- 1Centre of Expertise Urban Vitality, Faculty of Health, Amsterdam University of Applied Science, Amsterdam, Netherlands
- 2Jellinek Prevention, Arkin, Amsterdam, Netherlands
As in many other countries worldwide, the coronavirus pandemic prompted the implementation of an “intelligent lockdown” in the spring of 2020 in the Netherlands, including the closure of nightlife venues and cancellation of festivals. Such restrictions and social distancing could particularly affect people who use alcohol or other drugs in recreational settings and give rise to new challenges and additional needs in the field of addiction prevention and care. To monitor changes in substance use and provide services with practical directions for tailored prevention, an anonymous web survey was set up, targeting a convenience sample aged 16 years or older through various social media and other online channels. Between May and October 2020, a total of 6,070 participants completed the survey, mainly adolescents and young adults (16–24 years old). These data were used to explore and describe changing patterns in substance use. Overall results showed declined current use compared to “pre-corona,” but mask underlying variation in changing patterns, including discontinued (tobacco 10.4%, alcohol 11.3%, cannabis 16.3%, other drugs 30.4%), decreased (tobacco 23.0%, alcohol 29.1%, cannabis 17.4%, other drugs 20.7%), unchanged (tobacco 30.3%, alcohol 21.2%, cannabis 22.3%, other drugs 17.3%), increased (tobacco 29.6%, alcohol 32.1%, cannabis 32.9%, other drugs 25.3%), and (re)commenced use (tobacco 6.7%, alcohol 6.3%, cannabis 11.1%, other drugs 6.2%). Especially the use of drugs like ecstasy and nitrous oxide was discontinued or decreased due to the lack of social occasions for use. Increased use was associated with coping motives for all substance types. As measures combatting the coronavirus may need to be practiced for some time to come, possibly leading to prolonged changes in substance use with lingering “post-corona” consequences, timely and ongoing monitoring of changing patterns of substance use is vital for informing prevention services within this field.
Introduction
The pandemic of coronavirus disease 2019 (COVID-19) has massively affected the lives of people all over the world. Countries have taken drastic measures to contain the outbreak, from curfews to national quarantines. In March 2020, the Dutch government implemented a so-called “intelligent lockdown” to mitigate the spread of the virus. Daycare centers, schools and universities were closed, as were sports clubs, libraries, cinemas, theaters, museums, restaurants and nightlife venues; large social gatherings and events were canceled; almost all “contact professions” (e.g., hairdressers, driving instructors, physiotherapists) were suspended; both public and private meetings of people from different households were rigorously restricted; and 1.5-m social distancing and work-from-home orders were issued. In June most measures were lifted or relaxed (provided 1.5-m distance was maintained, thus restricting numbers of guests and customers), though festivals and club nights remained prohibited. However, rising infection rates warranted gradually more stringent measures from August onwards, yet again impeding social occasions like sports games, cultural outings, going out for drinks or dinner, or inviting friends to a party at home.
The impacts of both the coronavirus and the measures taken to reduce its spread are severe and disrupting on many societal levels, including public mental health (1, 2). Several authors have predicted or expressed concern about increased substance use liability due to emotional distress (3–9). However, Rehm et al. (10) postulated two (not mutually exclusive) scenarios with opposite predictions regarding the impact of the current pandemic on the level and patterns of alcohol consumption. The first scenario predicts an increase in consumption due to psychological distress, while the second scenario predicts a lowered level of consumption due to decreased physical and financial availability.
There is a growing amount of literature about the coronavirus and substance use, but many of these studies address the heightened risks of people using substances in contracting the virus or having poorer disease prognosis [cf. (11)]. Research into changing patterns of substance use is less common and often limited to alcohol and/or tobacco (12–24); some studies (also) look into changes in the use of cannabis (25–30), but few were found that included other drugs like “party drugs” that tend to be predominantly used in social contexts affected by the coronavirus measures (31–33).
Measures combatting the coronavirus may need to be practiced until 2022 (34), possibly leading to prolonged changes in substance use with lingering “post-corona” consequences. Health policy makers and services are expected to proactively address the emerging changes and related risks needs. Monitoring changing patterns of substance use is therefore vital for prevention and addiction care when developing and delivering appropriate public health responses and interventions. With all festivals being suspended and nightlife venues closed due to the “intelligent lockdown,” prevention practice lost sight of a large and important group of people who use alcohol and other drugs in recreational settings. At the same time, restrictions and social distancing could particularly affect this population, resulting in changing substance use patterns and practices with associated risks. A signaling tool was rapidly needed to provide prevention services with practical directions for relevant and tailored educational information to promote healthy behaviors within this field.
Antenna Amsterdam (35) is an ongoing monitoring scheme that has been documenting developments and trends in recreational substance use in the Dutch capital since 1993, making it the oldest of such monitors running in Europe (36). Part of the mixed-methods approach is an annual on-site survey among varying target groups, including pub-goers and visitors of clubs and dance events. To address the needs of prevention services throughout the Netherlands for timely directions for targeted action an alternative nationwide online survey was set up. Interim national and regional results of the survey were regularly shared in dashboards and infographics within the Dutch network of prevention organizations to monitor changes in substance use patterns.
This paper is based on partial and preliminary data from this survey. Since the survey cannot be used to estimate drug use prevalence of the general population (37) and was not designed as an epidemiological effect study, the aim of this paper is not to test pre-formulated hypotheses about the impact of measures combating the coronavirus on public health, but to explore and describe changing patterns in substance use. Using the survey data we aim to assess to what extent the aforementioned scenarios of increased and decreased alcohol consumption (10) have taken place among people who use alcohol in the Netherlands, and if these scenarios also apply to the use of tobacco, cannabis and other drugs.
Materials and Methods
Sample
In May 2020, the “Antenne NL Corona Special” survey about substance use, gaming and gambling during the coronavirus pandemic went online. A convenience sample was recruited by circulating the link through the university and the network of organizations for treatment and prevention of substance use and abuse throughout the Netherlands. Methods included placing targeted advertisements on social media platforms such as Facebook and Instagram, posting messages on websites and in newsletters, and sharing via communication channels of various interventions and programs. There was no predefined target population and the link could be widely disseminated, but recruitment efforts could also be aimed at (varying) specific groups (e.g., students) or users (e.g., alcohol consumers). The questionnaire was accessible for anyone aged 16 years or older. By commencing the survey, participants gave electronic consent to understanding the study purpose, being aware of voluntariness and anonymity (no identifying information or IP address was recorded), and permitting storage and use of their responses.
Between 12 May and 13 October 2020, the survey was completed 6,380 times. Repeated participation was allowed and reported in 310 (4.9%) questionnaires. Because questions about the “pre-corona” period could be skipped when participating for the second or subsequent time, this paper is based on a selection of 6,070 questionnaires where participants indicated first-time participation (answered negatively to the first question “Have you participated in this survey before?”).
In this paper, we focus on the use of tobacco, alcohol, cannabis and other drugs (omitting gaming and gambling) prior to the time the measures combatting the coronavirus were enforced on 16 March 2020 in the Netherlands (further on: “pre-corona” use) and current use.
Measures
The online self-report questionnaires included the following measures.
Demographics were covered by questions about sex (male, female, other), age, residential municipality, type of persons participants were living with (multiple choice: none, parents, partner, housemates, children, other), enrollment in school or university (no, secondary or secondary vocational school, higher professional school, or university), and current working situation.
