by the first EMS team, the physician of the air rescue system abstained from switching the LT to a tracheal tube. Mechanical ventilation was assumed to be sufficient for the patient and difficult ETI conditions were suspected. During air transport, the patient suffered from cardiac arrest and arrived in the ED undergoing CPR with inadequate ventilation. In the ER, ETI was performed immediately and without any problems. Owing to an instable chest with several rib fractures, bilateral tension pneumothorax was clinically suspected and immediately treated by inserting chest tubes. The CT scan confirmed a thoracic trauma with pneumothorax and severe aspiration. The patient died of abdominal and thoracic injuries in the ED.
Case report 6
A 22-year-old patient was the victim of a high-speed motor vehicle accident. Initial GCS was 5 but his respiration and cardiopulmonary condition were stable. Still entrapped in his vehicle, a LTS II was inserted by an EMS physician through the window on the driver’s side. During extrication and 20 min after insertion, the LTS II was subsequently dislocated. It was not possible to reinsert the LTS II. Laryngoscopy demonstrated massive swelling of the throat and vocal cords. The patient’s cardiopulmonary condition worsened and he ultimately suffered cardiac arrest. Cricothyroidotomy was performed, and the patient arrived in the ED under prolonged CPR. ROSC could not be established in the ED.
Case report 7
A 32-year-old patient suffered from severe head injury with midfacial fractures after a fall from a height of 8 m. The patient was breathing spontaneously and in stable cardiopulmonary condition with a GCS of 6. After induction of emergency anesthesia, ETI attempts failed due to blood in the oropharynx, and thus the EMS physician inserted a LTS II. Upon arrival in the ED, using manual bag-valve ventilation, the patient’s ventilation was inadequate due to LT displacement, as verified by low expiratory minute volume. ETI was successful after inducing anesthesia with neuromuscular blockade and aspirating blood from the oropharynx. Whole-body MSCT confirmed the diagnosis of severe head injury with a dismal prognosis. The patient died on the ICU.
Case report 8
A 70-year-old patient suffered from out-of-hospital cardiac arrest. A LT was inserted by a paramedic without attempting ETI first. The patient achieved ROSC after arrival of an EMS physician and a CPR duration of 5 min. During the transport, however, the patient’s ventilation became increasingly difficult, with a peak airway pressure of > 40 cmH2O and a drop in peripheral oxygen saturation. Upon arrival in the ED, ventilation was inadequate and airway obstruction was highly suspected. The LT was removed immediately and the cause of the ventilation problem recognized: the LT and the trachea were obstructed by chunks of bread. The bread was extracted from the oropharynx using a Magill forceps and ETI was performed with no difficulty. The patient was transferred to the ICU and survived.
Discussion
Securing the airway and effectively managing oxygenation and ventilation play a central role in emergency medicine. Up to now, ETI has been considered the gold standard for securing the airway. Depending on the experience of the person performing the procedure, however, exceptions are sometimes made to applying the gold standard and alternative methods are recommended [3]. Currently, SGA have shifted into the focus not only as an alternative for difficult ETI but also to replace conventional bag–valve mask ventilation [12]. However, a recently published secondary analysis of data from the multicenter Resuscitation Outcome Consortium (ROC) PRIMED trial showed that outcome was better after ETI than after inserting SGA in patients suffering from out-of-hospital cardiac arrest [47].
Most studies investigating SGA have been performed on airway trainers or in routine clinical situations in anesthetized patients [13, 14, 15, 17, 18, 42]. In prehospital research settings, both EMS physicians and paramedics have used the laryngeal tube [19, 20, 21, 43, 44]. The insertion technique is described as being simple and easy to learn, and the rate of correctly and safely placing the laryngeal tube (here: LTS-D) is reported to be high even for inexperienced personnel [22]. However, various and severe complications have been observed in using the laryngeal tube [9, 16, 17, 44].
The main point of presenting this case series is to show that laryngeal tube-associated problems can occur and that the provider must be aware of all the problems and needs to deal with them. Therefore, the problems described in this case series are related to the following:
-
laryngeal tube,
-
(lack of) monitoring (e.g., capnography),
-
user (deficits), and
-
management of patients with laryngeal tube in situ upon hospital admission.
