Abstract
Purpose
High-dependency care units (HDUs) are a focus of research to optimize critical care resource allocation. HDUs provide a level of care between the general ward and the intensive care unit (ICU). However, few data report on the case mix and outcomes of patients in these units.
Methods
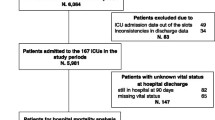
Retrospective observational cohort study of patients admitted to 11 stand-alone HDUs in the UK from 2008 to 2011. We stratified patients by location prior to HDU admission and location on discharge from HDU, and we summarized the case mix, transitions of care, and mortality.
Results
Of 9008 patients admitted to 11 stand-alone HDUs, 56.5 % were male and the mean age was 62.7 ± 17.9 years. The majority of patients admitted to HDUs were non-surgical (59.3 %), with 22.4 and 20.1 % admitted from the ICU and general ward, respectively; 41.3 % were admitted from the operating room or recovery suite. The median length of stay in HDU was 1.8 days (IQR 0.9–3.5) and in-HDU mortality was 5.1 %. Among HDU survivors (n = 8551), 8.5 % were discharged to an ICU, 80.9 % to a general ward, and 10.6 % to other care areas. For patients admitted to HDU from an ICU, only 5.8 % were readmitted to ICU. Hospital mortality for the HDU population was 14.8 %; for patients discharged to an ICU, hospital mortality was 43.6 %.
Conclusions
In a sample of 11 stand-alone HDUs in the UK, patients are from many different hospital locations. Hospital mortality for patients requiring HDU care is high, particularly for patients who require transfer to an ICU.

Similar content being viewed by others
References
Chaboyer W, James H, Kendall M (2005) Transitional care after the intensive care unit: current trends and future directions. Crit Care Nurse 25:16–28
Beard H (2005) Does intermediate care minimize relocation stress for patients leaving the ICU? Nurs Crit Care 10:272–278
Heller J, Murch P (2008) Development in service provision. Making major elective surgery happen. The development of a postoperative surgical unit. Nurs Crit Care 13:97–104
Prin M, Wunsch H (2014) The role of stepdown beds in hospital care. Am J Respir Crit Care Med 190:1210–1216
Wunsch H, Harrison DA, Jones A, Rowan K (2015) The impact of the organization of high-dependency care on acute hospital mortality and patient flow for critically ill patients. Am J Respir Crit Care Med 191:186–193
Corrado A, Roussos C, Ambrosino N, Confalonieri M, Cuvelier A, Elliott M, Ferrer M, Gorini M, Gurkan O, Muir JF, Quareni L, Robert D, Rodenstein D, Rossi A, Schoenhofer B, Simonds AK, Strom K, Torres A, Zakynthinos S (2002) Respiratory intermediate care units: a European survey. Eur Respir J 20:1343–1350
Capuzzo M, Volta C, Tassinati T, Moreno R, Valentin A, Guidet B, Iapichino G, Martin C, Perneger T, Combescure C, Poncet A, Rhodes A (2014) Hospital mortality of adults admitted to intensive care units in hospitals with and without intermediate care units: a multicentre European cohort study. Crit Care 18:551
Harrison DA, Brady AR, Rowan K (2004) Case mix, outcome and length of stay for admissions to adult, general critical care units in England, Wales and Northern Ireland: the Intensive Care National Audit and Research Centre Case Mix Programme Database. Crit Care 8:R99–111
Department of Health (2000) Comprehensive critical care: a review of adult critical care services. Department of Health, London, p 37. Available at: http://webarchive.nationalarchives.gov.uk/20130107105354/http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_4082872.pdf
Padkin A, Goldfrad C, Brady AR, Young D, Black N, Rowan K (2003) Epidemiology of severe sepsis occurring in the first 24 h in intensive care units in England, Wales, and Northern Ireland. Crit Care Med 31:2332–2338
Harrison DA, Welch CA, Eddleston JM (2006) The epidemiology of severe sepsis in England, Wales and Northern Ireland, 1996–2004: secondary analysis of a high quality clinical database, the ICNARC Case Mix Programme Database. Crit Care 10:R42
Harrison DA, Parry GJ, Carpenter JR, Short A, Rowan K (2007) A new risk prediction model for critical care: the Intensive Care National Audit and Research Centre (ICNARC) model. Crit Care Med 35:1091–1098
Goldfrad C, Rowan K (2000) Consequences of discharges from intensive care at night. Lancet 355:1138–1142
Renton J, Pilcher DV, Santamaria JD, Stow P, Bailey M, Hart G, Duke G (2011) Factors associated with increased risk of readmission to intensive care in Australia. Intensive Care Med 37:1800–1808