For current substance use, as narrow a time frame as possible was chosen to take into account the rapidly changing corona situation. For alcohol, tobacco and cannabis this was the last week, but for other drugs that are usually not used weekly by most this was stretched to last month. In an effort to measure “typical” substance use prior to the corona pandemic for comparison, the same narrow time frames would not be appropriate. Instead, use of alcohol, tobacco and cannabis was asked retrospectively for the pre-corona month (15 Feb−15 Mar 2020) and use of other drugs was asked for the pre-corona year (15 Mar 2019–15 Mar 2020).
Use of tobacco, alcohol and cannabis was measured by questions about the number of use days per week (0–7) and average amount (number of cigarettes/glasses/joints) per use day. Use of other drugs was measured by a multiple choice list (yes, no) of eleven substances: ecstasy (XTC/MDMA), amphetamines, cocaine, nitrous oxide, ketamine, LSD, psychedelic mushrooms/truffles, GHB, 2C-B, 3-MMC/4-MMC and/or any other drug (excluding tobacco, alcohol, cannabis, and prescription drugs).
Changes in substance use were derived from weekly consumption for tobacco, alcohol and cannabis (see Analyses). For other drugs, participants were asked in a single overall question to self-indicate whether they were using (a lot) more or less (frequently) than “pre-corona.”
To asses motives for current use a short ad-hoc list of eight reasons was developed: Because I find it pleasant/fun/mind-expanding; Because I find it makes social moments more fun/cozy; Because I needed an outlet now that there are few other options; Because I wanted to feel less worried/afraid/angry/stressed; Because I wanted to feel less lonely; Because I couldn't resist, at a time when I actually didn't want to; Because I already had it at home; Because I always do at those moments, out of habit. Answer categories for each of these reasons were: totally agree, agree, neutral, disagree, totally disagree.
An ad-hoc eight-item multiple choice list (yes, no) was developed to asses reasons for current discontinued or decreased other drug use: It's better for my state of mind; It's better for my health/fitness; I had less free time; I had fewer social occasions (going out, appointments, visits, parties, etc.); I was home alone less often; Someone in my environment has asked for it; I was ill/did not feel well. This question was not asked for tobacco, alcohol or cannabis use.
Analyses
For the purpose of analyses, age was recoded into four categories (16–17 years, 18–24 years, 25–39 years, and 40+ years) and residential municipality was recoded into two categories (large > 100.000 inhabitants, and small < 100.000 inhabitants). Three working situations were distinguished: not working [no job or own business or (most) work has come to standstill], working from home (mostly), and working on location (mostly). And five types of household were derived from type of persons participants were living with: alone, with partner/housemates only, with parents only (and any siblings), with children (and any partner or other persons), and other.
For tobacco, alcohol and cannabis prevalence rates were derived from number of use days per week. Responses of large amounts per day (sometimes up to hundreds) were not classified as invalid and deleted, but perceived as meaning “a lot” and maximized around the 97.5th percentile (80 cigarettes, 20 glasses and 20 joints). Days per week and amount per day were multiplied to derive weekly consumption. Number of other drug types used was derived by counting the number of positive answers to the multiple choice questions, excluding the “other drug” category.
After recoded and derived variables were created, a four-step analyses procedure was carried out.
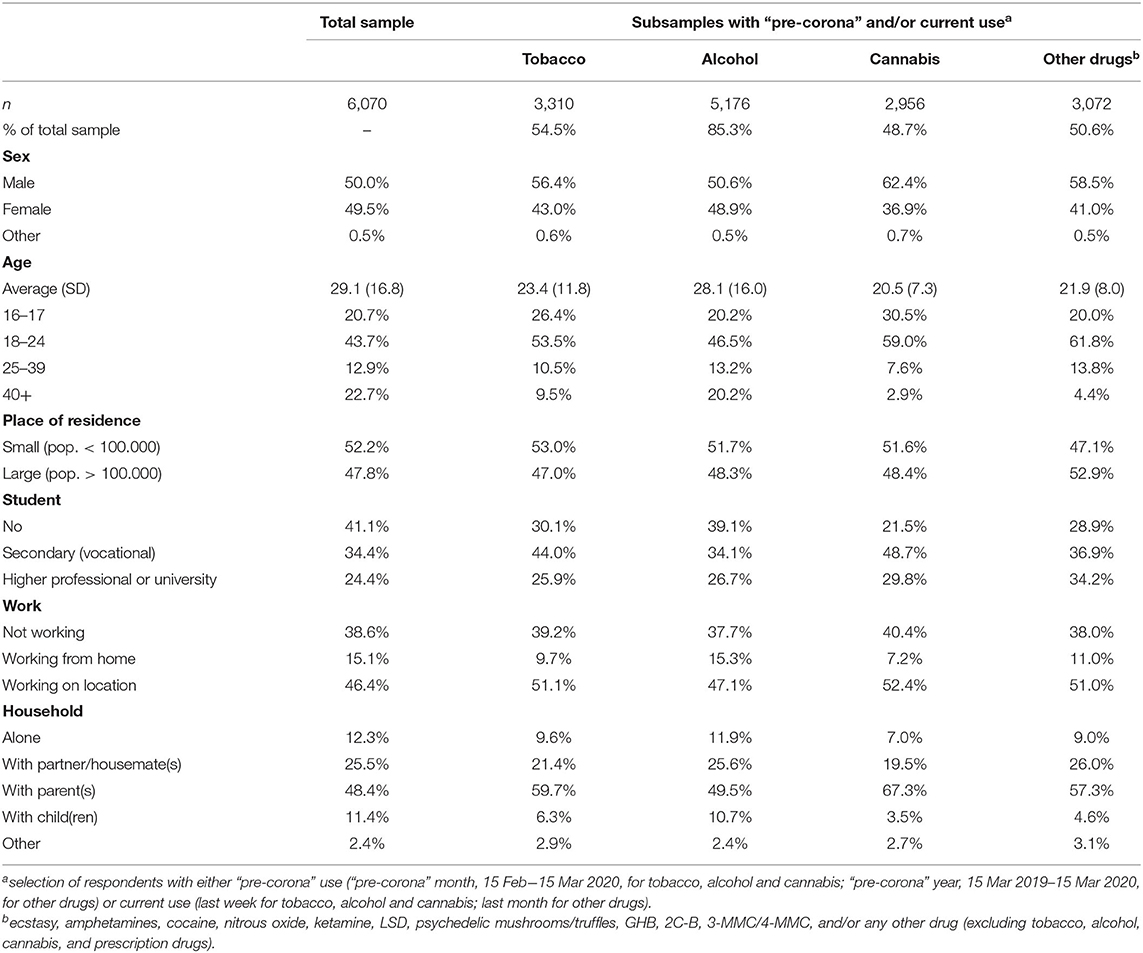
First, for each type of substance a selection was made of respondents with either current use or “pre-corona” use. Descriptive statistics were calculated for the total sample and the subsamples of selected respondents (Table 1).
Second, within the subsamples, “pre-corona” and current use were compared using McNemar tests for prevalence rates, and paired T-tests for average number of days, average amount per day and average weekly consumption (Table 2).