First, the risks of using the laryngeal tube presented in this paper should be applied in the decision-making process, since SGA-associated problems can cause complications (Tab. 1). Other studies report incorrect positioning of laryngeal tubes during in-hospital and prehospital conditions [28, 42, 44]. Keeping this in mind, the findings in case 1 suggest misplacement, speculatively in the trachea. In fact, owing to its construction, the laryngeal tube can cause hypoxia when the distal end is incorrectly positioned in the trachea or it is misplaced in the glottis level, both not recognized.
Other kinds of obstruction are also possible using laryngeal tubes [16]: The use of a cervical immobilization collar can cause caudal herniation of the pharyngeal cuff of the LT, with subsequent obstruction of the ventilation orifices. Rotation of the LTS II along its longitudinal axis (caused by tension of the rigid tube of the ventilator) can render ventilation instantly impossible. Deep esophageal insertion of a LTS II that is too large may result in impossible ventilation (ventilation orifices obstructed by esophageal mucosa; case 7). If the laryngeal tube is not correctly placed in the esophagus or the cuff of the LT/LTS is blocked at the level of the larynx, the laryngeal structures can be compressed or the airways completely obstructed [16, 44]. Subsequently, the air that is insufflated exerts uncontrolled airway pressure on the upper esophageal sphincter [16]. If the pressure on the upper esophageal sphincter drops rapidly during cardiac arrest, air will inevitably be forced into the stomach [31]. In such situations, any subsequent airway pressure that is applied will be directed to the esophagus and ventilation will be inadequate. Furthermore, the lower part of the LT/LTS can bend such that the distal cuff is located in the larynx instead of the esophagus and the air flow is blocked [16, 28]. This would also cause stomach insufflation [28]. If air is directed into the stomach due to obstruction, regurgitation and aspiration are inevitable as the upper cuff in the pharynx prevents air from flowing out through the mouth. These kinds of obstruction apply in general for all versions of the laryngeal tube.
It is also possible to misplace the tip of the laryngeal tube in the piriform sinus, which can also result in leakage, gastric insufflation, and even airway trauma with a swollen pharyngeal wall or tongue [16, 44]. Therefore, laryngeal tubes with the possibility to insert a gastric tube should be preferred [40]. If problems are encountered in inserting a gastric tube soon after a LTS has been placed, it can be assumed that the lower part of the LTS is bent, thus, causing this obstruction, and the LTS must be inserted again. However, adequate ventilation must be controlled by auscultation and capnography after inserting any device (case 1).
Difficulties in initial tube positioning, tube dislocation, and aspiration (case 6) were reported in 25, 13, 5 %, respectively [43, 44]. ETI is the gold standard for airway management in trauma patients [30] and SGA may be a useful strategy in entrapped patients. However, in an entrapped patient under worse conditions, this should only be the “last resort” treatment and in an individual case. In the majority, however, high-flow oxygen via a face mask is sufficient to bridge the time until the patient can be reached for proper airway management.
As reported for other devices, the tongue and laryngeal swelling in cases 2, 3, and 6 do not represent a laryngeal tube-specific problem [32, 33, 34, 35, 43]. The mechanism ultimately underlying the tongue swelling is still unknown (e.g., venous stasis, secondary tissue edema). However, tongue swelling associated with the use of a laryngeal tube is almost always related to inappropriate cuff pressure. Using the amount of air indicated with color markings on the syringe may result in excessive cuff pressure above 100 mmHg. Such high cuff pressure can interfere with both the arterial blood supply to the tongue and venous drainage. Therefore, after prehospital or in-hospital initial placement of a laryngeal tube and cuff inflation, it is important to adjust and monitor cuff pressure.
Furthermore, blood in the oropharynx can be the result of traumatic insertion of the laryngeal tube, particularly if the laryngeal tube was inserted without actively creating sufficient retropharyngeal space by means of a chin lift manoeuver or with a laryngoscope.
Second, training for assessing/controlling/monitoring correct positioning and adequate ventilation is as important as inserting a SGA. In case 1, insufficient airway management is described and, retrospectively, the fatal outcome could have been avoided if capnography had been used. Thus, auscultation and capnography need to be integrated into training programs. Ultimately, capnography should be employed whenever the airway needs to be secured [38]. Since 2007, an EMS in Germany can be held liable if rescue vehicles are not equipped with capnography [27]. Cases 1 and 3 show, however, that capnography is still not always utilized, even today. Unrelated to the use of a specific device, a prehospital provider must detect incorrect placement by using capnography, and neglecting to do this plays a significant role in the catastrophic outcome here, possibly independently of the airway device being employed.