Lilly CM, Zuckerman IH, Badawi O, Riker RR (2011) Benchmark data from more than 240,000 adults that reflect the current practice of critical care in the United States. Chest 140:1232–1242
Chong JL, Pillai R, Fisher A, Grebenik C, Sinclair M, Westaby S (1992) Cardiac surgery: moving away from intensive care. Br Heart J 68:430–433
Armstrong K, Young J, Hayburn A, Irish B, Nikoletti S (2003) Evaluating the impact of a new high dependency unit. Int J Nurs Pract 9:285–293
Crosby DL, Rees GA (1983) Post operative care: the role of the high dependency unit. Ann R Coll Surg Engl 65:391–393
Peacock JE, Edbrooke DL (1995) Rationing intensive care. Data from one high dependency unit supports their effectiveness. BMJ 310:1413
Frieden J, Cooper JA (1976) The role of the intermediate cardiac care unit. JAMA 235:816–818
Cady N, Mattes M, Burton S (1995) Reducing intensive care unit length of stay. A stepdown unit for first-day heart surgery patients. J Nurs Adm 25:29–35
Bellomo R, Goldsmith D, Uchino S, Buckmaster J, Hart G, Opdam H, Silvester W, Doolan L, Gutteridge G (2005) A before and after trial of the effect of a high-dependency unit on post-operative morbidity and mortality. Crit Care Resusc 7:16–21
Confalonieri M, Gorini M, Ambrosino N, Mollica C, Corrado A, Scientific Group on Respiratory Intensive Care of the Italian Association of Hospital P (2001) Respiratory intensive care units in Italy: a national census and prospective cohort study. Thorax 56:373–378
Corrado A, Confalonieri M (1999) Respiratory high-dependency care units in Italy. Monaldi Arch Chest Dis 54:435–437
Junker C, Zimmerman JE, Alzola C, Draper EA, Wagner DP (2002) A multicenter description of intermediate-care patients: comparison with ICU low-risk monitor patients. Chest 121:1253–1261
Wunsch H, Angus DC, Harrison DA, Linde-Zwirble WT, Rowan KM (2011) Comparison of medical admissions to intensive care units in the United States and United Kingdom. Am J Respir Crit Care Med 183:1666–1673
Hutchings A, Durand MA, Grieve R, Harrison D, Rowan K, Green J, Cairns J, Black N (2009) Evaluation of modernisation of adult critical care services in England: time series and cost effectiveness analysis. BMJ 339:b4353
Jones HJ, Coggins R, Lafuente J, de Cossart L (1999) Value of a surgical high-dependency unit. Br J Surg 86:1578–1582
Jones DR, Copeland GP, de Cossart L (1992) Comparison of POSSUM with APACHE II for prediction of outcome from a surgical high-dependency unit. Br J Surg 79:1293–1296
McIlroy DR, Coleman BD, Myles PS (2006) Outcomes following a shortage of high dependency unit beds for surgical patients. Anaesth Intensive Care 34:457–463
Byrick RJ, Power JD, Ycas JO, Brown KA (1986) Impact of an intermediate care area on ICU utilization after cardiac surgery. Crit Care Med 14:869–872
Akkerman R, Knip M (2004) Reallocation of beds to reduce waiting time for cardiac surgery. Health Care Manag Sci 7:119–126
Hilton G, Madayag M, Shagoury C (1993) Development of a surgical/trauma intermediate care unit. Clin Nurse Spec 7:274–279
Lucena JF, Alegre F, Martinez-Urbistondo D, Landecho MF, Huerta A, Garcia-Mouriz A, Garcia N, Quiroga J (2013) Performance of SAPS II and SAPS 3 in intermediate care. PLoS One 8:e77229
Ip SP, Leung YF, Ip CY, Mak WP (1999) Outcomes of critically ill elderly patients: is high-dependency care for geriatric patients worthwhile? Crit Care Med 27:2351–2357
Alegre F, Landecho MF, Huerta A, Fernandez-Ros N, Martinez-Urbistondo D, Garcia N, Quiroga J, Lucena JF (2015) Design and performance of a new severity score for intermediate care. PLoS One 10:e0130989
Boots R, Lipman J (2002) High dependency units: issues to consider in their planning. Anaesth Intensive Care 30:348–354
Acknowledgments
We would like to thank the Case Mix Programme staff at Intensive Care National Audit and Research Centre (ICNARC) for the use of these data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Funding
Award Number K08AG038477 from the National Institute on Aging to Hannah Wunsch.
Additional information
Take-home message: In a sample of 11 HDUs in the UK, there was a mix of patients from many different hospital locations, with the majority being non-surgical. Hospital mortality for patients requiring HDU care was high, particularly for patients who required transfer to an ICU.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Prin, M., Harrison, D., Rowan, K. et al. Epidemiology of admissions to 11 stand-alone high-dependency care units in the UK. Intensive Care Med 41, 1903–1910 (2015). https://doi.org/10.1007/s00134-015-4011-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-015-4011-y