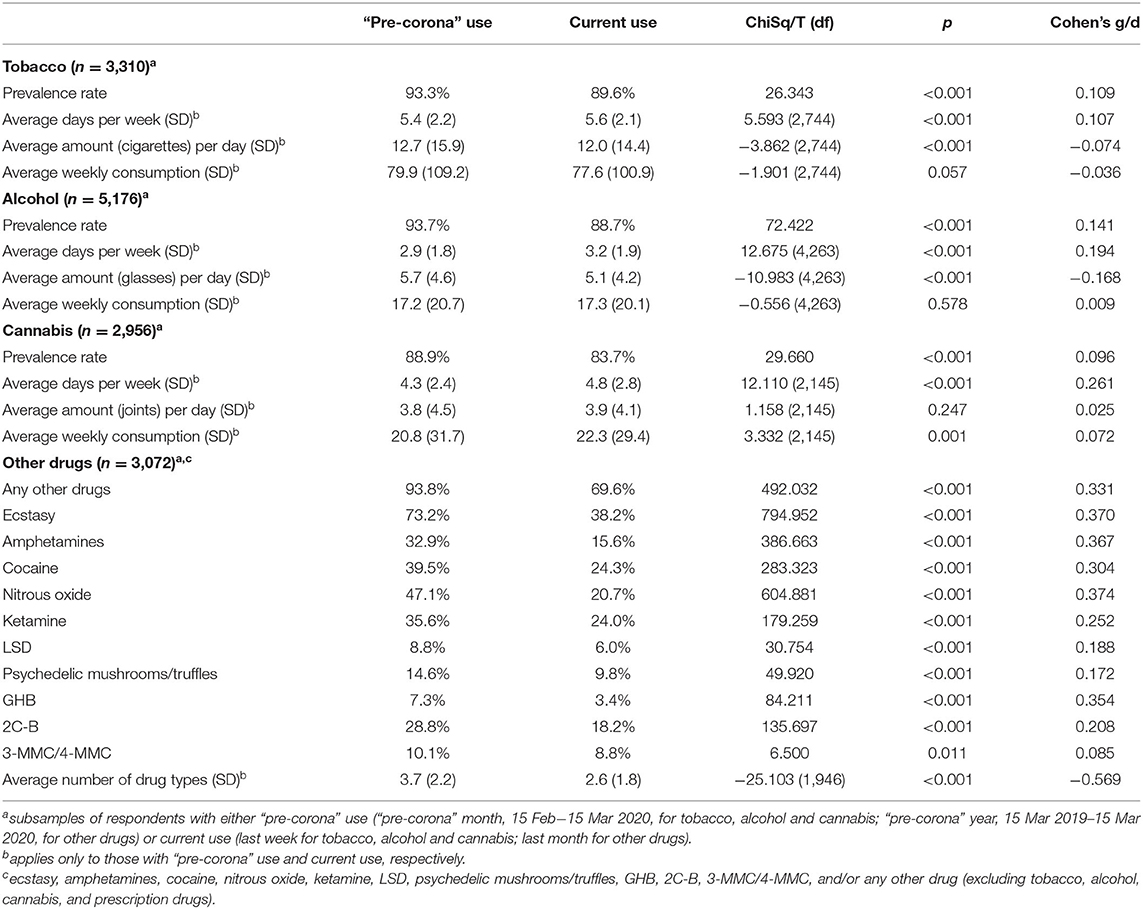
Table 2. “Pre-corona” and current use of tobacco, alcohol, cannabis, and other drugs (paired tests).
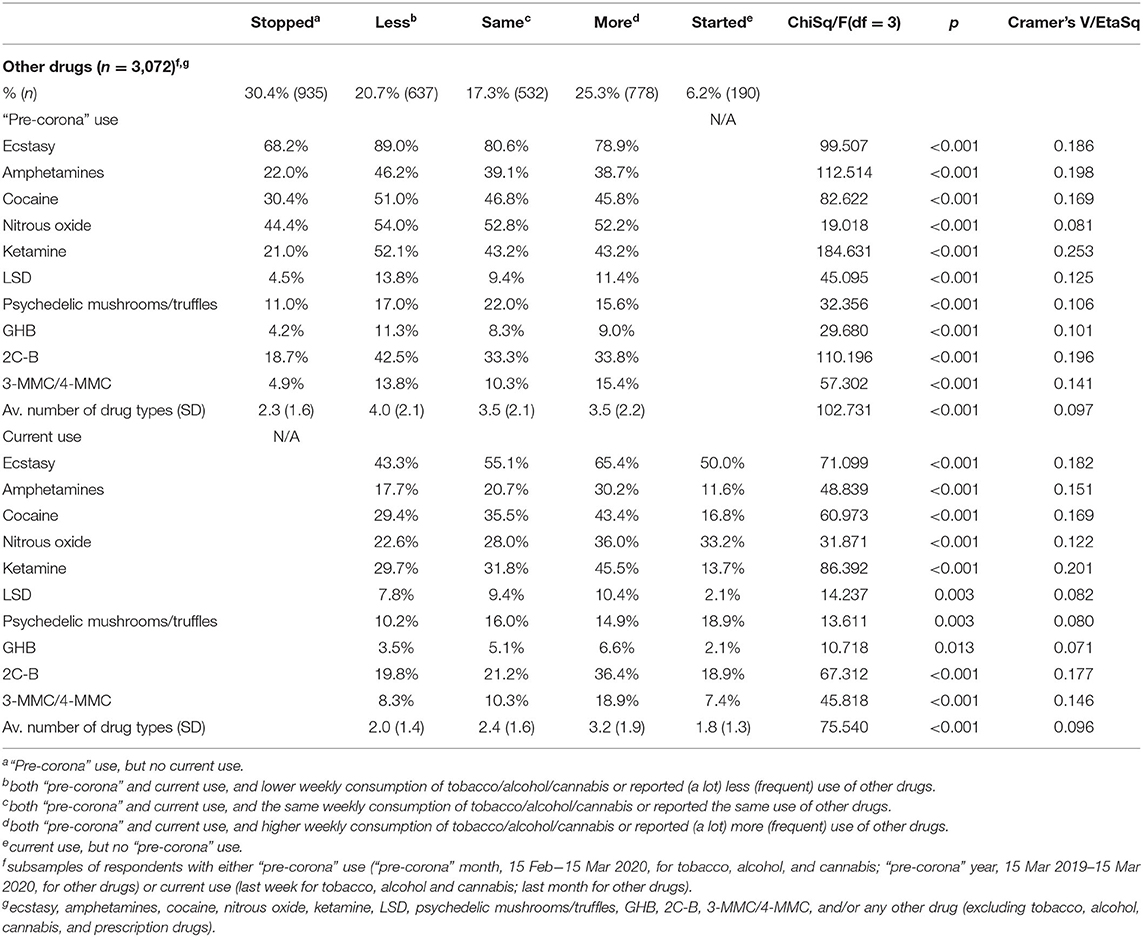
Third, five groups were identified within each subsample, based on the difference between “pre-corona” and current use: (1) Stopped: “Pre-corona” use, but no current use; (2) Less: Both “pre-corona” and current use, and lower weekly consumption of tobacco/alcohol/cannabis or reported (a lot) less (frequent) use of other drugs; (3) Same: Both “pre-corona” and current use, and the same weekly consumption of tobacco/alcohol/cannabis or reported the same use of other drugs; (4) More: Both “pre-corona” and current use, and higher weekly consumption of tobacco/alcohol/cannabis or reported (a lot) more (frequent) use of other drugs; and (5) Started: Current use, but no “pre-corona” use. “Pre-corona” and current use were compared across these five groups using ChiSq and ANOVA tests (Tables 3A,B).