Third, not all EMS providers have sufficient expertise in airway management (ETI and SGA). In Germany,the results of a survey published 7 years ago reported that 18 % of nonanesthesiological EMS physicians had only performed 20 ETI procedures and 53 % had performed 20–100 such procedures in the in-hospital setting [23]. Furthermore, the individual EMS physician only performed an ETI procedure twice per month during air rescue missions and only every 1.4 months during ground rescue missions [24]. Sufficient skills and experience—especially in airway management—cannot be achieved through work in the field alone [23, 24]. Moreover, an older evaluation showed that 42 % of nonanesthesiological EMS physicians have no practical experience in using SGA [23].
Presently, there is no national regulation concerning the number of successful ETI procedures necessary before a physician is allowed to function as a prehospital provider in Germany [25, 26, 40]. Likewise, practical experience in using SGA has not been defined in the emergency medicine curriculum. The corresponding requirements for paramedics also lack such specifications. A recently published statement of the German Society of Anaesthesiology and Intensive Care Medicine gives for the first time clear recommendations for prehospital qualification of paramedics and out-of-hospital physicians concerning endotracheal intubation and SGA (e.g., 100 ETI under supervision, then 10 ETI per year, 10 SGA under supervision, and 3 SGA per year) [40]. This statement is supported by one from the Association of Anaesthetists of Great Britain and Ireland, which has also provided recommendations for the qualification of prehospital airway providers [48]. In particular, the use of bag–valve mask ventilation, SGA, and even rapid-sequence induction in routine clinical management such as in anesthesiology, intensive care medicine, or prehospital and in-hospital emergency medicine settings should be a prerequisite for successful use of these methods. Regular training both in airway management and in routinely inducing anesthesia should be considered mandatory for EMS physicians. Indeed, the problems in these case reports might be a consequence of insufficient individual clinical expertise and airway management skills.
EMS physicians, in particular, who do not practice airway management daily, should be sensitized to the presented problems in this case series. This also applies to paramedics who are increasingly employing laryngeal tubes as part of their “extended skills”. This involves more than mastering the clinical skills for performing an ETI or inserting SGA. However, keeping in mind that manikin training alone was reported to be insufficient, this represents a dilemma since the laryngeal tube has not been comprehensively and regularly applied for routine anesthesia or in other clinical procedures [29].
It should be kept in mind that, in line with guidelines in Germany for prehospital airway management of patients suffering from multiple trauma, if oxygenation and ventilation are adequate and the provider is uncertain about his/her airway skills, patients can be transferred with a “scoop and run” strategy to the hospital without inserting endotracheal tube or any kind of SGA [30].
Fourth, management of the patient treated with laryngeal tube upon hospital admission should be highlighted: Perceiving the risk potential in a given situation is particularly relevant for the staff who take over. Upon arrival at the emergency scene or ED, the new staff immediately needs to assess oxygenation and ventilation and take preparatory measures for reintubation. It is undoubtedly important that alternative strategies are available for securing the airway when difficult ETI conditions are already known from prehospital management [45]. In addition and as demonstrated in this paper, the use of laryngeal tubes as the primary airway in the field can be associated with relevant, subsequent problems. Several cases (cases 1–4, 8) demonstrate this clearly. Standard procedures for managing difficult airways should be performed in the ED and physicians who are experienced in airway management should be involved in primary care.
After a laryngeal tube has been inserted by a former provider, the EMS physician or the ED staff that takes over must decide whether to keep it in place or to replace it by an endotracheal tube. In the authors’ view, the decision to replace a laryngeal tube that has been successfully inserted and is providing adequate ventilation, while being continuously monitored by capnography, should be critically weighed against the option of removing it to enforce the gold standard ETI. The decision to remove the laryngeal tube should depend on the given situation, the success of oxygenation and ventilation, and the patient’s individual risk profile. Numerous factors affect this decision, not least the experience of the provider. However, if problems occur after inserting a laryngeal tube (A-Problem), the provider must recognize and resolve them, even though this means removing the laryngeal tube and switching to a tracheal tube (cases 1 and 5). If problems with ventilation persist after replacing the laryngeal tube by an ETI, typical reversible causes should be considered and treated (e.g., tension pneumothorax, B-Problem). In particular for patients suffering from multiple injuries, especially from thoracic injury and/or apparent aspiration (case 6) who may require high airway pressures, it should be considered strictly unacceptable to refrain from ETI because of inexperience in favor of a seemingly easier procedure for securing the airways [36].
SGA often only represent a temporary solution. At the latest upon hospital admission, even a well-positioned laryngeal tube that is ventilating the patient sufficiently will need to be replaced by a tracheal tube with respect to a presumably longer period of ventilation and/or likely difficult mechanical ventilation with higher PEEP. When the airway conditions are indeed difficult, a tracheotomy may need to be considered. The best procedure must be gauged in each individual case with respect to the individual situation (e.g., videolaryngoscope) [46].
We know that the presented case reports could be discussed controversially. A limitation of our study is the nature of the presented nonconsecutive case series. Therefore, these case reports only present examples of such complications and describe what happened when the complications were not treated very well. As another consequence, care must be taken in comparing our findings with the incidence of airway catastrophes in other studies [39]. Although this question cannot be addressed owing to the design of this study, the findings are essential: Because this may constitute the tip of the iceberg, insufficient airway management is an actual problem at the scene and SGA should not be claimed to be helpful in these situations. In this context, it is hazardous not to recommend acquiring practical skills for the use of SGA in a prehospital setting. As another limitation of this nonconsecutive case series, which is given from the emergency department’s point of view, the clinical background and the level of experience of each of the involved prehospital emergency physicians or paramedics is unknown.
Conclusion
Laryngeal tubes are considered to be effective, safe, and rapid SGAs. Operators must be aware of the operator- und procedure-related complications of laryngeal tubes, and they must recognize them. In order to prevent tongue swelling, after initial prehospital or in-hospital placement of laryngeal tube and cuff inflation, it is important to adjust and monitor the cuff pressure. Problem-solving strategies should be taught in seminars and training courses and further education must include employing the device in patients, perhaps in the OR [37]. Furthermore, and particularly in difficult airway situations, capnography is mandatory [38]. Ultimately, the success of inserting the laryngeal tube can only be as good as the operator’s training.
References
Berlac P, Hyldmo PK, Kongstad P et al (2008) Pre-hospital airway management: guidelines from a task force from the Scandinavian society of anaesthesiology and intensive care medicine. Acta Anaesthesiol Scand 52:897–907
Deakin CD, Nolan JP, Soar J et al (2010) European resuscitation council guidelines for resuscitation 2010. Section 4. Adult advanced life support. Resuscitation 81:1305–1352
Paal P, Herff H, Mitterlechner T et al (2010) Anaesthesia in prehospital emergencies and in the emergency room. Resuscitation 81:148–154
Komatsu R, Kasuya Y, Yogo H et al (2010) Learning curves for bag-and-mask ventilation and orotracheal intubation. An application of the cumulative sum method. Anesthesiology 112:1525–1531
Konrad C, Schüpfer G, Wietlisbach M, Gerber H (1998) Learning manual skills in anesthesiology: is there a recommended number of cases for anesthestic procedures? Anesth Analg 86:635–639
Caplan RA, Benumof JL, Berry FA et al (2003) ASA task force on difficult airway management. Practice guidelines for management of the difficult airway. Anesthesiology 98:1269–1277
Heidegger T, Gerig HJ, Henderson JJ (2005) Strategies and algorithms for the management of difficult airway. Best Pract Res Clin Anaesthesiol 19:661–674
Henderson JJ, Popat MT, Lotto IP, Pearce AC (2004) Difficult airway society guidelines for management of the unanticipated difficult intubation. Anaesthesia 59:675–694
Schalk R, Meininger D, Ruesseler M et al (2011) Emergency airway management in trauma patients using laryngeal tube suction. Prehosp Emerg Care 15:347–350