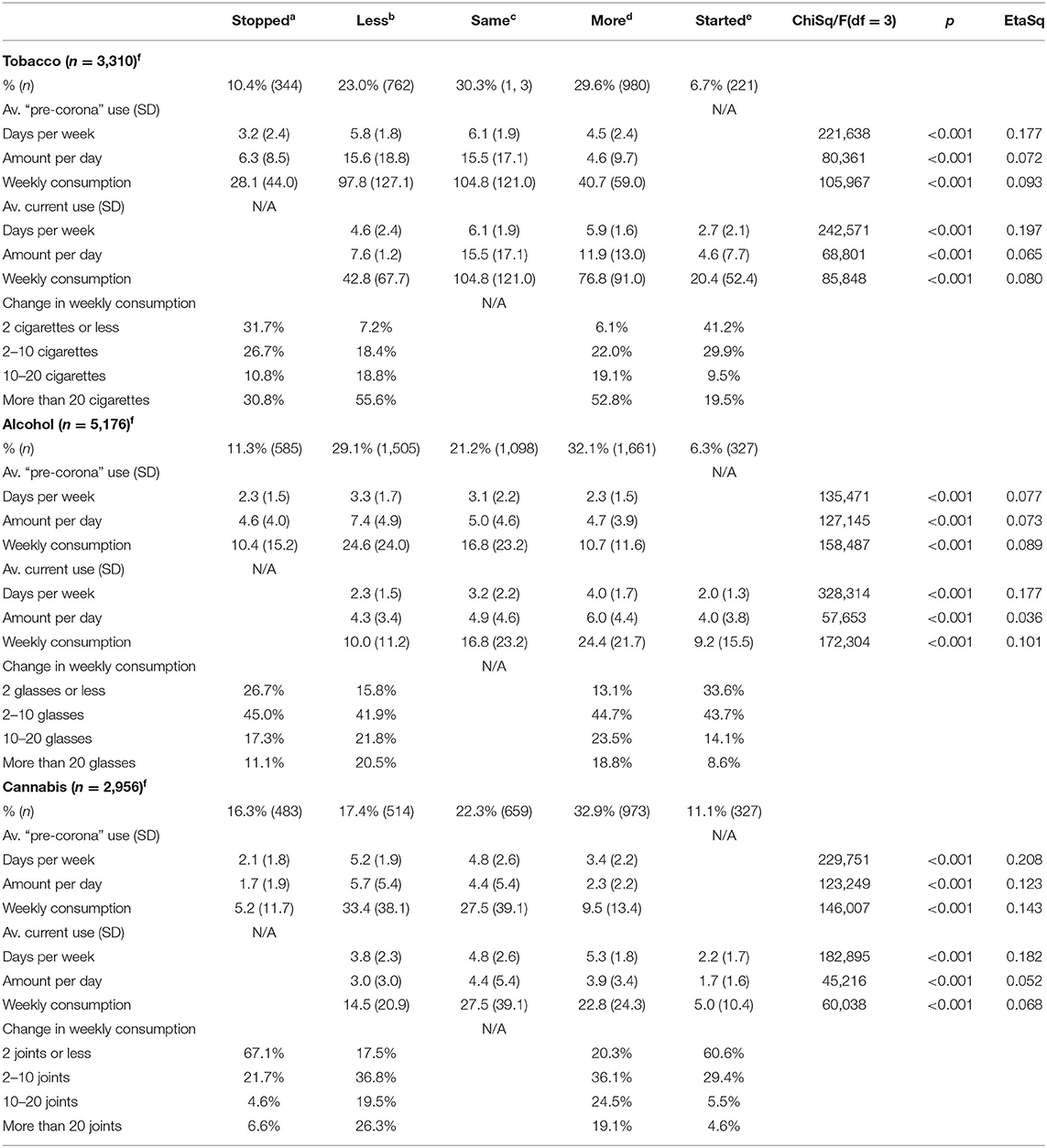
Table 3A. Change in the use of tobacco, alcohol and cannabis—current use compared to “pre-corona” use.
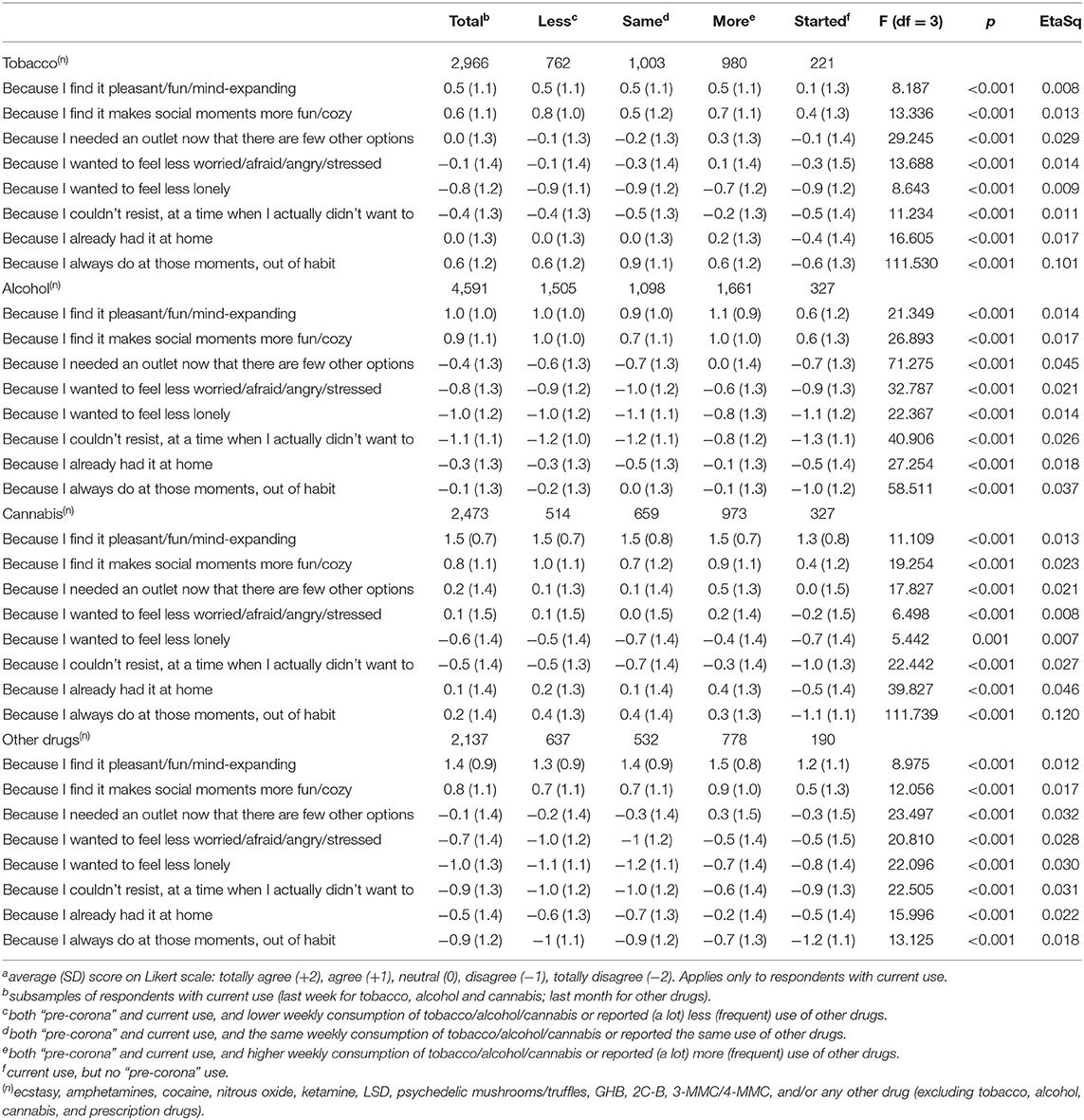
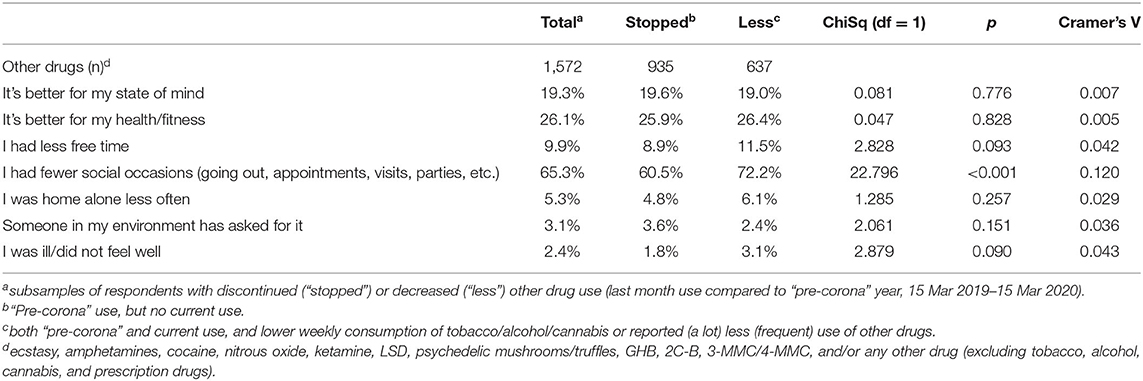
Fourth, associations between change in use and demographic characteristics (Supplementary Tables 1–4), reasons for current use (Table 4) and reasons for discontinued/decreased use (Table 5) were examined using ChiSq and ANOVA tests. When comparing demographics, the “other” category for sex and household were omitted from analyses. When comparing reasons for current use, respondents without current use (“stopped”) were omitted from analyses. The latter analyses were limited to respondents with discontinued (“stopped”) or decreased (“less”) use of other drugs.