Gahan K, Studnek JR, Vandeventer S (2011) King LT-D use by urban basic life support first responders as the primary airway device for out-of-hospital cardiac arrest. Resuscitation 82:1525–1528
Emerson GB, Warme WJ, Wolf FM et al (2010) Testing for the presence of positive-outcome bias in peer review. A randomized controlled trial. Arch Intern Med 170:1934–1939
Schalk R, Scheller B, Habler O et al (2008) Disposable laryngeal tube suction—a randomized comparison of two insertion techniques performed by novice users in anaesthetised patients. Resuscitation 76:364–368
Keul W, Bernhard M, Völkl A et al (2004) Methods of airway management in the prehospital emergency medicine. Anaesthesist 53:978–992
Kurola JO, Turunen MJ, Laakso JP et al (2005) A Comparison of the laryngeal tube and bag–valve mask ventilation by emergency medical technicians: a feasibility study in anesthetized patients. Anesth Analg 101:1477–1481
Kurola J, Harve H, Kettunen T et al (2004) Airway management in cardiac arrest-comparison of the laryngeal tube, tracheal intubation and bag–valve mask ventilation in emergency medical training. Resuscitation 61:149–153
Dengler V, Wilde P, Byhahn C et al (2011) Prehospital airway management of laryngeal tubes. Should the laryngeal tube S with gastric drain tube be preferred in emergency medicine? Anaesthesist 60:135–138
Mihai R, Knottenbelt G, Cook TM (2007) Evaluation of the revised laryngeal tube suction: the laryngeal tube suction II in 100 patients. Br J Anaesth 99:734–739
Russo CS, Wilcox CL, House HR (2007) The laryngeal tube device: a simple and timely adjunct to airway management. Am J Emerg Med 25:263–267
Heuer JF, Barwing J, Eich C et al (2010) Initial ventilation through laryngeal tube instead of face mask in out-of-hospital cardiopulmonary arrest is effective and safe. Eur J Emerg Med 17:10–15
Schalk R, Byhahn C, Fausel F et al (2010) Out-of-hospital airway management by paramedics and emergency physicians using laryngeal tubes. Resuscitation 81:323–326
Wiese CH, Semmel T, Müller JU et al (2009) The use of the laryngeal tube disposable (LT-D) by paramedics during out-of-hospital resuscitation—an observational study concerning ERC guidelines 2005. Resuscitation 80:194–198
Scheller B, Walcher F, Byhahn C et al (2010) Laryngeal tube suction. Temporary device for emergency patients with a difficult airway. Anaesthesist 59:210–216
Timmermann A, Braun U, Panzer W et al (2007) Out-of-hospital airway management in northern Germany. Physician-specific knowledge, procedures and equipment. Anaesthesist 56:328–334
Gries A, Zink W, Bernhard M et al (2006) Realistic assessment of the physician-staffed emergency services in Germany. Anaesthesist 55:1080–1086
Bernhard M, Mohr S, Weigand MA et al (2012) Developing the skill of endotracheal intubation: implication for emergency medicine. Acta Anaesthesiol Scand 56:164–171
Reifferscheid F, Harding U, Dörges V et al (2010) Implementation of a specialist qualification in emergency medicine—do we now have uniform requirements in Germany? Anästh Intensivmed 51:82–89
Genzwürker H, Lessing O, Ellinger K et al (2007) Infrastructure of emergency medical services. Comparison of physician-staffed ambulance equipment in the state of Baden-Wuerttemberg in 2001 and 2005. Anaesthesist 56:665–672
Kikuchi T, Kamiya Y, Ohtsuka T et al (2008) Randomized prospective study comparing the laryngeal tube suction ii with the Proseal™ laryngeal mask airway in anesthetized and paralyzed patients. Anesthesiology 109:54–60
Rai MR, Popat MT (2011) Evaluation of airway equipment: man or manikin. Anaesthesia 66:1–3
Bernhard M, Matthes G, Kanz KG et al (2011) Emergency anesthesia, airway management and ventilation in major trauma. Background and key messages of the interdisciplinary S3 guidelines for major trauma patients. Anaesthesist 60:1027–1040
Gabrielli A, Wenzel V, Layon AJ et al (2005) Lower esophageal sphincter pressure measurement during cardiac arrest in humans: potential implications for ventilation of the unprotected airway. Anesthesiology 103:987–899