Overall model results are presented (no pairwise post-hoc tests were computed). Analyses were carried out using IBM SPSS Statistics 25.
Results
Table 1 shows numbers and characteristics of the total sample and subsamples of respondents with “pre-corona” and/or current use of tobacco, alcohol, cannabis and other drugs. The majority of respondents use alcohol; the subsamples of those using tobacco, cannabis and other drugs comprise about half of the total sample. In the total sample males and females, and respondents from both small and large municipalities are equally divided, while males make up a (small) majority in the subsamples. Both the total sample and subsamples consist for a large part of young adults (18–24 years) and students living with parents. This is especially true for subsamples of respondents who use tobacco, cannabis and other drugs; a little less so for the subsample of respondents who use alcohol. As far as respondents have a job or own a business, they mostly work on location and not from home.
Within all subsamples current prevalence rates are lower compared to “pre-corona” (Table 2). Those who indicated continued use of tobacco and alcohol consumed increased in frequency (tobacco: from 5.4 to 5.6 days per week; alcohol from 2.9 to 3.2 days per week), but decreased in amounts (tobacco: from 12.7 to 12.0 cigarettes per day; alcohol: from 5.7 to 5.1 glasses per day), so that the average weekly consumption remained the same. Those continuing to use cannabis also increased their frequency of use (from 4.3 to 4.8 days per week), but did not change the amount. Average weekly consumption of cannabis therefore increased from 20.8 to 22.3 joints per week. Within the category of other drugs, ecstasy and nitrous oxide showed the most prominent decline in use. Respondents with both “pre-corona” and current drug use narrowed their drugs palette and used fewer different types of drugs (from 3.7 to 2.6 drug types on average).
While current overall prevalence rates in the subsamples were either lower than or similar to “pre-corona,” Tables 3A,B show that there are also respondents with increased use, including those who did not use in the “pre-corona” period but currently do. The latter group (“started”) formed around 6% of the subsamples of respondents who used tobacco, alcohol and other drugs, and 11.1% for cannabis.
Respondents who started using tobacco, alcohol and cannabis since the coronavirus measures came into effect do so less frequently and in smaller amounts than those already using (Table 3A). Almost a third of respondents using tobacco (29.6%), alcohol (32.1%), and cannabis (32.9%) smoked and drank more than “pre-corona” (“more”) and increased both frequency and amount of use, amounting to about a doubling of the weekly consumption. In some cases the total increase is limited to 2 cigarettes/glasses/joints per week, but there are also those who show a substantial increase in weekly consumption of more than 20 cigarettes/glasses/joints. Conversely, respondents using less tobacco (23.0%), alcohol (29.1%), and cannabis (17.4%) (“less”) reduced both frequency and quantity, cutting the average weekly consumption in half. Notably, these respondents with decreased use show the highest “pre-corona” weekly consumption of alcohol (average 24.6 glasses) and cannabis (average 33.4 joints), and the second highest weekly tobacco consumption (average 97.8 cigarettes). Those who stopped using tobacco (10.4%), alcohol (11.3%), and cannabis (16.3%) since the coronavirus measures came into effect (“stopped”) showed less extensive “pre-corona” consumption patterns. Current consumption of tobacco and cannabis was highest among respondents with unchanged use (“same”); current alcohol use was heaviest among those with increased use (“more”).
Compared to tobacco, alcohol and cannabis, a larger proportion of respondents stopped using other drugs (“stopped” 30.4%) (Table 3B). These respondents showed a less extensive pattern of “pre-corona” use compared to respondents with continued use (2.3 compared to 3.5–4.0 drug types on average). In fact, many used no more than one type of drug before the coronavirus measures came into effect, mostly ecstasy or nitrous oxide. Respondents reporting decreased (but continued) other drug use (“less”) reduced the number of drug types used from 4.0 to 2.0 on average [paired T(df) = −27.020(636), p <0.001, Cohen's d = −1.071]. Markedly, respondents reporting increased use (“more”) also showed a reduction in the number of drug types used [from 3.5 to 3.2, T(df) = −5.259(777), p ≤ 0.001, Cohen's d = −0.189]. Moreover, current prevalence rates were lower than “pre-corona” rates for ecstasy (65.4% vs. 78.9%, McNemar paired ChiSq = 45.255, p ≤ 0.001, Cohen's g = 0.220), amphetamines (30.2 vs. 38.7%, ChiSq = 24.006, p ≤ 0.001, Cohen's g = 0.188), nitrous oxide (36.0 vs. 52.2%, ChiSq = 73.703, p ≤ 0.001, Cohen's g = 0.297) and GHB (6.6 vs. 9.0%, ChiSq = 7.200, p = 0.007, Cohen's g = 0.211), and only higher for 3-MMC/4-MMC (18.9 vs. 15.4%, ChiSq = 8.557, p = 0.003, Cohen's g = 0.171).
Associations between change in use and demographic characteristics varied between types of substance. For alcohol, increased use was relatively more common among adults (25–39 years) and decreased use relatively more common among young adults (18–24 years). For other drugs, however, the opposite was true. Supplementary Material about demographic characteristics associated with changing patterns in substance use is available for professionals seeking input for tailored prevention.
Regardless of change in substances use, the most endorsed reason for current use of alcohol, cannabis or other drugs was either “Because I find it pleasant/fun/mind-expanding” or “Because I find it makes social moments more fun/cozy” (Table 5). Tobacco was often used out of habit. On face value, this seemed especially true for those with unchanged use (“same” average score 0.9, compared to −0.6 to 0.6 in other four groups). Respondents with unchanged use of alcohol also seemed to report habitual use more often than the other groups (0.0, compared to −0.1 to −1.0). Those with increased use of tobacco, alcohol, cannabis or other drugs (“more”) showed relatively high scores for the other reasons of use (“I needed an outlet…”, “I wanted to feel less worried…”, “I wanted to feel less lonely,” “I couldn't resist…”, and “I already had it at home”).
Having fewer social occasions than “pre-corona” was the most important reason to discontinue or decrease other drug use (65.3%), followed by physical (26.1%), and mental (19.3%) health. Overall, those who reduced their use of other drugs and those who had stopped using altogether reported similar reasons for doing so, but lack of social occasions was endorsed more often by respondents with decreased other drug use.
Discussion
This paper is based on data from a survey about “pre-corona” (before measures combatting the coronavirus pandemic came into effect in March 2020) and current substance use among Dutch respondents aged 16 years and older recruited through online channels. The survey was set up as a monitoring tool, using a short questionnaire and a convenience sample, to provide descriptive results for prevention practice.
The total sample was divided into subsamples of 3,310 respondents who had smoked tobacco either during the “pre-corona” month or last week, 5,176 respondents who had drank alcohol, 2,956 respondents who had used cannabis, and 3,072 respondents who had used other drugs (e.g., ecstasy, amphetamines, cocaine, nitrous oxide) in the “pre-corona” year or last month. Within these subsamples, overall results showed declined use compared to “pre-corona.” However, overall figures mask underlying variation in changing patterns, including discontinued (tobacco 10.4%, alcohol 11.3%, cannabis 16.3%, other drugs 30.4%), decreased (tobacco 23.0%, alcohol 29.1%, cannabis 17.4%, other drugs 20.7%), unchanged (tobacco 30.3%, alcohol 21.2%, cannabis 22.3%, other drugs 17.3%), increased (tobacco 29.6%, alcohol 32.1%, cannabis 32.9%, other drugs 25.3%), and (re)commenced use (tobacco 6.7%, alcohol 6.3%, cannabis 11.1%, other drugs 6.2%). Others have also found both less and more substance use following enforcement of coronavirus measures (12–16, 20–27, 29, 38). The two opposite scenarios Rehm et al. (10) predicted from literature and a review of the effects of past economic crises on alcohol consumption, one with increased and one with decreased use, apparently co-exist and also pertain to other substances. These results inform prevention practice about differential effects of corona measures on substance use that are masked by population trend curves, as the effects of opposite patterns of increased and decreased use cancel each other out.
Discontinued use was found to be much more common for other drugs than for tobacco, alcohol and cannabis, but for all substance types applied that those who stopped using showed less extensive “pre-corona” consumption patterns. Notably, the groups with decreased use showed relatively high levels of “pre-corona” use. This finding contradicts other studies who reported heavier pre-pandemic drinking patterns among respondents with increased alcohol use (13, 20). In this study, increased use of any of the substances was not associated with heavier “pre-corona” use. Current consumption of tobacco and cannabis was highest for respondents with unchanged use, while respondents with increased use showed most extensive current use of alcohol and other drugs, although the latter group did show lower prevalence rates for ecstasy, amphetamines, nitrous oxide and GHB. Respondents having taken up substance use (again) after the coronavirus measures came into effect showed less extensive current consumption patterns compared to the other groups.
Associations between change in use and demographic characteristics varied between types of substance, indicating for instance that different age groups are at risk for increased use of alcohol and other drugs. This underlines the need for tailored prevention targeting specific populations for specific substances. Associations between change in use and reasons for current use showed a consistent pattern across different substances. All substances, regardless of change in use, were often used for pleasure and social reasons. In fact, the lack of social occasions was reported as the main reason for discontinued and decreased other drug use. But respondents with increased use of tobacco, alcohol, cannabis and other drugs were also more likely to report additional reasons for use, in particular needing an outlet and wanting to feel less worried/afraid/angry/stressed or lonely. These reasons can be seen as coping motives, which have been linked to problematic use of alcohol [e.g., (39)], cannabis [e.g., (40)], and ecstasy [e.g., (41)] in general, and have more specifically been found to mediate the link between stressors (having children at home, depression, social connectedness, income loss, and living alone) and alcohol-related problems during the coronavirus pandemic (42). This is perhaps the most important finding from a prevention point of view.
In this paper, we looked at changes in the use of tobacco, alcohol, cannabis and other drugs separately. Further analyses, taking into account combined use, should reveal whether the groups with increased or decreased use overlap, or whether there are also groups in which decreased use of one type of substance is associated with increased use of another.
Another further exploration of the data would be to study changing patterns across time. Short-term changes immediately after the measures came into effect may differ from long-term changes after months of restrictions and accumulating socio-economic consequences. In addition, government measures varied with infection rates over time. In fact, on 14 October 2020 (the day after survey data for this paper was extracted) a new “partial lockdown” was enforced, that has been tightened into a “hard lockdown” since 14 December 2020 (while the survey was still ongoing).
Limitations
Because of anonymity, it cannot be ascertained that the sample consist of unique individuals. A selection was made of respondents who answered negatively to the question whether they had previously participated. The chance of duplication is estimated to be small because no incentives were given and there was nothing to gain by filling out the questionnaire for the second or subsequent time and lying about it.
This study cannot claim optimal generalizability due to under-coverage and self-selection inherent to web surveys (43). Substance use is over-represented in the total sample (tobacco 54.5%, alcohol 85.3%, cannabis 48.7%, other drugs 50.6%) when compared to the general Dutch population (tobacco 22.4%, alcohol 80.4%, cannabis 7.5%, ecstasy 2.8%, amphetamines 1.1%, cocaine 1.6%, nitrous oxide 2.7%) (44), and even subsamples of respondents who use these substances may not be representative of populations of users. Because of under-coverage some groups of users will be insufficiently presented in our sample (e.g., elderly or marginalized users), while self-selection may have caused our sample to be skewed toward young users who have experienced changing consumption patterns. Furthermore, the sample studied is relatively young (mainly 16–24 years). In this age group personality and brain development is still in process, and both are of significant influence on substance use trajectories (45). Proportion sizes of discontinued, decreased, unchanged, increased and (re)commenced use can therefore not be extrapolated to absolute figures for the general population.
To limit questionnaire length, detailed information on frequency and amount of use was not collected for drugs other than tobacco, alcohol and cannabis. Changing patterns in the use of other drugs is therefore based on self-report rather than objective measures. When asked if using more or less drugs than “pre-corona” the reference time frame was the “pre-corona” year (15 March 2019–15 March 2020), but respondents may have reflected on the time directly preceding the coronavirus measures. This period is “slow season” for music festivals (29–53 per month in Jan-Mar 2019; 118–174 per month in Apr-Sep 2019) (46), which are often preferred settings for drugs like ecstasy and nitrous oxide. Compared to that time, any drug use after the coronavirus measures came into effect could have felt like an increase in the respondents' minds. This may explain why respondents reported increased use of other drugs that could not be corroborated with increased prevalence rates. Measuring change in other drug use in a single question also impedes the ability to examine more complex patterns like selection (choosing a particular drug to use or quit) or substitution (replacing one drug with another).
Finally, some remarks about the definition of changing patterns. This was based on the frequency and amount of use in two relatively short periods for tobacco, alcohol and cannabis (“pre-corona” month and last week). Neither of these periods may have reflected “typical” consumption patterns and any absence of use may be “coincidental.” Discontinued use (defined as “pre-corona” use, but no last week use), for instance, may also include incidental (non-weekly) use and does not necessarily imply that there has not been any use since the coronavirus measures came into effect. Furthermore, increased and decreased use was derived from the difference in weekly consumption. In some cases differences were limited to only a few cigarettes/glasses/joints per week. For one person a small decrease in substance use may imply a clinically relevant risk level reduction, while for another a large decrease may not affect risk level outcome. For example, a female decreasing weekly consumption from 15 to 13 glasses will thereby fall below the threshold of excessive drinking, defined as more than 14 glasses a week for females in the Netherlands (44), while for a female decreasing weekly consumption from 25 to 15 glasses the end point will not fall below the threshold and the risk level outcome will remain that of excessive drinking. The current classification of changing patterns does not discern between these two examples and both are assigned to the “less” group. The aim of this paper was to explore different patterns of change in substance use. A more comprehensive examination of decreased or increased use may take different end points in terms of amount and frequency into account, but the survey did not measure any functional outcomes (e.g., health or use-related problems).