Gaither JB, Matheson J, Eberhardt A, Colwell CB (2010) Tongue engorgement associated with prolonged use of the king-LT laryngeal tube device. Ann Emerg Med 55:367–369
Khaja SF, Provenzano MJ, Chang KE (2010) Use of the king LT for emergency airway management. Arch Otolaryngol Head Neck Surg 136:979–982
Stillman PC (2003) Lingual oedema associated with the prolonged use of an inappropriately large laryngeal mask airway (LMA™) in an infant. Paediatr Anaesth 13:637–639
Twigg S, Brown JM, Williams R (2000) Swelling and cyanosis of the tongue associated with use of a laryngeal mask airway. Anaesth Intensive Care 28:449–450
Bernhard M, Helm M, Aul A, Gries A (2004) Preclinical management of multiple trauma. Anaesthesist 53:887–904
Schalk R, Auhuber T, Haller O et al (2012) Implementation of the laryngeal tube for prehospital airway management. Training of 1,069 emergency physicians and paramedics. Anaesthesist 61:35–40
Timmermann A, Brockmann JC, Fitzka R, Nickel EA (2012) Measurement of carbon dioxide in emergency medicine. Anaesthesist 61:148–155
Timmermann A, Russo SG, Eich C et al (2007) The out-of-hospital esophageal and endobronchial intubations performed by emergency physicians. Anesth Analg 104:619–623
Timmermann A, Byhahn C, Wenzel V et al (2012) Handlungsempfehlung für das präklinische Atemwegsmanagement. Für Notärzte und Rettungsassistenten. Anästh Intensivmed 53:294–308
Frascone RJ, Russi C, Lick C et al (2011) Comparison of prehospital insertion success rates and time to insertion between standard endotracheal intubation and a supraglottic airway. Resuscitation 82:1529–1536
Russo SG, Cremer S, Galli T et al (2012) Randomized comparison of the i-gel™, the LMA Supreme™, and the laryngeal tube suction-D using clinical and fiberoptic assessments in elective patients. BMC Anesthesiol 12:18
Müller JU, Semmel T, Stepan R et al (2013) The use if the laryngeal tube disposable by paramedics during out-of-hospital cardiac arrest: a prospectively observational study (2008–2012). Emerg Med J 30:1012–1016
Sunde GA, Brattebo G, Odegarden T et al (2012) Laryngeal tube use in out-of-hospital cardiac arrest by paramedics in Norway. Scand J Trauma Resusc Emerg Med 20:84
Kahja SF, Chang KE (2013) Airway algorithm for the management of patients with a king LT. Laryngoscope 124:1123–1127
Schalk R, Weber CF, Byhahn C et al (2012) Reintubation using the C-MAC videolaryngoscope. Implementation in patients with difficult airways initially managed with in situ laryngeal tubes. Anaesthesist 61:777–782
Wang HE, Szydlo D, Stouffer JA et al (2012) Endotracheal intubation versus supraglottic airway insertion in out-of-hospital cardiac arrest. Resuscitation 83:1061–1066
http://www.aagbi.org/sites/default/files/prehospital_glossy09.pdf. Accessed 02 June 2014
Authors’ contributions
MB, WB, and AG collected the cases. MB, WB, CAG, AT, and AG analyzed the pertinent complications and problems. MB, WB, and AG prepared the first version of the manuscript. UXK, RS, AT, and CAG contributed intellectually to the writing process and performed substantial corrections. All authors participated in the writing process. All authors read and approved the final manuscript.
Acknowledgement
We would like to thank Dr. T.K. Becker (Department of Emergency Medicine, University of Michigan) for his assistance in preparing the English version of this manuscript.
Compliance with ethical guidelines
Conflict of interest. M. Bernhard, W. Beres, A. Timmermann, R. Stepan, C.-A. Greim, U.X. Kaisers, and A. Gries state that there are no conflicts of interest. The accompanying manuscript does not include studies on humans or animals.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bernhard, M., Beres, W., Timmermann, A. et al. Prehospital airway management using the laryngeal tube. Anaesthesist 63, 589–596 (2014). https://doi.org/10.1007/s00101-014-2348-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00101-014-2348-1
Keywords
- Respiration, artificial
- Emergency medical service
- Endotracheal intubation
- Professional competence
- Adverse effect