Conclusion
People show varying changing patterns of substance use since social distancing and other measures combatting the coronavirus came into effect. Some are using more than “pre-corona,” some are using less, and others are currently not using at all. Especially the use of drugs like ecstasy and nitrous oxide was discontinued or decreased due to the lack of social occasions for use. Those who increased their intake of tobacco, alcohol, cannabis or other drugs are more likely to report coping motives for use.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
AB contributed to the study design, questionnaire development, analysis, interpretation, and wrote the manuscript. FB contributed to the study design, interpretation, and assisted in drafting and reviewing the manuscript. JN contributed to the study design, questionnaire development, coordination of data collection, and assisted in drafting and reviewing the manuscript. All authors agree to be accountable for the content of the work and provided approval of the manuscript.
Funding
This study was funded from an annual grant from the municipality of Amsterdam to Jellinek Prevention as part of a structural monitoring effort. Jellinek Prevention commissioned the Amsterdam University of Applied Science to conduct the survey as part of the Antenna Amsterdam monitor.
Conflict of Interest
AB is employed by the Amsterdam University of Applied Science, a public knowledge institution offering higher professional education. FB and JN are employed by Arkin, a non-profit organization for mental health and addiction care. The authors declare that this study was funded from an annual grant from the municipality of Amsterdam as part of a structural monitoring effort. The funder was not involved in the study design, collection, analysis, interpretation of data, the writing of this article or the decision to submit it for publication.
Acknowledgments
The authors acknowledge the member organizations of Verslavingskunde Nederland (Dutch Addiction Association) for their recruitment efforts, and thank Tom Bart (Jellinek Prevention), Anneke Goudriaan (Arkin), and Jannet de Jonge (Amsterdam University of Applied Science) for commenting on the draft manuscript.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2021.633551/full#supplementary-material
References
1. Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. (2020) 395:912–20. doi: 10.1016/S0140-6736(20)30460-8
2. Galea S, Merchant RM, Lurie N. The mental health consequences of COVID-19 and physical distancing: the need for prevention and early intervention. JAMA Intern Med. (2020) 180:817–8. doi: 10.1001/jamainternmed.2020.1562
3. Balanzá-Martínez V, Atienza-Carbonell B, Kapczinski F, De Boni RB. Lifestyle behaviours during the COVID-19 - time to connect. Acta Psychiatr Scand. (2020) 141:399–400. doi: 10.1111/acps.13177
4. Clay J, Parker M. Alcohol use and misuse during the COVID-19 pandemic: a potential public health crisis? Lancet Public Health. (2020) 5:e259. doi: 10.1016/S2468-2667(20)30088-8
5. McKay D, Asmundson G. COVID-19 stress and substance use: current issues and future preparations. J Anxiety Disord. (2020) 74:102274. doi: 10.1016/j.janxdis.2020.102274
6. Mallet J, Dubertret C, Le Strat Y. Addictions in the COVID-19 era: current evidence, future perspectives a comprehensive review. Prog Neuropsychopharmacol Biol Psychiatry. (2020) 106:110070. doi: 10.1016/j.pnpbp.2020.110070
7. Patwardhan P. COVID-19: Risk of increase in smoking rates among England's 6 million smokers and relapse among England's 11 million ex-smokers. BJGP Open. (2020) 4:bjgpopen20X101067. doi: 10.3399/bjgpopen20X101067
8. Ramalho R. Alcohol consumption and alcohol-related problems during the COVID-19 pandemic: a narrative review. Australas Psychiatry. (2020) 28:524–6. doi: 10.1177/1039856220943024
9. Zaami S, Marinelli E, Varì M. New trends of substance abuse during COVID-19 pandemic: an international perspective. Front Psychiatry. (2020) 11:700. doi: 10.3389/fpsyt.2020.00700
10. Rehm J, Kilian C, Ferreira-Borges C, Jernigan D, Monteiro M, Parry C, et al. Alcohol use in times of the COVID 19: implications for monitoring and policy. Drug Alcohol Rev. (2020) 39:301–4. doi: 10.1111/dar.13074
11. Wei Y, Shah R. Substance use disorder in the COVID-19 pandemic: a systematic review of vulnerabilities and complications. Pharmaceuticals. (2020) 13:155. doi: 10.3390/ph13070155
12. Avery AR, Tsang S, Seto EYW, Duncan E. Stress, anxiety, and change in alcohol use during the COVID-19 pandemic: findings among adult twin pairs. Front Psychiatry. (2020) 11:1030. doi: 10.3389/fpsyt.2020.571084
13. Chodkiewicz J, Talarowska M, Miniszewska J, Nawrocka N, Bilinski P. Alcohol consumption reported during the COVID-19 pandemic: the initial stage. Int J Environ Res Public Health. (2020) 17:4677. doi: 10.3390/ijerph17134677
14. Kim JU, Majid A, Judge R, Crook P, Nathwani R, Selvapatt N, et al. Effect of COVID-19 lockdown on alcohol consumption in patients with pre-existing alcohol use disorder. Lancet Gastroenterol Hepatol. (2020) 5:886–7. doi: 10.1016/S2468-1253(20)30251-X
15. Klemperer EM, West JC, Peasley-Miklus C, Villanti AC. Change in Tobacco and electronic cigarette use and motivation to quit in response to COVID-19. Nicotine Tob Res. (2020) 22:1662–3. doi: 10.1093/ntr/ntaa072
16. Malta DC, Szwarcwald CL, Barros MBA, Gomes CS, Machado ÍE, Souza Júnior PRB, et al. The COVID-19 Pandemic and changes in adult Brazilian lifestyles: a cross-sectional study. Epidemiol Serv Saude. (2020) 29:e2020407. doi: 10.1590/S1679-49742020000400026
17. McPhee MD, Keough MT, Rundle S, Heath LM, Wardell JD, Hendershot CS. Depression, environmental reward, coping motives and alcohol consumption during the COVID-19 pandemic. Front Psychiatry. (2020) 11:574676. doi: 10.3389/fpsyt.2020.574676
18. Lechner W, Laurene K, Patel S, Anderson M, Grega C, Kenne D. Changes in alcohol use as a function of psychological distress and social support following COVID-19 related University closings. Addict Behav. (2020) 110:106527. doi: 10.1016/j.addbeh.2020.106527
19. López-Bueno R, Calatayud J, Casaña J, Casajús JA, Smith L, Tully MA, et al. COVID-19 confinement and health risk behaviors in Spain. Front Psychol. (2020) 11:1426. doi: 10.3389/fpsyg.2020.01426
20. Neill E, Meyer D, Toh W, Rheenen T, Phillipou A, Tan E, et al. Alcohol use in Australia during the early days of the COVID−19 pandemic: initial results from the COLLATE project. Psychiatry Clin Neurosc. (2020) 74:542–9. doi: 10.1111/pcn.13099
21. Scarmozzino F, Visioli F. Covid-19 and the subsequent lockdown modified dietary habits of almost half the population in an Italian sample. Foods. (2020) 9:675. doi: 10.3390/foods9050675
22. Siddiqi K, Siddiqui F, Khan A, Ansaari S, Kanaan M, Khokhar M, et al. The impact of COVID-19 on smoking patterns in Pakistan: findings from a longitudinal survey of smokers. Nicotine Tob Res. (2020) 23:765–9. doi: 10.1093/ntr/ntaa207
23. Sidor A, Rzymski P. Dietary choices and habits during COVID-19 lockdown: experience from Poland. Nutrients. (2020) 12:1657. doi: 10.3390/nu12061657
24. Stanton R, To QG, Khalesi S, Williams SL, Alley SJ, Thwaite TL, et al. Depression, anxiety and stress during COVID-19: associations with changes in physical activity, sleep, tobacco and alcohol use in australian adults. Int J Environ Res Public Health. (2020) 17:4065. doi: 10.3390/ijerph17114065
25. Dumas T, Ellis W, Litt D. What does adolescent substance use look like during the COVID-19 pandemic? examining changes in frequency, social contexts, and pandemic-related predictors. J Adolesc Health. (2020) 67:354–61. doi: 10.1016/j.jadohealth.2020.06.018
26. Rolland B, Haesebaert F, Zante E, Benyamina A, Haesebaert J, Franck N. Global changes and factors of increase in caloric/salty food intake, screen use, and substance use during the early COVID-19 containment phase in the general population in france: survey study. JMIR Public Health Surveill. (2020) 6:e19630. doi: 10.2196/19630
27. Sharma P, Ebbert JO, Rosedahl JK, Philpot LM. Changes in substance use among young adults during a respiratory disease pandemic. SAGE Open Med. (2020) 8:2050312120965321. doi: 10.1177/2050312120965321
28. Tucker JS, D'Amico EJ, Pedersen ER, Garvey R, Rodriguez A, Klein DJ. Behavioral health and service usage during the coronavirus disease 2019 pandemic among emerging adults currently or recently experiencing homelessness. J Adolesc Health. (2020) 67:603–5. doi: 10.1016/j.jadohealth.2020.07.013
29. Vanderbruggen N, Matthys F, Van Laere S, Zeeuws D, Santermans L, Van den Ameele S, et al. Self-reported alcohol, tobacco, and cannabis use during COVID-19 lockdown measures: results from a web-based survey. Eur Addict Res. (2020) 26:309–15. doi: 10.1159/000510822
30. University of Antwerp. COVID-19 International Student Well-being Study. Available online at: https://www.uantwerpen.be/en/research-groups/centre-population-family-health/research2/covid-19-internation/ (accessed November 23, 2020).
31. Rogers AH, Shepherd JM, Garey L, Zvolensky MJ. Psychological factors associated with substance use initiation during the COVID-19 pandemic. Psychiatry Res. (2020) 293:113407. doi: 10.1016/j.psychres.2020.113407
32. European Monitoring Centre for Drugs and Drug Addiction. Impact of COVID-19 on Patterns of Drug Use and Drug-Related Harms in Europe, EMCDDA Trendspotter Briefing. Luxembourg: Publications Office of the European Union (2020). p. 27.
33. Palamar JJ, Le A, Acosta P. Shifts in drug use behavior among electronic dance music partygoers in New York During COVID-19 social distancing. Subst Use Misuse. (2021) 56:238–44. doi: 10.1080/10826084.2020.1857408
34. Kissler SM, Tedijanto C, Goldstein E, Grad YH, Lipsitch M. Projecting the transmission dynamics of SARS-CoV-2 through the post-pandemic period. Science. (2020) 368:860–8. doi: 10.1126/science.abb5793
35. Hogeschool van Amsterdam. Antenne Amsterdam. Available online at: https://hva.nl/antenne-amsterdam (accessed November 23, 2020).
36. European Monitoring Centre for Drugs and Drug Addiction. Monitoring Drug Use in Recreational Settings Across Europe: Conceptual Challenges and Methodological Innovations. Luxembourg: Publications Office of the European Union (2018). p. 42.
37. Barratt MJ, Ferris JA, Zahnow R, Palamar JJ, Maier LJ, Winstock AR. Moving on from representativeness: testing the utility of the global drug survey. Subst Abuse. (2017) 11:1–17. doi: 10.1177/1178221817716391
38. Stathopoulou T, Mouriki A, Papaliou O. Student Well-Being During the COVID-19 Pandemic in Greece: Results From the C19 ISWS Survey. Athens: National Centre for Social Research (EKKE) (2020). p. 82.
39. Kuntsche E, Knibbe R, Gmel G, Engels R. Why do young people drink? A review of drinking motives. Clin Psychol Rev. (2005) 25:841–61. doi: 10.1016/j.cpr.2005.06.002
40. Spradlin A, Cuttler C. Problems associated with using cannabis to cope with stress. Cannabis. (2019) 2:29–38. doi: 10.26828/cannabis.2019.01.003
41. Meikle S, Carter O, Bedi G. Individual differences in distress, impulsivity, and coping motives for use as predictors of problematic ecstasy use. Addict Behav. (2020) 108:106397. doi: 10.1016/j.addbeh.2020.106397
42. Wardell JD, Kempe T, Rapinda KK, Single A, Bilevicius E, Frohlich JR, et al. Drinking to cope during COVID-19 pandemic: the role of external and internal factors in coping motive pathways to alcohol use, solitary drinking, and alcohol problems. Alcohol Clin Exp Res. (2020) 44:2073–83. doi: 10.1111/acer.14425
43. Bethlehem J. Selection bias in web surveys. Int Stat Rev. (2010) 78:161–88. doi: 10.1111/j.1751-5823.2010.00112.x
44. Van Laar M, Cruts G, Van Miltenburg L, Strada L, Ketelaars T, Croes E, et al. Nationale Drug Monitor Jaarbericht 2019. Utrecht/Den Haag: Trimbos-instituut/WODC (2020). p. 582. Available online at: https://www.trimbos.nl/docs/2611d773-620a-45af-a9e5-c27a7e6688e4.pdf
45. Peeters M, Boendermaker WJ, Veltkamp RC, Oldehinkel AJ, Vollebergh WAM. Trajectories of alcohol and cannabis use from early to late adolescence and important determinants for intervention purposes. Alcohol Clin Exp Res. (2018) 42:227A. doi: 10.1111/acer.13748
46. Van Vliet H. Festival Atlas. Het Nederlandse Festivallandschap 2019 – Muziekfestivals. Deventer: Plan B publishers (2020). p. 62. Available online at: http://www.festivalatlas.nl/files/Festivalatlas2019_MUZIEK.pdf
Keywords: COVID-19, coronavirus, substance use, tobacco, alcohol, cannabis, drugs
Citation: Benschop A, van Bakkum F and Noijen J (2021) Changing Patterns of Substance Use During the Coronavirus Pandemic: Self-Reported Use of Tobacco, Alcohol, Cannabis, and Other Drugs. Front. Psychiatry 12:633551. doi: 10.3389/fpsyt.2021.633551
Received: 25 November 2020; Accepted: 27 April 2021;
Published: 26 May 2021.
Edited by:
Ornella Corazza, University of Hertfordshire, United KingdomReviewed by:
Marc Auriacombe, Université de Bordeaux, FranceHollis C. Karoly, Colorado State University, United States
Copyright © 2021 Benschop, van Bakkum and Noijen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Annemieke Benschop, w.j.benschop@hva.nl
 Annemieke Benschop
Annemieke Benschop Floor van Bakkum2
Floor van Bakkum2 Judith Noijen
Judith Noijen